Newly Diagnosed Glioblastoma: A Review on Clinical Management
This review focuses on clinical developments and management of newly diagnosed glioblastoma, and includes a discussion about the incorporation of molecular features into the classification of this disease.
Oncology (Williston Park). 33(3):91-100.

Rimas V. Lukas, MD

Derek A. Wainwright, PhD

Erik Ladomersky, PhD

Sean Sachdev, MD

Adam M. Sonabend, MD
Roger Stupp, MD

Table 1. Clinical Trials Investigating Various Radiation Dosing Regimens
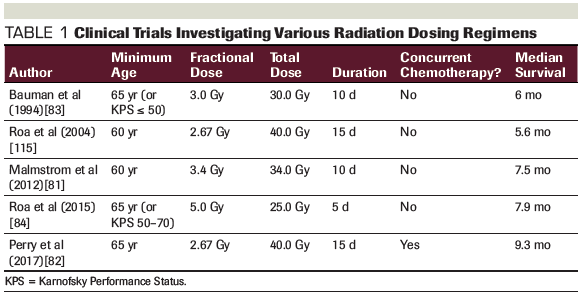
Table 2. Key Late-Phase Clinical Trials for Newly Diagnosed Glioblastoma
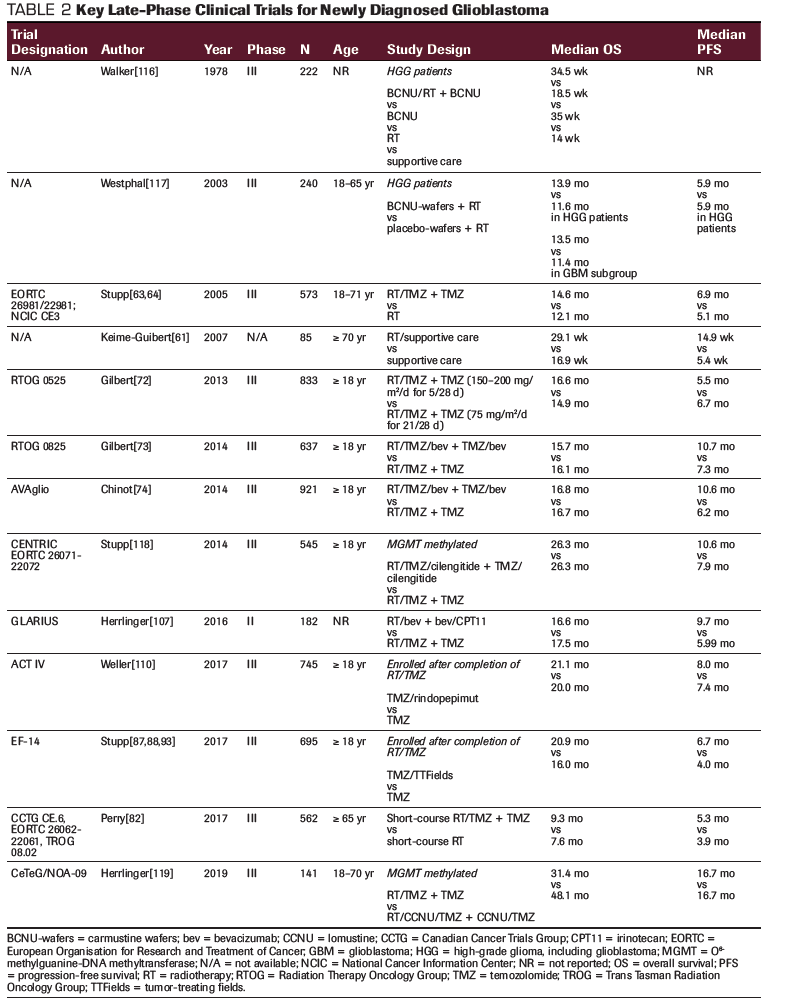
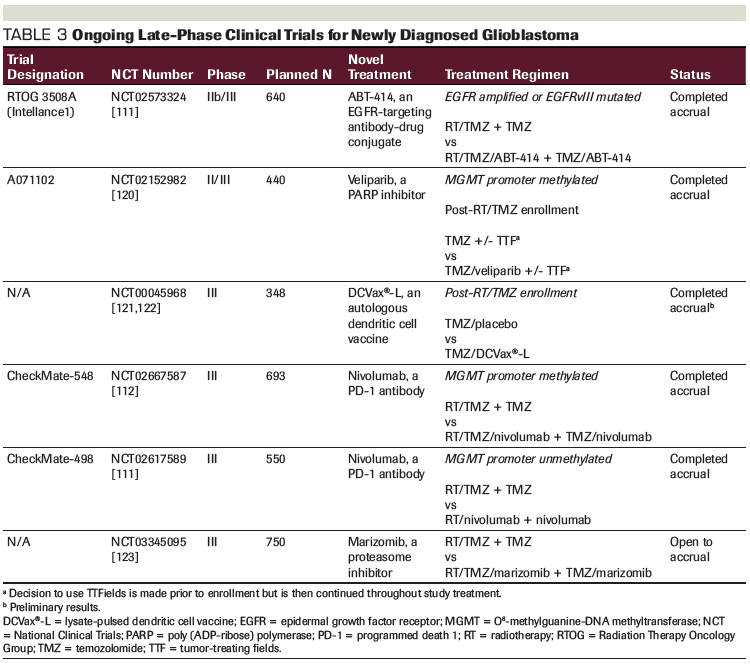
Table 3. Ongoing Late-Phase Clinical Trials for Newly Diagnosed Glioblastoma
Glioblastoma is an aggressive primary tumor of the central nervous system. This review will focus on clinical developments and management of newly diagnosed disease, including a discussion about the incorporation of molecular features into the classification of glioblastoma. Such advances will continue to shape our thinking about the disease and how to best manage it. With regards to treatment, the role of surgical resection, radiotherapy, chemotherapy, and tumor-treating fields will be presented. Pivotal studies defining our current standard of care will be highlighted, as will key ongoing trials that may influence our management of glioblastoma in the near future.
Click here to read an expert perspective from Nicholas Butowski, MD.
Introduction
Glioblastoma, previously known as glioblastoma multiforme, is the most aggressive among infiltrative gliomas, a group of primary tumors arising from the central nervous system (CNS). Patients with this cancer type face significant morbidity and mortality, with over 13,000 deaths per year in the United States. Recent advances in our biological understanding of gliomas have led to important and substantive changes in their classification, in the identification of prognostic and predictive molecular markers, and in the therapeutic management of newly diagnosed glioma.
Classification
The term ‘glioblastoma multiforme’ was introduced in the 1926 classification system devised by Cushing and Bailey.[1] ‘Multiforme,’ which refers to a heterogenous histologic appearance and proliferation of multiple cell types, was abandoned from the revised nomenclature in the 2007 World Health Organization Classification of Tumors of the Central Nervous System, and is now simply called ‘glioblastoma.’[2] Glioblastoma is histologically defined by neoplastic cells with astrocytic characteristics and the presence of either endothelial proliferation-often in a glomeruloid morphology-and/or necrosis, which may resemble a pseudopalisading pattern (a false fence of neoplastic cells surrounding an area of necrotic tissue).
Due to its aggressive and highly proliferative course, glioblastoma is considered a grade IV astrocytoma. Molecular characterization has allowed for further refinement of the condition’s classification and is now an integral part of the diagnosis of malignant glioma.[3] Patients are classified into one of two distinct categories based on the presence or absence of mutations in the IDH1 or IDH2 genes.
Primary glioblastoma/IDH wild-type glioblastoma
The majority of glioblastomas are IDH wild-type and correspond to the longstanding clinical description of primary glioblastomas, which arise rapidly from non-neoplastic brain cells and progress quickly. In addition, a subgroup of lower-grade gliomas may carry molecular features and signatures similar to glioblastoma, with a similarly aggressive natural course,[4] for which an intensive treatment strategy is advocated. These facts stress that a microscopic histologic diagnosis alone is insufficient to make informed and rational clinical decisions; therefore, it is essential that molecular alterations be integrated when diagnosing and managing glioma. This will potentially be of benefit in opening up appropriate clinical trial opportunities for this subset of patients in the future.[5]
Secondary glioblastoma/IDH-mutated glioblastoma
Up to 10% of patients with glioblastoma harbor a mutation in the IDH1 or IDH2 genes, an early event in gliomagenesis. Since these glioblastomas often arise from a prior lower-grade glioma, they are considered secondary glioblastomas. In the past, both primary and secondary glioblastomas were considered to be the same clinical entity. However, recent studies clearly indicate that IDH-mutated glioblastomas have a more protracted natural course. As such, secondary glioblastomas are to be classified as a distinct biological and molecular entity for which different treatment strategies will ultimately be proposed. Former series of long-term survivors are commonly enriched for patients with IDH-mutated tumors.[3]
Epidemiology
Primary CNS tumors represent only 2% of adult cancer diagnoses; however, due to their location and often rapid clinical course, they are associated with high morbidity and mortality. About 50% of primary malignant CNS tumors are glioblastoma, with an incidence rate of 3.20 per 100,000 population for the United States. Incidence is higher in whites than in blacks (3.46 vs 1.79 per 100,000 population, respectively), with a 1.93:1 ratio (P < .05), a difference for which no biological explanation exists. Compared with whites, the incidence of glioblastoma is somewhat lower in Asians. The condition occurs more frequently in men than in women, with a 1.58:1 ratio (P < .05).[6] Over the last 3 decades, the incidence of glioblastoma in the United States has been relatively stable[7]; however, an aging population and better diagnostic tools may lead to a higher incidence of disease, as has been suggested in other countries.[8] Further study is needed to confirm changes in incidence, and, if present, to determine the causal factors.
Both environmental and patient-intrinsic factors may influence the risk of developing glioblastoma. An established risk factor is prior exposure to ionizing radiation to the CNS. The lag time between radiation and the development of glioblastoma may range from years to decades.[9-11] Unlike other cancers, there is no histologic or molecular signature that is pathognomonic for radiation-induced glioblastoma. The condition is observed in several hereditary cancer syndromes, including Lynch syndrome (with mutations in MSH2, MLH1, MSH6, and PMS2) and Li-Fraumeni syndrome (with mutations in TP53).[7] While mutations in some tumor suppressor genes increase the risk of susceptibility, the presence of an allergic disorder appears to be associated with a decreased incidence of glioma, including glioblastoma, across a number of epidemiologic and preclinical studies.[7,12-14]
Pathophysiology
Despite extensive study, the cellular origin of glioblastoma and the pathophysiologic mechanism of gliomagenesis remain uncertain. Research on the cell of origin for glioblastoma often involves targeting different precursor cell populations in transgenic mouse models and explores the effects of these interventions on the development of glioma. However, contemporary thought favors primitive pluripotent cells, including neural stem cells, glial precursor cells, and oligodendrocyte precursor cells.[15] Numerous preclinical models have been conducted in this area, each with their favorable attributes and drawbacks.[16-19]
Research demonstrates that, amongst IDH wild-type glioblastomas, there are spatial intratumoral differences in the mutational profile and clonality of tumor cells, with approximately half of the mutations being regionally exclusive. Distinct areas found within these tumors can exhibit a hypermutated phenotype. When present, mutations in the TERT gene appeared across all clones.[20] Recent studies utilizing xenografts in murine models have shown that these tumors consist of a slow-cycling population of stem-like cells, which give rise to a rapidly dividing progenitor cell population, a proportion of whose daughter cells develop into terminal differentiated cells, supporting a hierarchical model of gliomagenesis.[21] A minority of the clonal population proves resistant to chemotherapy.[21] In turn, this cell population will require different treatments. When evaluated longitudinally, recurrent glioblastoma can accumulate additional mutations,[22] and can appear similar to the primary tumor or may resemble a distinct subclonal population.[23,24] It is thought that this genomic heterogeneity is driven, at least in part, by the uneven cellular inheritance patterns of extra-chromosomal DNA.[25] As we garner a clearer understanding of the pathophysiology of gliomagenesis, new areas for potential therapeutic intervention will open up.
In addition to the difficulties associated with treating heterogenous tumors, which evolve over the course of the disease and harbor treatment-resistant subpopulations of cells, the blood-brain barrier is another impediment to the effective treatment of these tumors. The blood-brain barrier is a dynamic functional system, which both precludes and modulates the traversing of systemically administered therapies into the CNS, including CNS tumors.[26] Numerous means have been utilized to overcome this obstacle. Thus far, the most successful have included systemically administered drugs with adequate CNS penetration (eg, temozolomide) and locally delivered alternating electrical fields (tumor-treating fields, TTFields). Direct intracranial application of both chemotherapy (eg, biodegradable carmustine–impregnated wafers) and radiation (eg, brachytherapy) has also been explored.
Intratumoral injection of oncolytic viruses and chimeric antigen receptor (CAR) T-cell therapies is a modern example of a similar strategy that is undergoing active investigation.[27,28] Disruption of the blood-brain barrier to facilitate transmission of a systemically administered therapy has been under investigation for many decades. Initial studies utilized intra-arterially–administered agents.[29] A recent strategy being studied includes ultrasound to open up the barrier.[30] Another, which has had varying degrees of success, is avoiding the need to overcome the blood-brain barrier. The utilization of therapeutics whose direct activity occurs on the luminal side of the blood-brain barrier (eg, bevacizumab)[31]-or which act on the luminal side, with a goal of affecting function on the tumoral side of the barrier (eg, immune checkpoint inhibitors)-is another way to attempt to circumvent this obstacle. It is reasonable to surmise that more than one approach may prove to be successful.
Therapeutic Management
The therapeutic management of newly diagnosed glioblastoma typically involves a four-pronged approach. First, surgical resection is completed to the maximal safe extent, thereby reducing the tumor load and establishing a histopathological and molecular diagnosis. Following surgery, adjuvant radiotherapy is given with concomitant and maintenance chemotherapy, as is treatment of alternating electrical fields.
Surgery
Surgery plays an important diagnostic and therapeutic role in the management of glioblastoma: it offers tissue for histological and molecular diagnosis, immediate relief of the tumor-related mass effect and its associated symptoms, and potential cytoreduction. However, due to the invariably infiltrative nature of the disease, even macroscopically complete resection is not curative. Numerous retrospective studies have evaluated the value of the extent of resection in glioblastoma. While early work suggested a dichotomous picture with a need for a substantial extent of resection of the contrast-enhancing tumor,[32] subsequent studies demonstrated the graded benefit of the extent of resection.[33,34] A more recent meta-analysis also supports a more extensive resection with improved 1- and 2-year survival rates, as well as prolonged progression-free survival.[35] In low-grade glioma, the extent of resection is influenced by the area of increased signal on T2/fluid-attenuated inversion recovery (FLAIR) imaging.[36-39] Similarly, glioblastoma tumors are not limited to the area of enhancement but rather involve the area of increased T2/FLAIR signal. The extent of resection of this non-enhancing glioblastoma may also be of clinical impact, as demonstrated in a recent retrospective study.[40]
Although the association between extent of resection and survival has been reported and consistently confirmed in numerous studies, it is subject to several potential confounders, biases, and occult prognostic factors. While cytoreduction may intuitively delay disease recurrence, the non-linear growth of tumor cells seen in glioblastoma could quickly recover the tumor burden that was removed during surgery, negating the survival benefit of small increments of cytoreduction. The durability of the effect of cytoreduction, and whether it leads to a survival benefit, is likely related to the rate of tumor cell proliferation. On the other hand, patients with neurological deficits have lower functional status, which ultimately impacts their overall survival. Thus, it is possible that relief of mass effect leading to improved functional status from resection might prolong survival in symptomatic patients, irrespective of cytoreduction. Finally, the tumor location may also reflect the underlying biology and dictate the natural history of the disease. Determination of the influence of these previously described variables on overall survival is complicated, since resectable tumors may have an overall better prognosis, regardless of the actual extent of resection.
Resectable tumors often present in “silent areas of the brain” that tolerate injury for a long period of time prior to becoming symptomatic. In addition, resectable tumors, such as fronto-polar tumors, are more likely to harbor IDH1 mutations, which are associated with a better prognosis. In contrast, unresectable tumors, such as midline/diencephalic or brainstem tumors, often bear H3K27 mutations, which indicate an overall more aggressive biology and a worse prognosis.[41] Further dissection of the relationship between the extent of resection and survival requires controlling for tumor resectability. Yet, this complicated variable is difficult to capture by established scales, and is influenced by anatomical considerations, as well as neurosurgeon-related factors.[42]
Maximizing extent of resection. A number of technological advances have been developed to safely maximize the extent of resection, although their availability and usage may vary greatly. These techniques have become more widespread over time because, in addition to maximizing the extent of resection, they also optimize the safety of intra-axial brain tumor surgery. The major technological tools that surgeons use for improving the safety and accuracy of resection can be divided into three groups, as follows.
Intraoperative navigation technology. This technology involves the use of volumetric imaging (eg, MRI or CT scan), which is used as a reference to locate a lesion/anatomical structure within the surgical field. Navigation involves an optical or electromagnetic system that uses a physical reference to register the location and position of a patient’s head in space, and allows real-time visualization of instruments within the images, which are loaded to a computer. These technologies help minimize the extent of the open craniotomy exposure; optimize a trajectory to access lesions that avoids critical neural structures, such as white matter pathways; and provides an anatomical reference during the operation. However, they are limited by the fact that the referenced images are not updated as resection progresses, and brain shift in space in relation to the skull makes this information less reliable as the case advances. To address this, several groups have introduced intraoperative MRI, which provides a real-time update of the field for navigation.[43,44] The true utility and cost-effectiveness ratio of intraoperative MRI remains a highly debated topic, since cost and added time during the procedure are not insignificant. The use of intraoperative ultrasound is a dynamic, easy to use, and affordable alternative for real-time imaging during surgery.
Electrophysiological monitoring and functional brain mapping. Wilder Penfield and George Ojemann pioneered the use of electrodes to functionally map sensory and motor primary cortical regions and related subcortical circuits as the spinothalamic and corticospinal tracts to avoid postoperative deficits.[45-48] Over the last few decades, work by George Ojemann, Hugues Duffau, Mitchell Berger, and others has incorporated the routine use of awake brain mapping techniques, which have greatly improved the surveillance of motor circuits, language/comprehension, coordination, vision, and some higher cognitive functions by enabling them to be mapped and preserved.[49-53]
Fluorescent markers to maximize tumor visualization. Fluorescent dyes-which are either metabolized by tumor cells, or accumulate in areas of blood-brain barrier breakdown-have been incorporated to maximize tumor tissue visualization in the operating room. This is helpful, as gross tumor tissue often has a similar texture or color as the surrounding edematous brain and is not always easy to distinguish under bright light. The use of 5-aminolevulinic acid under blue light allows the neurosurgeon to view residual tumor in real-time during surgery. A phase III trial demonstrated an improved rate of complete resection (65% vs 36%; P < .0001) and an improved 6-month progression-free survival rate (41% vs 21%; P = .0003) for contrast-enhancing tumor with 5-aminolevulinic acid compared with conventional microsurgery with white light. However, this did not translate into an improvement in overall survival.[54] Fluorescein has also been used to visualize enhancing tumor, as this dye leaks through areas with defective blood-brain barrier.[55,56] Here, no special light source is needed.
Radiation therapy
Radiotherapy has been shown to improve survival in glioblastoma and plays a key role in treatment. Modern conformal radiotherapy-which utilizes three-dimensional computerized planning and multi-beam modulation-focally treats MRI-evident disease plus margin to a cumulative absorbed dose of 60 Gy. Given in daily doses of 1.8 to 2.0-Gy fractions, total treatment lasts approximately 6 weeks and is usually initiated 3 to 4 weeks after surgery. While some reports have suggested that delayed radiotherapy has a detrimental effect, other investigators have reported better outcomes; this question has yet to be definitively answered.[57,58] Up to 6 to 7 weeks of postoperative recovery is considered acceptable as part of the established standard of care.
Earlier studies have examined doses of more than 60 Gy, some of which incorporated stereotactic radiosurgery. However, they failed to demonstrate improved outcomes with doses of up to 76 Gy.[59] An ongoing randomized phase II study, NRG BN001 (ClinicalTrials.gov identifier: NCT02179086), is evaluating dose escalation to 75 Gy compared with standard 60-Gy radiotherapy.[60] This study includes distinct cohorts utilizing photons or protons, and the primary endpoint is survival.
For elderly patients or those with substantially altered performance status and poor prognosis, an abbreviated course of “hypofractionated” radiotherapy allows for a shortened overall treatment time. Long-term toxicity is of less concern in this population due to a commonly short survival. Hypofractionated radiation, which has been widely investigated, has been utilized to improve tolerability of radiotherapy (Table 1). Tumor volume often guides the selection of a radiation regimen because the risk of toxicity is theoretically greater with high vs low daily doses. Omitting radiotherapy (even less than the standard 60 Gy) leads to significantly worse survival compared with best supportive care alone.[61] Recent prospective data have demonstrated that abbreviated courses can also be safely and effectively combined with concurrent chemotherapy, as covered in the section below regarding treatment strategies for elderly patients.
A direct prospective comparison between full-course radiotherapy with concurrent and adjuvant chemotherapy vs abbreviated-course radiotherapy with concurrent and adjuvant chemotherapy has not been conducted. In addition to an abbreviated course of radiotherapy, the shorter course also employs a shorter course of concomitant chemotherapy. This lack of direct comparison leaves an important question not fully answered. In many clinical practices, the full course of radiotherapy and chemotherapy will be utilized in elderly patients with good performance status.
Systemic therapy
We recently reviewed in detail the pivotal late-phase trials that led to the current standard of care for patients with newly diagnosed glioblastoma.[62] These trials are summarized in Table 2. Temozolomide is a DNA-alkylating chemotherapy agent that is designed to readily cross the blood-brain barrier to achieve therapeutic concentrations in the brain. In 2005, a large, international, randomized, phase III trial, the European Organisation for Research and Treatment of Cancer (EORTC) 26981/22981/National Cancer Institute of Canada (NCIC) CE3 trial, demonstrated prolonged survival when daily temozolomide chemotherapy (75 mg/m2 daily × 40–49 days) is added concomitantly to radiotherapy followed by 6 cycles of maintenance temozolomide (150–200 mg/m2 × 5/28 days). Based on this landmark trial, temozolomide/radiotherapy followed by maintenance temozolomide has become the worldwide standard of care for patients with newly diagnosed glioblastoma.[63,64]
Temozolomide adds a methyl group to the DNA residues at the O6, N3, and N7 positions that, if unrepaired, leads to DNA strand breaks and cytotoxicity. More than one-third of glioblastomas are deficient in O6-methylguanine-DNA methyltransferase (MGMT), a repair protein that removes the methyl adduct from the O6 guanine position. This MGMT deficiency is via methylation of the MGMT gene promoter, which leads to downregulated transcription. Glioblastoma patients with a silenced MGMT gene who are treated with an alkylating agent chemotherapy have a longer survival than those with an unmethylated MGMT and those treated with radiotherapy alone.[65] In studies of paired tissue samples, MGMT promoter methylation is relatively conserved from the newly diagnosed to progressive disease settings, with the majority of tumors maintaining an unchanged profile over time.[66,67]
In mismatch repair–deficient conditions, the O6 guanine methyl adduct is tolerated and can be mutagenic. This may be a key mechanism in the development of glioma mutations due to temozolomide, and is described in low-grade glioma progressing to higher-grade tumors, as well as potentially in the development of a hypermutated phenotype.[68,69] The methyl adducts at N3 and N7 are addressed by the base excision repair mechanism.[70] Inhibition of this mechanism continues to undergo investigation in trials of poly (ADP-ribose) polymerase (PARP) inhibitors.
Optimal duration of adjuvant temozolomide chemotherapy. The pivotal EORTC/NCIC study established a regimen of up to 6 adjuvant chemotherapy cycles. However, in the United States, the duration of chemotherapy may still extend for up to 12 cycles or more in non-progressive patients. While early treatment discontinuation is a concern due to the disease’s poor prognosis, cumulative toxicity, impaired bone marrow reserve for subsequent second-line chemotherapy, and increased risk of secondary malignancies are concerns with prolonged treatment. In some trials, treatment was allowed per local practice to be extended to up to 12 cycles.
A pooled meta-analysis of individual patient outcomes data stemming from four randomized trials compared the duration of maintenance temozolomide chemotherapy (6 cycles vs 7+ cycles) among individuals who were non-progressive after 6 cycles.[71] While there was a slight improvement in progression-free survival, no difference in survival was seen for those who received 6 cycles vs more than 6 cycles of chemotherapy. This suggests that prolonged administration and dose intensification do not improve disease control. At this time, the value of temozolomide during radiotherapy, independent of adjuvant temozolomide in the treatment of glioblastoma, is unknown.
Alternative temozolomide dosing schedules. Alternative dosing schedules have been investigated in the newly diagnosed and recurrent disease settings. However, none of these regimens have been shown to be superior to the standard temozolomide dosing schedule. The randomized Radiation Therapy Oncology Group (RTOG) 0525 study found no benefit with intensified maintenance chemotherapy. Patients were randomized at the end of chemoradiotherapy to either standard maintenance therapy (150–200 mg/m2/day × 5/28 days) or an intensified daily regimen (75 mg/m2/day × 21/28 days), effectively doubling the cumulative dose of chemotherapy. No difference in outcomes was noted, and a higher incidence of grade 3/4 toxicities was observed in the investigational arm.[72]
Hopes and disappointments with bevacizumab. The addition of the anti- angiogenic agent bevacizumab to radiotherapy and temozolomide has been explored in two phase III trials focusing on newly diagnosed glioblastoma[73,74] and one phase III trial focusing on recurrent glioblastoma.[75] The observed and expected improvement in progression-free survival based on imaging did not translate into any improvement in overall survival when bevacizumab was added. Unplanned post-hoc analyses found an association of improved overall survival in a molecularly defined subset of patients.[76] The addition of bevacizumab to hypofractionated radiotherapy demonstrated no improvement in overall survival compared with hypofractionated radiotherapy alone in elderly (≥ 65 years) patients with newly diagnosed glioblastoma.[77] Based on the results of these trials, bevacizumab should not be administered as part of primary treatment of glioblastoma. Of note, some physicians utilize bevacizumab as a corticosteroid-sparing agent to decrease cerebral edema, so that treatment with standard radiotherapy and chemotherapy is feasible without high doses or prolonged use of corticosteroids.
De-escalation of treatment in the elderly. De-escalation of therapeutic interventions has been extensively explored in the elderly and in frail populations with glioblastoma. This interest is driven by the overall brief survival of elderly glioblastoma patients, and thus the desire to shorten the duration of medical intervention. This topic has recently been reviewed in detail.[78,79] Several studies have prospectively evaluated abbreviated courses of radiotherapy in these patients (as covered earlier in the “Radiation Therapy” section).
Two large randomized trials have evaluated the exclusive administration of temozolomide chemotherapy in the elderly. Consistently, both trials demonstrated that withholding radiotherapy and instead treating patients with temozolomide alone may be an option for elderly patients with tumors harboring a methylated MGMT gene promoter, while this strategy is detrimental in the absence of MGMT methylation.[80,81] Monotherapy with temozolomide offers the advantage of an oral treatment regimen without the need for daily radiotherapy. The utilization of a short-course hypofractionated radiotherapy regimen (of 40 Gy in 15 treatments) with concomitant temozolomide, followed by adjuvant temozolomide, was shown to improve outcomes in the elderly, which is consistent with the observed benefit reported 10 years earlier by the EORTC/NCIC trial in patients up to age 70 years.[82] The clinical circumstances, including chronologic age, performance status, concurrent medical problems, MGMT promoter methylation status, and logistical concerns should all be weighed during therapeutic decision making for elderly patients with glioblastoma. In healthy MGMT-methylated elderly patients with good performance status, a more aggressive approach, including full-course radiotherapy and temozolomide, can be considered.
Poor performance status. Both de-escalation and escalation of care for patients with poor performance status have been considered. Many of these evaluations have been performed specifically in the elderly population, thus potentially limiting their generalizability to younger patients. De-escalation approaches attempt to limit the toxicity of treatment in a patient population that may not tolerate and is less likely to benefit from therapy. These approaches also attempt to shorten treatment duration, as well as the amount of travel to the treatment facility, particularly for patients with limited mobility.
The previously discussed abbreviated radiotherapy courses for elderly patients are also often used in the frail population with a poorer performance status; some prospective studies on abbreviated radiotherapy included patients on the basis of performance status alone.[83,84] The use of temozolomide chemotherapy alone has been studied in patients with poor performance status (Karnofsky Performance Score [KPS] of < 70); it was shown to be associated with an improvement in performance status or an improvement to the level of self-care (KPS ≥ 70) in one-third and one-fourth of patients, respectively.[85] Increasing the number of concomitant therapeutics has been performed with the goals of extending survival and improving functionality. One treatment intensification approach adds bevacizumab to the standard of care, relying on the corticosteroid-sparing effects described earlier. This approach has demonstrated only a transient improvement in performance status, and the data thus far do not justify its routine employment, since median overall survival remained short at 5.6 months (95% CI, 4.4–6.4).[86]
TTFields
The addition of TTFields to maintenance temozolomide chemotherapy for newly diagnosed glioblastoma patients has recently been incorporated as a new standard of care.[87-89] TTFields are applied via multiple electrodes that are directly fixed to the scalp. These low-intensity alternating electrical fields of 200 Hz interfere with polar organelles (eg, tubulins), which are required for normal cell division. Mitotic disruption ultimately leads to cell cycle arrest, aneuploidy, and apoptosis.[90,91] Additional mechanisms potentially contributing to therapy-associated effects include a disruption of organelles and an induction or modulation of the anti-glioma immune response.[92]
The effect of TTFields was evaluated in two large, prospective, non-blinded randomized trials. In recurrent disease, TTFields failed to show superiority over best physicians’ choice therapy in patients with recurrent glioblastoma.[93] In a pivotal large, randomized, phase III trial, 695 patients with newly diagnosed glioblastoma were randomized to receive adjuvant temozolomide and TTFields or standard maintenance therapy of temozolomide alone after the end of initial treatment with temozolomide/radiotherapy. Patients who received adjuvant temozolomide and TTFields fared much better than those treated with temozolomide alone. Survival was prolonged, with a hazard ratio of 0.63 (95% CI, 0.52–0.76; P < .001), and durable survival was achieved in some patients.[88] This improvement was observed without a measurable negative impact on health- related quality of life.[94] In the real-world setting, the rate of compliance among patients utilizing TTFields is high.[95] The primary toxicity noted in the trials was mild-to-moderate cutaneous toxicity, which typically resolves with minimal intervention.[96]
Impact of Other Medications
It has been hypothesized that certain medications commonly used to treat other conditions may potentially benefit patients with glioblastoma. These range from those prescribed for tumor-related conditions-such as epilepsy[97,98] and cerebral edema-to those which are independent of the neoplastic disease, including hypertension, hyperlipidemia, and venous thromboembolism.[99,100] Thus far, none have been proven to be beneficial. When thoroughly evaluated, none of the associations observed in several studies could be validated in larger cohorts, underscoring the importance of prospective (rather than retrospective) trials with strong biological hypotheses.
Corticosteroids
Corticosteroids are frequently used to decrease cerebral edema. Their off-target effects also lead to the suppression of immune system activity. Recent preclinical and clinical work suggests that these unfavorable effects contribute to shortened survival.[101] This is of particular importance as we evaluate the role of immunotherapeutic approaches for the treatment of glioma.[102] Despite the lack of a clear benefit in survival, bevacizumab has been shown to decrease the utilization of corticosteroids in patients with glioblastoma in numerous trials.[73,74,103-105] In routine clinical practice, functional improvement is often seen in association with radiographic improvement; however, it has not been proven to correlate with improved overall survival.
Future Directions
Efforts are continuously being undertaken to improve outcomes for patients with newly diagnosed glioblastoma. The diminishing return of second- and subsequent-line oncologic therapies supports the testing of promising new therapeutic approaches in the newly diagnosed population. This is underscored by the strong survival benefit seen among patients treated with TTFields in the newly diagnosed setting compared with those with progressive disease. A number of novel regimens are being studied in the newly diagnosed setting (Table 3). While many contemporary trials for newly diagnosed glioblastoma build upon the standard of care, as previously described, trials for patients with unmethylated MGMT promoter status may omit temozolomide without losing treatment efficacy.[106-108]
Epidermal growth factor receptor (EGFR) remains an attractive therapeutic target, since it is frequently upregulated in glioblastoma, and its expression is associated with a worse prognosis; it is constitutionally activated in 30% of glioblastomas with a VIII variant. However, randomized trials targeting EGFR have repeatedly failed.[109,110] The addition of a novel peptide vaccine, rindopepimut, to the standard of care has been studied in a phase III trial. While the preclinical and early-phase studies held substantial promise, the phase III trial failed to demonstrate improved survival.[110] Phase III trial evaluation of the antibody-drug conjugate depatuxizumab mafodotin (ABT-414) in combination with standard-of-care treatment for patients with EGFR-amplified newly diagnosed glioblastoma is eagerly awaited.[111] Finally, the results of two separate trials evaluating the anti–programmed death 1 monoclonal antibody nivolumab in newly diagnosed glioblastoma patients with unmethylated (CheckMate-498)[112] and methylated (CheckMate-548)[113] MGMT promoter status are anticipated. Biomarkers that may help predict benefit from immunotherapies[114] will require prospective evaluation, but may provide insight into the role of immunotherapeutic approaches in glioblastoma.
Conclusion
The therapeutic management of newly diagnosed glioblastoma is well-defined and includes surgery, radiation, temozolomide, and TTFields. Nuances to management in the elderly or frail exist; in these populations, treatment de-escalation is often considered on a patient-specific basis. The addition of other systemic therapies-such as antiangiogenic agents or other routinely administered medications, such as anti-epileptic or blood pressure agents-has not been shown to improve survival in newly diagnosed glioblastoma. Concerns exist, substantiated by both preclinical and clinical data, that corticosteroid utilization may negatively impact outcomes of immunotherapeutic approaches for the treatment of these patients. This will need to be carefully considered in the design, administration, and interpretation of clinical trials for this disease. As outcomes in glioblastoma remain poor, continued investigation into promising therapeutics is necessary.
Financial Disclosure: Dr. Lukas, Dr. Wainwright, Dr. Sonabend, and Dr. Stupp receive funding support from P50CA221747 SPORE for Translational Approaches to Brain Tumors. Dr. Lukas is a consultant for AbbVie, and has served as a consultant for NewLink Genetics and ReNeuron; he has also served on an advisory board for Monteris Medical; served as a medical editor for EBSCO and MedLink Neurology; and has presented CME board review courses for the American Physician Institute. Dr. Wainwright receives funding support from the NIH/National Institute of Neurological Disorders and Stroke R01NS097851 grant. Dr. Sonabend is a consultant for AbbVie. Dr. Stupp receives travel support from NovoCure; he also served on one-time advisory boards for Boehringer Ingelheim, Celgene, and Northwest Biotherapeutics. Dr. Ladomersky and Dr. Sachdev have no significant financial interest in or other relationship with the manufacturer of any product or provider of any service mentioned in this article.
PERSPECTIVE
Glioblastoma-What’s Next?
Nicholas Butowski, MD
Glioblastoma remains a macabre tumor with only incremental improvement over the last 4 to 5 decades. Fortunately, we practice in a time of remarkable growth in our neuroscience and cancer biology knowledge base. This leads one to hope that innovation in the management of glioblastoma is close at hand.
In the near future, operative methods will continue to trend toward decreased invasiveness, through techniques such as guided laser thermal ablation. Surgical precision will improve through fluorescence-guided resection of tumors. Drug delivery, too, will be optimized with the use of transport vesicles steered by engineered proteins and nanoparticles, used as vehicles to deliver therapeutic agents across the blood-brain barrier. Consequently, many drugs previously thought unsuitable for glioblastoma due to systemic toxicity or blockage by the blood-brain barrier may prove useful.
Moreover, it is expected that big data, next-generation sequencing, and genetic identification algorithms will guide operative intervention, clinical trials, and medication selection. Such methods will also account for the marked heterogeneity in glioblastoma and lead to an era of molecular polytherapy, guided by analysis from numerous tumor samples from the same patient. Such tailored ‘molecular cocktails’ will improve efficacy by targeting upstream initiators, alterations enabling cell growth, and predicted downstream compensation/resistance mechanisms. Recent advances in sequencing of tumor DNA from circulating tumor markers will make such clinical trials easier to perform and less reliant on operative procedures such as invasive tumor biopsies. Hope, too, remains that combination immunotherapy will play a role in glioblastoma management, whether by tailoring immune cells to target glioblastoma or by reinvigorating appropriate microglial function.
Insights on stem cell biology will also help to advance our management of glioblastoma. While radiation and traditional chemotherapy may serve a waning role in the future, their efficacy will be improved by simultaneous use of agents targeting tumor stem cell quiescence. Realistically, though, salvage therapy will still be required, and one can envision the use of self-replicating viruses to fight tumor stem cells, finally partially fulfilling the promise inherent in our present knowledge base.
To completely fulfill our promise to our patients, we’ll have to accept that glioblastoma is a disease of information and mixed-up signals among the genome, epigenome, microbiome, proteome, transcriptome, and metabolome, among others. As such, we’ll need a better bibliome of all the expanding information that separates the inessential from the pertinent.
Financial Disclosure:Dr. Butowski has no significant financial interest in or other relationship with the manufacturer of any product or provider of any service mentioned in this article.
Dr. Butowski is a Professor of Neurological Surgery; Director of Translational Research and Director of the UCSF Fellowship in the Division of Neuro-Oncology; and Chair of the CNS Tumors Site Committee at UCSF Helen Diller Family Comprehensive Cancer Center in San Francisco, California. He is also a Neuro-Oncologist in the Department of Neurological Surgery at the University of California, also in San Francisco.
References:
1. Bailey P, Cushing H. A classification of the tumours of the glioma group on a histogenetic basis, with a corre-lated study of prognosis. Br J Surg. 1926;14:554-5.
2. Louis DN, Ohgaki H, Wiestler OD, et al. The 2007 WHO classification of tumors of the central nervous sys-tem. Acta Neuropathol. 2007;114:97-109.
3. Louis DN, Perry A, Reifenberger G, et al. The 2016 World Health Organization classification of tumors of the central nervous system: a summary. 2016;131:803-20.
4. Brat DJ, Aldape K, Colman H, et al. cIMPACT-NOW update 3: recommended diagnostic criteria for “diffuse astrocytic glioma, IDH-wildtype, with molecular features of glioblastoma, WHO grade IV”. Acta Neuropathol. 2018;136:805-10.
5. Velázquez Vega JE, Brat DJ. Incorporating advances in molecular pathology into brain tumor diagnostics. Adv Anat Pathol. 2018;25:143-71.
6. Ostrum QT, Gittleman H, Liao P, et al. CBTRUS statistical report: primary brain and other central nervous sys-tem tumors diagnosed in the United States in 2010-2014. Neuro Oncol. 2017;19(suppl 5):v1-88.
7. Ostrum QT, Bauchet L, Davis FG, et al. The epidemiology of glioma in adults: a “state of the science” review. Neuro Oncol. 2014;16:896-913.
8. Philips A, Henshaw DL, Lamburn G, O’Carroll M. Brain tumors: rise in glioblastoma multiforme incidence in England 1995-2015 suggests an adverse environmental or lifestyle factor. J Environ Public Health. 2018 Jun 24. [Epub ahead of print]
9. Elsamadicy AA, Babu R, Kirkpatrick JP, Adamson DC. Radiation-induced malignant gliomas: a current re-view. World Neurosurg. 2015;83:530-42.
10. Taylor AJ, Little MP, Winter DL, et al. Population based risks of CNS tumors in survivors of childhood can-cer. J Clin Oncol. 2010;28:5287-93.
11. Neglia JP, Robison LL, Stovall M, et al. New primary neoplasms of the central nervous system in survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. J Natl Cancer Inst. 2006;98:1528-37.
12. Krishnamachari B, Il’yasova D, Scheurer ME, et al. A pooled multisite analysis of the effects of atopic medical conditions in glioma risk in different ethnic groups. Ann Epidemiol. 2015;25:270-4.
13. Amirian ES, Zhou R, Wrensch MR, et al. Approaching a scientific consensus on the association between al-lergies and glioma risk: a report from the Glioma International Case-Control Study. Cancer Epidemiol Biomarkers Prev. 2016;25:282-90.
14. Schwartzbaum JA, Hwang K, Lawler S, et al. Allergy and inflammatory transcriptome is predominantly nega-tively correlated with CD133 expression in glioblastoma. Neuro Oncol. 2010;12:320-7.
15. Shao F, Liu C. Revisit the candidacy of brain cell types as the cell(s) of origin for human high-grade glioma. Front Mol Neurosci. 2018;11:48.
16. Miyami M, Tomita H, Soeda A, et al. Current trends in mouse models of glioblastoma. J Neurooncol. 2017;135:423-32.
17. Lei L, Sonabend AM, Guarnieri P, et al. Glioblastoma models reveal the connection between adult glial pro-genitors and the proneural phenotype. PLoS One. 2011 May 23. [Epub ahead of print]
18. Sonabend AM, Bansal M, Guarnieri P, et al. The transcriptional regulatory network of proneural glioma de-termines the genetic alterations selected during tumor progression. Cancer Res. 2014;74:1440-51.
19. Verhaak RG, Hoadley KA, Purdom E, et al. Integrated genomic analysis identifies clinically relevant subtypes of glioblastoma characterized by abnormalities in PDGFRA, IDH1, EGFR, and NF1. Cancer Cell. 2010;17:98-110.
20. Mahlokozera T, Vellimana AK, Li T, et al. Biological and therapeutic implications of multisector sequencing in newly diagnosed glioblastoma. Neur Oncol. 2018;20:472-83.
21. Lan X, Jorg DJ, Cavalli FMG, et al. Fate mapping of human glioblastoma reveals an invariant stem cell hierar-chy. Nature. 2017;549:227-32.
22. Wang J, Cazzato E, Ladewig E, et al. Clonal evolution of glioblastoma under therapy. Nat Gent. 2016;48:768-76.
23. Kim H, Zheng S, Amini SS, et al. Whole-genome and multisector exome sequencing of primary an post-treatment glioblastoma reveals patterns of tumor evolution. Genome Res. 2015;25:316-27.
24. Neilsen BK, Sleightholm R, McComb R, et al. Comprehensive genetic alteration profiling in primary and re-current glioblastoma. J Neurooncol. 2018 Dec 9. [Epub ahead of print]
25. deCarvalho AC, Kim H, Poisson LM, et al. Discordant inheritance of chromosomal and extrachromosomal DNA elements contributes to dynamic disease evolution in glioblastoma. Nat Genet. 2018;50:708-17.
26. Banks WA. From blood-brain barrier to blood-brain interface: new opportunities for CNS drug delivery. Nat Rev Drug Discov. 2016;15:275-92.
27. Panek WK, Kane JR, Young JS, et al. Hitting the nail on the head: combining adenovirus-mediated virothera-py and immunomodulation for the treatment of glioma. Oncotarget. 2017;8:89391-405.
28. Maxwell R, Luksik AS, Garzon-Muvdi T, Lim M. The potential of cellular- and viral-based immunotherapies for malignant glioma-dendritic cell vaccines, adoptive cell transfer, and oncolytic viruses. Curr Neurol Neurosci Rep. 2017;17:50.
29. Joshi S, Ellis JA, Ornstein E, Bruce JN. Intrarterial drug delivery for glioblastoma multiforme: will the phoe-nix rise again? J Neurooncol. 2015;124:333-43.
30. Carpentier A, Canney M, Vignopt A, et al. Clinical trial of blood-brain barrier disruption by pulsed ultra-sound. Sci Transl Med. 2016;8:343re2.
31. Hundsberger T, Reardon DA, Wen PY. Angiogenesis inhibitors in tackling recurrent glioblastoma. Expert Rev Anticancer Ther. 2017;17:507-15.
32. Lacroix M, Abi-Said D, Fourney DR, et al. A multivariate analysis of 416 patients with glioblastoma multi-forme: prognosis, extent of resection, and survival. J Neurosurg. 2001;95:190-8.
33. Sanai N, Polley MY, McDermott MW, et al. An extent of resection threshold for newly diagnosed glioblas-toma. J Neurosurg. 2011;115:3-8.
34. Chaichana KL, Jusue-Torres I, Navarro-Ramirez R, et al. Establishing percent resection and residual volume thresholds affecting survival and recurrence for patients with newly diagnosed intracranial glioblastoma. Neuro Oncol. 2014;16:113-22.
35. Brown TJ, Brennan MC, Li M, et al. Association of the extent of resection with survival in glioblastoma: a systematic review and meta-analysis. JAMA Oncol. 2016;2:1460-9.
36. Jakola AS, Myrmel KS, Kloster R, et al. Comparison of a strategy favoring early surgical resection vs a strate-gy favoring watchful waiting in low-grade gliomas. JAMA. 2012;308:1881-8.
37. Xia L, Fang C, Chen G, Sun C. Relationship between the extent of resection and the survival of patients with low-grade gliomas: a systematic review and meta-analysis. BMC Cancer. 2018;18:48.
38. Duffau H. Long-term outcomes after supratotal resection of diffuse low-grade gliomas: a consecutive series with 11-year follow-up. Acta Neurochir (Wien). 2016;158:51-8.
39. Smith JS, Chang EF, Lamborn KR, et al. Role of extent of resection in the long-term outcome of low-grade hemispheric gliomas. J Clin Oncol. 2008;26:1338-45.
40. Kotrotsou A, Elakkad A, Sun J, et al. Multi-center study finds postoperative residual non-enhancing compo-nent of glioblastoma as a new determinant of patient outcome. J Neurooncol. 2018;139:125-33.
41. Beiko J, Suki D, Hess KR, et al. IDH1 mutant malignant astrocytomas are more amenable to surgical resection and have a survival benefit associated with maximal surgical resection. Neuro Oncol. 2014;16:81-91.
42. Sonabend AM, Zacharia BE, Cloney MB, et al. Defining glioblastoma resectability through the wisdom of the crowd: a proof-of-principle study. Neurosurgery. 2017;80:590-601.
43. Napolitano N, Vaz G, Lawson TM, et al. Glioblastoma surgery with and without intraoperative MRI at 3.0T. Neurochirurgie. 2014;60:143-50.
44. Kuhnt D, Becker A, Ganslandt O, et al. Correlation of the extent of tumor volume resection and patient surviv-al in surgery of glioblastoma multiforme with high field intraoperative MRI guidance. Neuro Oncol. 2011;13:1339-48.
45. Penfield W. The electrode, the brain and the mind. Z Neurol. 1972;201:297-309.
46. Penfield W. Combined regional and general anesthesia for craniotomy and cortical exploration. Part I. Neuro-surgical considerations. Int Anesthesiol Clin. 1986;24:1-11.
47. Keles GE, Lundin DA, Lamborn KR, et al. Intraoperative subcortical stimulation mapping for hemispherical perirolandic gliomas located within or adjacent to the descending motor pathways: evaluation of morbidity and as-sessment of functional outcomes in 294 patients. J Neurosurg. 2004;100:369-75.
48. Farrell DF, Leeman S, Ojemann GA. Study of the human visual cortex: direct cortical evoked potentials and stimulation. J Clin Neurophysiol. 2007;24:1-10.
49. Ojemann G, Ojemann J, Lettich E, Berger MS. Cortical language localization in left, dominant hemisphere. An electrical stimulation mapping investigation in 117 patients. 1989. J Neurosurg. 2008;108:411-21.
50. Engel AK, Moll CK, Fried I, Ojemann GA. Invasive recordings from the human brain: clinical insights and beyond. Nat Rev Neurosci. 2005;6:35-47.
51. Duffau H. Mapping the connectome in awake surgery for gliomas: an update. J Neurosurg Sci. 2017;61:612-30.
52. Southwell DG, Riva M, Jordan K, et al. Language outcomes after resection of dominant inferior parietal lobule gliomas. J Neurosurg. 2017;127:781-9.
53. Sanai N, Mirzadeh Z, Berger MS. Functional outcome after language mapping for glioma resection. N Engl J Med. 2008;358:18-27.
54. Stummer W, Pichelmeier U, Meinel T, et al. Fluorescence-guided surgery with 5-aminolevulinic acid for re-section of malignant glioma: a randomized controlled multicentre phase III trial. Lancet Oncol. 2006;7:392-401.
55. Bowden SG, Neira JA, Gill BJA, et al. Sodium fluorescein facilitates guided sampling of diagnostic tumor tissue in nonenhancing gliomas. Neurosurgery. 2018;82:719-27.
56. Catapano G, Sgulò FG, Seneca V, et al. Fluorescein-guided surgery for high-grade glioma resection: an in-traoperative “contrast enhancer”. World Neurosurg. 2017;104:239-47.
57. Han SJ, Englot DJ, Birk H, et al. Impact of timing of concurrent chemoradiation for newly diagnosed glioblas-toma: a critical review of current evidence. Neurosurgery. 2016;62(suppl 1):160-5.
58. Han SJ, Rutledge WC, Molinaro AM, et al. The effect of timing of concurrent chemoradiation in patients with newly diagnosed glioblastoma. Neurosurgery. 2015;77:248-53.
59. Kirkpatrick JP, Laack NN, Shih HA, Gondi V. Management of GBM: a problem of local recurrence. J Neu-rooncol. 2017;134:487-93.
60. NIH U.S. National Library of Medicine, ClinicalTrials.gov. Dose-escalated photon IMRT or proton beam ra-diation therapy versus standard-dose radiation therapy and temozolomide in treating patients with newly diagnosed glioblastoma. ClinicalTrials.gov identifier: NCT02179086. https://clinicaltrials.gov/ct2/show/NCT02179086. Ac-cessed February 7, 2019.
61. Keime-Guibert F, Chinot O, Taillandier L, et al. Radiotherapy for glioblastoma in the elderly. N Engl J Med. 2007;356:1527-35.
62. Lukas RV, Mrugala MM. Pivotal therapeutic trials for infiltrating gliomas and how they affect clinical practice. Neurooncol Pract. 2017;4:209-19.
63. Stupp R, Mason WP, van den Bent MJ, et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med. 2005;352:987-96.
64. Stupp R, Hegi ME, Mason WP, et al. Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet Oncol. 2009;10:459-66.
65. Hegi ME, Diserens AC, Gorlia T, et al. MGMT gene silencing and benefit from temozlomide in glioblastoma. N Engl J Med. 2005;352:997-1003.
66. Felsberg J, Thon N, Eigenbrod S, et al. Promoter methylation and expressionof MGMT and the DNA mis-match repair genes MLH1, MSH2, MSH6, and PMS2 in paired primary and recurrent glioblastomas. Int J Can-cer. 2011;129:659-70.
67. O’Regan CJ, Kearney H, Beausang A, et al. Temporal stability of MGMT promoter methylation in glioblas-toma patients undergoing STUPP regimen. J Neurooncol. 2018;137:233-240.
68. Choi S, Yu Y, Grimmer MR, et al. Temozlomide-associated hypermutation in gliomas. Neuro Oncol. 2018;20:1300-9.
69. Van Thuijl HF, Mazor T, Johnson BE, et al. Evolution of DNA repair defects during malignant progression of low-grade gliomas after temozolomide treatment. Acta Neuropathol. 2015;129:597-607.
70. Zhang J, Stevens MF, Bradshaw TD. Temozolomide: mechanisms of action, repair, and resistance. Curr Mol Pharmacol. 2012;5:102-14.
71. Blumenthal DT, Gorlia T, Gilbert MR, et al. Is more better? The impact of extended adjuvant temozolomide in newly diagnosed glioblastoma: a secondary analysis of EORTC and NRG Oncology/RTOG. Neuro Oncol. 2017;19:1119-26.
72. Gilbert MR, Wang M, Aldape KD, et al. Dose-dense temozolomide for newly diagnosed glioblastoma: a ran-domized phase III clinical trial. J Clin Oncol. 2013;31:4085-91.
73. Gilbert MR, Dignan JJ, Armstrong TS, et al. A randomized trial of bevacizumab for newly diagnosed glio-blastoma. N Engl J Med. 2014;370:699-708.
74. Chinot OL, Wick W, Mason W, et al. Bevacizumab plus radiotherapy-temozolomide for newly diagnosed gli-oblastoma. N Engl J Med. 2014;370:709-22.
75. Wick W, Gorlia T, Bendszus M, et al. Lomustine and bevacizumab in progressive glioblastoma. N Engl J Med. 2017;377:1954-63.
76. Sandmann T, Bourgon R, Garcia J, et al. Patients with proneural glioblastoma may derive overall survival benefit from the addition of bevacizumab to first-line radiotherapy and temozolomide: a retrospective analysis of the AVAglio trial. J Clin Oncol. 2015;33:2735-44.
77. Wirsching HG, Tabatabai G, Roelcke U, et al. Bevacizumab plus hypofractionated radiotherapy versus radio-therapy alone in elderly patients with glioblastoma: the randomized, open-label, phase II ARTE trial. Ann Oncol. 2018;29:1423-30.
78. Young JS, Chmura SJ, Wainwright DA, et al. Management of glioblastoma in elderly patients. J Neurol Sci. 2017;380:250-5.
79. Das S, Kim AH, Chang S, Berger MS. Management of elderly patients with glioblastoma after CE.6. Front Oncol. 2017;7:196.
80. Wick W, Platten M, Meisner C, et al. Temozolomide chemotherapy alone versus radiotherapy alone for malig-nant astrocytoma in the elderly: the NOA-08 randomised, phase III trial. Lancet Oncol. 2012;13:707-15.
81. Malmstrom A, Gronberg BH, Marosi C, et al. Temozolomide versus standard 6 week radiotherapy versus hypofractionated radiotherapy in patients older than 60 years with glioblastoma: the Nordic, randomized phase 3 trial. Lancet Oncol. 2012;13:916-26.
82. Perry JR, Laperriere N, O’Callaghan CJ, et al. Short-course radiation plus temozolomide in elderly patients with glioblastoma. N Engl J Med. 2017;376:1027-37.
83. Bauman GS, Gaspar LE, Fisher BJ, et al. A prospective study of short-course radiotherapy in poor prognosis glioblastoma multiforme. Int J Radiat Oncol Biol Phys. 1994;29:835-9.
84. Roa W, Kepka L, Kumar N, et al. International Atomic Energy Agency randomized phase III study of radia-tion therapy in elderly and/or frail patients with newly diagnosed glioblastoma multiforme. J Clin Oncol. 2015;33:4145-50.
85. Gallego Perez-Larraya J, Ducray F, Chinot O, et al. Temozolomide in elderly patients with newly diagnosed glioblastoma and poor performance status: an ANOCEF phase II trial. J Clin Oncol. 2011;29:3050-5.
86. Reyes-Botero G, Cartalat-Carel S, Chinot OL, et al. Temozolomide plus bevacizumab in elderly patients with newly diagnosed glioblastoma and poor performance status: an ANOCEF phase II trial (ATAG). Oncologist. 2018;23:524-e44.
87. Stupp R, Taillibert S, Kanner AA, et al. Maintenance therapy with tumor-treating fields plus temozlomide alone for glioblastoma: a randomized clinical trial. JAMA. 2015;314:2535-43.
88. Stupp R, Taillibert S, Kanner A, et al. Effect of tumor-treating fields plus maintenance temozolomide vs maintenance temozolomide alone on survival in patients with glioblastoma: a randomized clinical trial. JAMA. 2017;318:2306-16.
89. Nabors LB, Portnow J, Ammiraiti M, et al. NCCN Guidelines Insights: Central Nervous System Cancers, Version 1.2017. J Natl Compr Canc Netw. 2017;15:1331-45.
90. Mrugala MM, Ruzevick J, Zlomanczuk P, Lukas RV. Tumor treating fields in neuro-oncological practice. Curr Oncol Rep. 2017;19:53.
91. Hottinger AF, Pacheco P, Stupp R. Tumor treating fields: a novel treatment modality and its use in brain tu-mors. Neuro Oncol. 2016;18:1338-49.
92. Zhu P, Zhu JJ. Tumor treating fields: a novel and effective therapy for glioblastoma: mechanism, efficacy, safety, and future perspectives. Chin Clin Oncol. 2017;6:41.
93. Stupp R, Wong ET, Kanner AA, et al. NovoTTA-100A versus physicians’ choice chemotherapy in recurrent glioblastoma: a randomized phase III trial of a novel treatment modality. Eur J Cancer. 2012;48:2192-202.
94. Taphoorn MJB, Dirven L, Kanner AA, et al. Influence of treatment of tumor-treating fields on health-related quality of life of patients with newly diagnosed glioblastoma: a secondary analysis of a randomized clinical trial. JAMA Oncol. 2018 Apr 1. [Epub ahead of print]
95. Onken J, Staub-Bartlett F, Vajkocy P, Misch M. Acceptance and compliance of TTFields treatment among high-grade glioma patients. J Neurooncol. 2018;139:177-84.
96. Lukas RV, Ratterman KL, Wong ET, Villano JL. Skin toxicities associated with tumor treating fields: case based review. J Neurooncol. 2017;135:593-9.
97. Weller M, Gorlia T, Cairncross JD, et al. Prolonged survival with valproic acid use in the EORTC/NCIC te-mozolomide trial of glioblastoma. Neurology. 2011;77:1156-64.
98. Happold C, Gorlia T, Chinot O, et al. Does valproic acid or levitaracetam improve survival in glioblastoma? A pooled analysis of prospective clinical trials in newly diagnosed glioblastoma. J Clin Oncol. 2016;34:731-9.
99. Happold C, Gorlia T, Nabors LB, et al. Do statins, ACE inhibitors, or sartans improve outcome in primary glioblastoma? J Neurooncol. 2018;138:163-71.
100. Le Rhun E, Genbrugge E, Stupp R, et al. Associations of anticoagulant use with outcome in newly diagnosed glioblastoma. Eur J Cancer. 2018;101:95-104.
101. Pitter KL, Tamagno I, Alikhanyan K, et al. Corticosteroids compromise survival in glioblastoma. Brain. 2016;139(pt 5):1458-71.
102. Giles AJ, Hutchinson MND, Sonnemann HM, et al. Dexamethasone-induced immunosuppression: mecha-nisms and implications for immunotherapy. J Immunother Cancer. 2018;6:51.
103. Vredenburgh JJ, Cloughesy T, Samant M, et al. Corticosteroid use in patients with glioblastoma at first or second relapse treated with bevacizumab in the BRAIN study. Oncologist. 2010;15:1329-34.
104. Ananthnarayan S, Bahng J, Roring J, et al. Time course of imaging changes of GBM during extended bevacizumab treatment. J Neurooncol. 2008;88:339-47.
105. Ellingson BM, Cloughesy TF, Lai A, et al. Quantitative volumetric analysis of conventional MRI response in recurrent glioblastoma treated with bevacizumab. Neuro Oncol. 2011;13:401-9.
106. Hegi ME, Stupp R. Witholding temozlomide in glioblastoma patients with unmethylated MGMT promoter-still a dilemma? Neuro Oncol. 2015;17:1425-7.
107. Herrlinger U, Schafer N, Steibach JP, et al. Bevacizumab plus irinotecan versus temozolomide in newly di-agnosed O6-methylguanine-DNA methylatransferase nonmethylated glioblastoma: the randomized GLARIUS trial. J Clin Oncol. 2016;34:1611-9.
108. Wick W, Gorlia T, Bady P, et al. Phase II study of radiotherapy and temsirolimus versus radiochemotherapy with temozolomide in patients with newly diagnosed glioblastoma without MGMT promoter hypermethylation (EORTC 26082). Clin Cancer Res. 2016;22:4797-4806.
109. Westphal M, Heese O, Steinbach JP, et al. A randomized, open label phase 3 trial of nimotuzumab, an anti-epidermal growth factor receptor monoclonal antibody in the treatment of newly diagnosed adult glioblastoma. Eur J Cancer. 2015;51:522-32.
110. Weller M, Butowski N, Tran DD, et al. Rindopepimut and temozolomide for patients with newly diagnosed, EGFRvIII-expressing glioblastoma (ACT IV): a randomised, double blind, international phase 3 trial. Lancet On-col. 2017;18:1373-85.
111. NIH U.S. National Library of Medicine, ClinicalTrials.gov. A study of ABT-414 in subjects with newly di-agnosed glioblastoma (GBM) with epidermal growth factor receptor (EGFR) amplification (Intellance1). https://clinicaltrials.gov/ct2/show/NCT02573324. Accessed February 26, 2019.
112. NIH U.S. National Library of Medicine, ClinicalTrials.gov. An investigational immuno-therapy study of nivolumab compared to temozolomide, each given with radiation therapy, for newly-diagnosed patients with glio-blastoma (GBM, a malignant brain cancer) (CheckMate 498). https://clinicaltrials.gov/ct2/show/NCT02617589. Accessed February 26, 2019.
113. NIH U.S. National Library of Medicine, ClinicalTrials.gov. An investigational immuno-therapy study of te-mozolomide plus radiation therapy with nivolumab or placebo, for newly diagnosed patients with glioblastoma (GBM, a malignant brain cancer) (CheckMate548). https://clinicaltrials.gov/ct2/show/NCT02667587. Accessed February 26, 2019.
114. Zhao J, Chen AX, Gartell RD, et al. Immune and genomic correlates of response to anti-PD-1 immunothera-py in glioblastoma. Nat Med. 2019 Feb 11. [Epub ahead of print]
115. Roa W, Brasher PM, Bauman G, et al. Abbreviated course of radiation therapy in older patients with glio-blastoma multiforme: a prospective randomized clinical trial. J Clin Oncol. 2004;22:1583-8.
116. Walker MD, Alexander E Jr, Hunt WE, et al. Evaluation of BCNU and/or radiotherapy in the treatment of anaplastic gliomas. A cooperative clinical trial. J Neurosurg. 1978;49:333-43.
117. Westphal M, Hilt DC, Bortey E, et al. A phase 3 trial of local chemotherapy with biodegradable carmustine (BCNU) wafers (Glaidel wafers) in patients with primary malignant glioma. Neuro Oncol. 2003;5:79-88.
118. Stupp R, Hegi ME, Gorlia T, et al. Cilengitide combined with standard treatment for patients with newly di-agnosed glioblastoma with methylated MGMT promoter (CENTRIC EORTC 26071-22072 study): a multicentre, randomized, open-label, phase 3 trial. Lancet Oncol. 2014;15:1100-8.
119. Herrlinger U, Tzaridis T, Mack F, et al. Phase III trial of CCNU/temozolomide (TMZ) combination therapy vs. standard TMZ therapy for newly diagnosed MGMT-methylated glioblastoma patients: the randomized, open-label CeTeG/NOA-09 trial. Lancet. 2019;393:678-88.
120. NIH U.S. National Library of Medicine, ClinicalTrials.gov. Temozolomide with or without veliparib in treat-ing patients with newly diagnosed glioblastoma multiforme. https://clinicaltrials.gov/ct2/show/NCT02152982. Ac-cessed February 26, 2019.
121. Liau LM, Ashkan A, Tran DD, et al. First results on survival from a large phase 3 clinical trial of an autolo-gous dendritic cell vaccine in newly diagnosed glioblastoma. J Transl Med. 2018;16:142.
122. Liau LM, Ashkan K, Tran DD, et al. Correction to: First results on survival from a large phase 3 clinical trial of an autologous dendritic cell vaccine in newly diagnosed glioblastoma. J Transl Med. 2018;16:179.
123. NIH U.S. National Library of Medicine, ClinicalTrials.gov. A phase III trial of with marizomib in patients with newly diagnosed glioblastoma. https://clinicaltrials.gov/ct2/show/NCT03345095. Accessed February 26, 2019.