No Recurrence in 971 Breast Cancer Patients With Negative SLNs Sentinel Lymph Node Biopsy
SAN ANTONIO-A negative sentinel lymph node (SLN) biopsy is an accurate indicator of the absence of nodal metastases in patients with invasive breast cancer and predicts recurrence-free survival, according to the early results of a study conducted at the H. Lee Moffitt Cancer Center and Research Institute at the University of South Florida.
SAN ANTONIOA negative sentinel lymph node (SLN) biopsy is an accurate indicator of the absence of nodal metastases in patients with invasive breast cancer and predicts recurrence-free survival, according to the early results of a study conducted at the H. Lee Moffitt Cancer Center and Research Institute at the University of South Florida.
The study tracked 971 patients who had negative SLN biopsies for a mean follow-up period of 23 months. There has been no regional or distant recurrence in any of the patients to date, Sophie Dessureault, MD, PhD, said at a general session of the 23rd Annual San Antonio Breast Cancer Symposium.
"Nodal status is the single most important prognostic factor in patients with breast cancer," Dr. Dessureault said. The standard of care for the management of invasive breast cancer has been complete axillary lymph node dissection (CALND). But sentinel lymph node biopsy is a "sensitive alternative" to CALND, she said.
Performing SLN is less expensive and reduces operative morbidity. "Complete axillary lymph node dissection is associated with nerve injury, chronic lymphedema, and other acute and chronic complications," she said.
The H. Lee Moffitt Cancer Center mapped 1,706 consecutive patients with suspected node-negative breast cancer between April 1994 and August 2000. Lymphatic mapping to identify sentinel lymph nodes was performed using Tc99m-labeled sulfur colloid and isosulfan blue dye.
The sentinel lymph node is the first node to receive lymphatic drainage from a cancer tumor, although it is not necessarily the node physically closest to the tumor, Dr. Dessureault said.
A patient may have more than one sentinel lymph node. In the study, a sentinel lymph node was defined as any blue node and/or any hot node with ex vivo radioactivity counts greater than 10 times that of an excised non-SLN or in situ radioactivity count greater than 3 times the background counts.
Lymphatic mapping was successful in 1,642 patients (96.3%). Within that group, 551 (33.6%) were found to have metastatic disease, and 1,091 (66.4%) were node negative.
The first 120 patients who were node negative underwent CALND to verify the accuracy of the SLN results. One patient was found to have metastatic disease in the nodal basin, for a false-negative rate of 0.83%. The next 971 were followed by observation alone. No cancer has recurred in this group.
Most patients treated with breast-conserving surgery had radiation therapy. Many patients received adjuvant chemotherapy. The decision to use adjuvant chemotherapy, hormonal therapy, or radiation therapy was individualized and made by a multidisciplinary team and the patient.
Dr. Dessureault emphasized that the study included all 971 patients who underwent SLN biopsy and were followed by observation alone. These patients were mapped between January 1995 and August 2000 with a mean follow-up of 23 months. The study was not skewed to focus only on patients with microscopic or T1 lesions nor did it follow only the more recent patients, she said.
"More follow-up is obviously needed, but the initial results are encouraging," Dr. Dessureault said in an ONI interview. Within the cohort of study participants, 40 patients have had more than 4 years of follow-up without an axillary recurrence, she said.
"Previous studies have reported 10-year nodal failure rates of 17% to 37% in patients treated without axillary dissection or radiation," she said. "Some studies have demonstrated that more than three quarters of patients who developed an axillary recurrence did so within 2 years."
The early results of the H. Lee Moffitt study are comparable to the results of a study reported by Giuliano et al in 2000, she said. That study also described no axillary recurrences. [See Giuliano et al: J Clin Oncol 18:2553-2559, 2000.]
Early Return to Work
Breast cancer patients who underwent SLN biopsy were far more likely to return to work in less than 4 days than patients who had complete axillary lymph node dissection, according to a prospective, nonrandomized study conducted at the Arthur G. James Cancer Hospital and Richard J. Solove Research Institute at the Ohio State University. William E. Burak, Jr., MD, and Emmanuel Zervos, MD, presented the study results at a poster session of the San Antonio symposium.
The researchers divided 96 patients who had undergone breast-conserving surgery at the James Hospital into two groups. One group consisted of patients who had a negative SLN biopsy while the second group consisted of patients who had an SLN biopsy and then underwent CALND either because their SLN biopsy was positive or they fell within the validation phase of the cancer center’s SLN biopsy protocol.
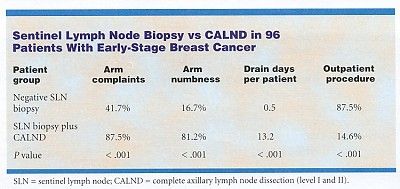
Of the group that received SLN biopsy, 70.7% returned to normal activity, including work, in less than 4 days, compared with 7.1% in the CALND group. The majority of patients who had CALND (73.8%) returned to normal activity after 7 days. Only 14.7% of the patients who had SLN biopsy took longer than 7 days to return to normal activity.
The study also found less postoperative morbidity in terms of midarm swelling, as measured by the investigators, and subjective complaints of arm numbness (see Table).