Mobile Mammography Programs Are Struggling to Survive
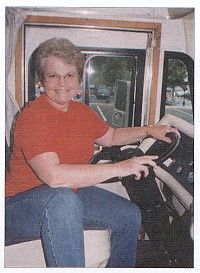
CHARLOTTE, NC-Mobile mammography programs that serve poor and working women in hard-to-reach, rural communities are an endangered species, according to Jean Griswold, founder and CEO of Mobile Health Outreach, Inc., one of the oldest surviving programs in the United States.
CHARLOTTE, NCMobile mammography programs that serve poor and working women in hard-to-reach, rural communities are an endangered species, according to Jean Griswold, founder and CEO of Mobile Health Outreach, Inc., one of the oldest surviving programs in the United States.
Rolling screening programs have higher costs than fixed-site centers, Ms. Griswold told ONI in an interview. Yet they receive the same insurance reimbursements as fixed-site facilities. These are the same reimbursements that an expert panel of the Radiological Society of North America recently blamed for closings and scale-backs in services at mammography centers around the nation.
"Mobile programs are going to be driven out of existence in many cases," Ms. Griswold said. "Mobile mammography is in crisis, and the women we serve are going to suffer. If mobile units are not out there, more women are likely to die of breast cancer."
In the case of Mobile Health Outreach, Ms. Griswold calculates that the company needs to receive $90 for every mammogram performed to reach break-even. However, they receive only $54 from Medicare, $57 from Medicaid, and similar amounts from commercial insurers.
Sometimes, Mobile Health Outreach only receives a co-payment because the organization’s policy is not to turn away walk-ins who do not have prior authorization from their insurance company. "Scheduling an appointment 2 weeks in advance is not always an option when the van is at a 1-day event or a remote site that won’t be revisited for months, a year, or even longer," she said.
Reimbursements do not cover the cost of basic services and don’t begin to cover the costs of purchasing new equipment, in particular, a new mobile van. After traveling 250,000 miles, many of them over rough mountain roads, the program’s current van is overdue for replacement at an estimated cost of $330,000. "People who set reimbursement rates have no clue what goes on in the trenches," she said. "Mammography centers are not paid enough to stay in business."
Ms. Griswold is not the first to draw attention to the special problems faced by mobile mammography centers. In 1996, the journal Radiology published results of a national survey completed by 159 mammography facilities: 30% had closed their mobile programs, and more than half of those still open were not profitable or breaking even.
Some hospital-affiliated programs can supplement screening income with revenue from follow-up services and hospitalization if needed. Independent providers rarely have that option.
Ms. Griswold credits her facility’s survival so far to "substantial personal money infusions" and a switch to nonprofit status that allows it to raise about 30% of its $750,000 annual budget from grants and donations.
She started the program in 1991 as Metrolina Outreach Mammography, Inc. to serve working women in the Carolinas and lower Virginia. A for-profit company, Metrolina went to textile mills, poultry farms, schools, and branches of banks and corporations, many of which had company-funded insurance programs that contracted its services.
In 1995, Ms. Griswold created a second company, Mobile Health Outreach, Inc, as a 501(c)(3) not-for-profit organization to serve additional populations who did not have easy access to health services, including low-income, rural, elderly, minority, and uninsured women.
Last year, after pouring more than $400,000 of their own money into Metrolina Outreach Mammography, Ms. Griswold and her husband, John Lynn, decided they could not keep the project going and consolidated their screening programs into the nonprofit company, which also provides mobile prostate screening.
In a report to the Susan G. Komen Breast Cancer Foundation, a major funding source, Mobile Health Outreach presents a dramatic picture of the rural areas it serves. In North Carolina alone, the ratio of women age 40 and over to certified mammography facilities is 6,723:1. Sixteen counties have no fixed-site mammography facilities. Statewide, the number of certified facilities dropped from 268 at the end of 1999 to 263 a year later.
Maintaining the Equipment
"We travel from the mountains to the ocean and occasionally go through some rough terrain," said Mr. Lynn, who keeps all the equipment working. An electrical engineer, he also runs his own manufacturing and health care companies.
Fixed-site mammography centers usually do preventive maintenance every 6 months on their x-ray equipment and monthly on their film processors, according to Mr. Lynn. Mobile Health Outreach services its x-ray equipment every 3 months and its processor every few weeks, he said. The added maintenance costs more, but a mechanical problem in the field can cause a major setback for the company and for the women it serves.
"If we can’t solve a problem, we have to come back [to Charlotte], and we don’t get paid for the trip," Mr. Lynn explained. Meanwhile, the women may wait months for a return visit, as the van will already be scheduled to go elsewhere. If no fixed-site facilities are nearby, most will have no alternative.
Most mobile units limit their service territory to within 50 miles of home base and shun overnight trips, Ms. Griswold said. Mobile Health Outreach has not adopted these restrictions. Nonetheless, it has reduced its service area until its aging vehicle can be replaced. "There are some areas in the mountains where I don’t want to go because repair service is difficult to get, and our staff could be stranded if there were a major mechanical failure. It could create a dangerous situation," she said. "I can’t put my people at risk."
Finding and keeping experienced technologists is a challenge for mammography centers everywhere in today’s job market, but mobile programs have an even tougher problem than fixed sites. They face the added task of finding highly independent professionals who are willing to drive the van and can make decisions on the spot if they have doubts about a mammogram’s quality.
"They have to recognize their own problems. They can’t say, "Doctor, what do I do now?’" Ms. Griswold said, citing her company’s visits to a Cherokee Indian reservation as an example. The reservation is a 5-hour drive from Charlotte, and the van stays a week. If a woman’s film is not readable, the staff can’t go back the following week to find her. They may be a hundred miles away.
Mobile Health Outreach pays its technologists approximately $42,000 annually plus benefits, Ms. Griswold said, describing salaries as skyrocketing nationwide. Radiologists do not travel with the van, but the high rate of malpractice suits for undiagnosed breast cancer has driven up their fees, too. One radiological group has already "fired" Mobile Health Outreach because its reimbursements were too low, according to Ms. Griswold, who placed the going rate nationally at $400 an hour.
Mobile Health Outreach currently works with Southeastern Radiology, a radiology group in Greensboro, NC, that used to run a mobile unit and understands the difficulties. "They work with us at a significantly discounted rate because their concern is the women," she said. Mobile Health Outreach also has case management personnel on staff who communicate with the women and their primary care doctors, doing detailed follow-up to be sure all abnormal mammograms receive attention.
‘Reason Enough’
Mobile Health Outreach’s early detection ratesix to eight breast cancers per thousand women screenedis more than double the national detection rate of one to two per thousand. To Ms. Griswold, that’s reason enough for insurance companies to increase reimbursement for mammograms. They calculate that insurers could save $500 per woman screenedmore than $3 million a yearat Mobile Health Outreach’s current screening rate of 6,000 women per year.
To compute that savings, they point to American Cancer Society statistics that show the cost of care rising from roughly $12,000 with early-stage detection to $150,000 and up for late-stage cancer.
"Insurance companies are saving money, and they’re saving lives in the long-term, but they can’t see past the short-term costs of the screening," Mr. Lynn said. "It is extremely illogical for insurance companies not to pay enough to keep mammography facilities in business, when it would save them money and save the lives of their clients."
Ms. Griswold added: "Those of us who provide mobile health services are vital to the health care of the nation, particularly in rural areas."