Peripheral T-Cell Lymphomas: Incorporating New Developments in Diagnostics, Prognostication, and Treatment Into Clinical Practice-PART 1: PTCL-NOS, FTCL, AITL, ALCL
This two-part series highlights the most important aspects of PTCLs and describes current treatment options and investigative opportunities. Part 1 will cover PTCL not otherwise specified, follicular T-cell lymphoma, angioimmunoblastic T-cell lymphoma, anaplastic large-cell lymphoma (ALCL), and breast implant–associated ALCL.
Oncology (Williston Park). 32(7):e74-e82.

Table 1. Peripheral T-Cell Lymphomas (PTCLs) According to the Current World Health Organization Classification
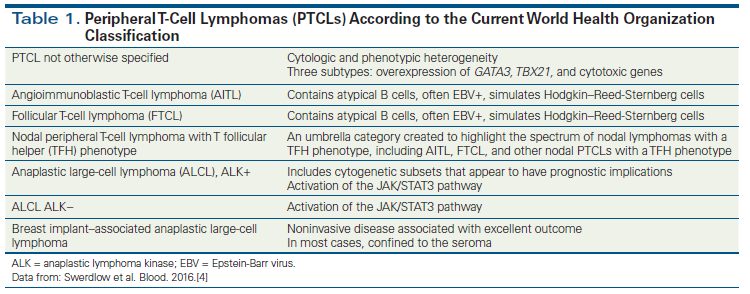
Figure 1. Epidemiologic Variability of Peripheral T-Cell Lymphomas According to Geographic Location
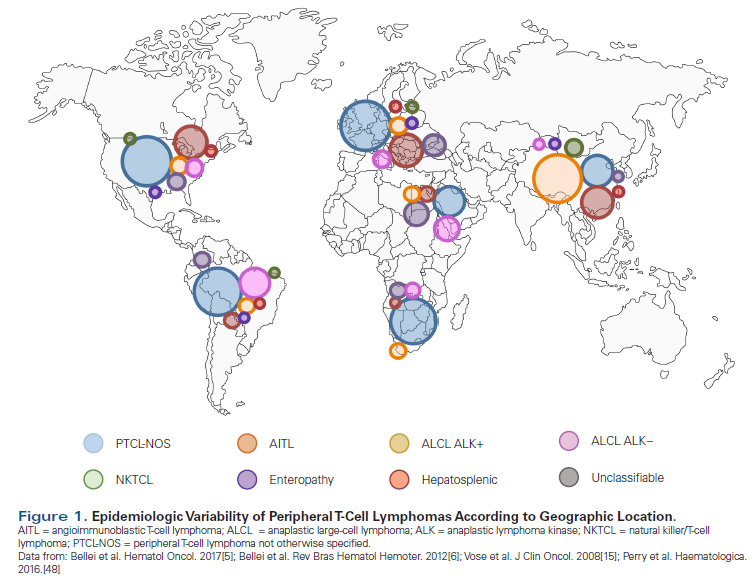
Figure 2. Treatment Algorithm for Initial Presentation of PTCL
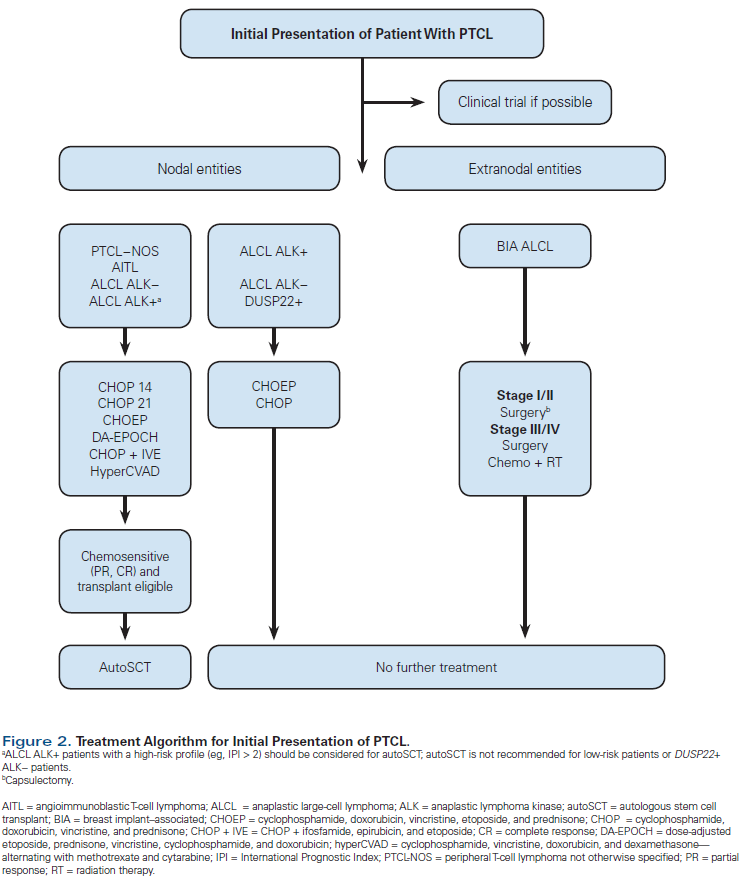
Table 2. The Prognostic Index for Peripheral T-Cell Lymphomas: Factors Associated With Worse Overall Survival
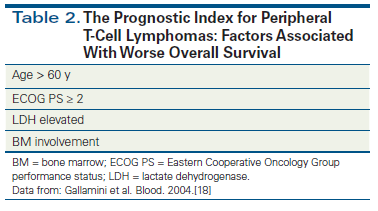
Table 3. Peripheral T-Cell Lymphomas (PTCLs) and Genetic Alterations
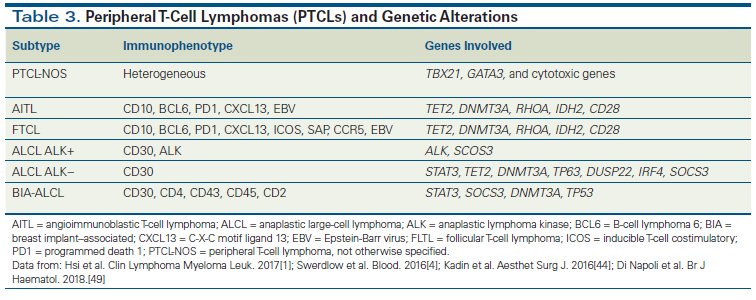
Table 4. New Drugs for Peripheral T-Cell Lymphomas
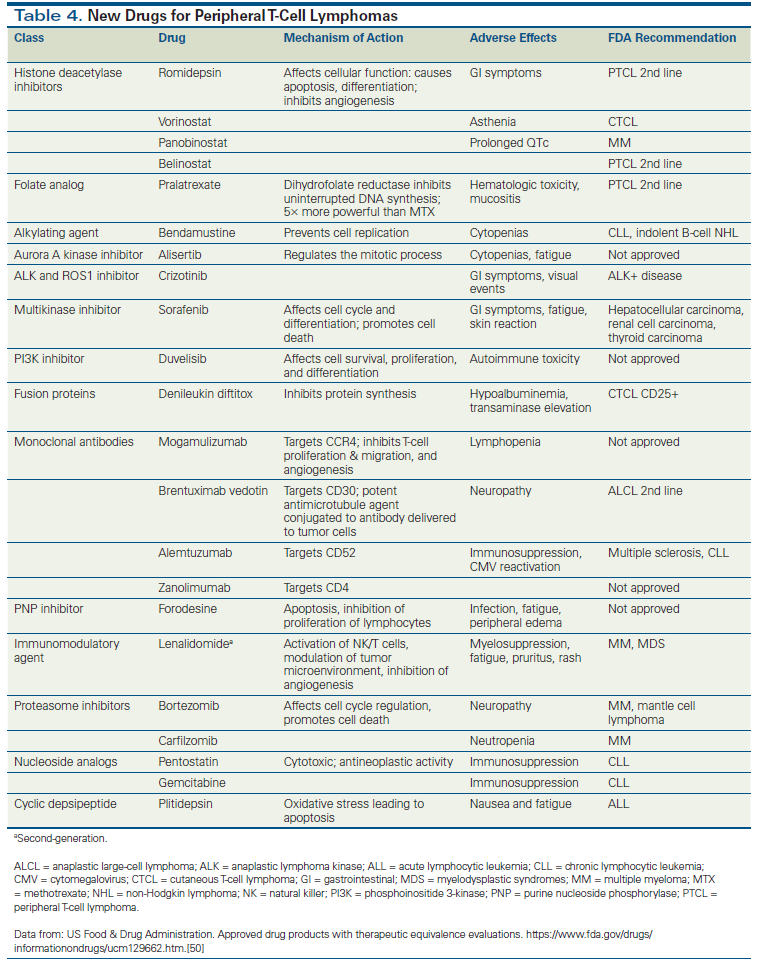
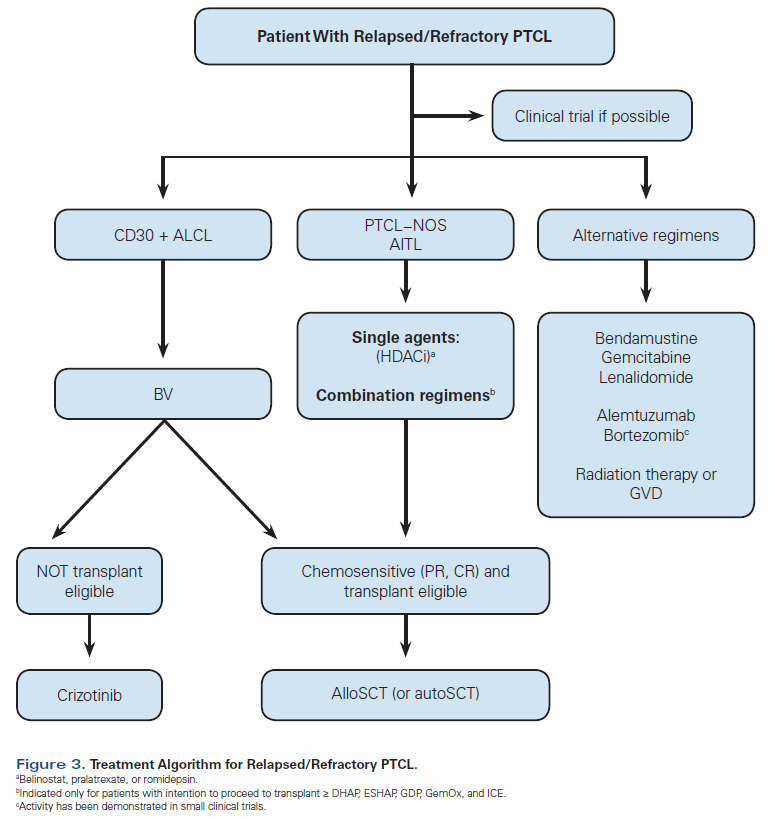
Figure 3. Treatment Algorithm for Relapsed/Refractory PTCL
Peripheral T-cell lymphomas (PTCLs) represent a heterogeneous group of diseases, with low incidence and unique epidemiology and pathobiology; they are usually clinically aggressive, with poor outcomes. There have been significant advances in our understanding of the molecular and signaling alterations seen in these malignancies. These observations have led to novel therapeutic strategies that have had a meaningful impact on outcomes. This two-part series highlights the most important aspects of PTCLs and describes current treatment options and investigative opportunities. Part 1 will cover PTCL not otherwise specified, follicular T-cell lymphoma, angioimmunoblastic T-cell lymphoma, anaplastic large-cell lymphoma (ALCL), and breast implant–associated ALCL. Part 2 will cover extranodal natural killer/T-cell lymphoma, enteropathy-associated T-cell lymphoma, indolent T-cell lymphoproliferative disorder of the gastrointestinal tract, adult T-cell leukemia/lymphoma, and hepatosplenic T-cell lymphoma.
Introduction
Peripheral T-cell lymphomas (PTCLs) constitute approximately 10% to 20% of non-Hodgkin lymphomas. They are heterogeneous, with more than 20 subtypes, including T-cell and natural killer cell diseases, and most exhibit aggressive behavior and have an unfavorable prognosis.[1-4]
PTCLs have a higher incidence in males, Caucasians, and adults aged 50 to 60 years.[5-9] Over the last decade, there has been an increase in the incidence of PTCLs, which could be partially explained by diagnostic advances and the aging of the population.[10] Several studies have demonstrated the epidemiologic variability found across different geographic populations (Figure 1). The incidence of each subtype is influenced by age, gender, and ethnicity.[3,5,8] Additional risk factors are a family history of hematologic malignancies, immune perturbations (autoimmune etiology or inflammatory response), alcoholism, and smoking.[8,9,11]
Based on clinical presentation, a PTCL may be characterized as one of four subtypes: nodal, extranodal, leukemic, or cutaneous. These subtypes differ in morphology, immunohistochemical phenotype, gene expression profile, and clinical outcome.[4,12] Part of the current World Health Organization (WHO) classification for PTCLs is described in Table 1.[4]
The complexity of the histologic classification and the low incidence explain why diagnosing PTCL is challenging.[3,13] An experienced hematopathologist is essential for an accurate diagnosis and subclassification, as is combining morphologic evaluation with immunohistochemical analysis.[1,5,14-16] Molecular and genetic studies are important tools for distinguishing subtypes.[13]
Once diagnosed, a patient’s risk should be stratified based on clinical, laboratory, and imaging findings.[13] It is crucial to consider the patient’s age, performance status, and comorbidities, because these will have an impact on treatment decisions.
The International Prognostic Index (IPI), specifically devised for assessing the prognosis of aggressive B-cell lymphomas, has also been applied to PTCL and in general correlates with overall survival (OS).[7,17] The Prognostic Index for T-cell lymphoma (PIT), developed by Gallamini et al[18] in 2004, is based on these investigators’ study of Italian patients with PTCL not otherwise specified (PTCL-NOS; Table 2). Although the PIT has already been modified, both these indexes have significant shortcomings. They were developed with small cohorts and before PTCL treatment improved, and they did not differentiate between subgroups.[10,15,18]
In general, patients with PTCL have a poor prognosis. Complete responses are expected in only half of patients, and relapses are common.[9,17] For this reason, autologous stem cell transplant (autoSCT) is often indicated in first remission.[13]
PTCL-NOS
The nodal subtypes of PTCL occur predominantly in patients from Europe and North America, and of these, PTCL-NOS is the most common histology.[8,10] The median age at presentation is approximately 60 years, with a male predominance. Clinically, most patients present with advanced disease.[13]
PTCL-NOS is not a distinct entity.[13] It can be described as an assortment of histologies with cytologic and phenotypic heterogeneity that cannot be subclassified as other PTCLs.[4,8]
Gene expression profiling has identified three subtypes of PTCL-NOS: TBX21-overexpressing, GATA3-overexpressing (associated with the worst prognosis), and PTCLs expressing other cytotoxic genes (Table 3).[3,4,19]
Conventional cytogenetic tests suggest limited recurrent karyotype abnormalities, which in most cases lack disease specificity.[6] MicroRNA profiling is being explored as another alternative for characterization and as an aid in improving our understanding of tumor biology.[16,20]
The treatment regimens developed for PTCL were derived from those designed for B-cell lymphomas.[21-24] In particular, CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone), with or without consolidation radiotherapy, is the regimen most often employed. The addition of etoposide to CHOP (CHOEP or dose-adjusted EPOCH) potentially benefits a subset of younger patients. Although adding etoposide to CHOP does not affect OS, it is associated with improved treatment-free intervals.[22-24]
Other CHOP-based combinations for first-line therapy feature the addition of alemtuzumab, denileukin diftitox, or bortezomib. Other intensive regimens include hyper-CVAD (cyclophosphamide, vincristine, doxorubicin, and dexamethasone, alternating with methotrexate and cytarabine) and ACVBP (doxorubicin, cyclophosphamide, vindesine, bleomycin, and prednisone), but to date, none of these regimens has been shown to be superior to the others.[13]
Due to the heterogeneity of PTCL-NOS and its poor outcomes, there is no standard of care for treatment.[13,25-27] However, most centers will consider consolidation with high-dose chemotherapy and autoSCT.[24]
In cases of relapsed/refractory disease, there are several options for second-line therapy (Table 4).[24] It is important to note that not all are approved by the US Food and Drug Administration for use in PTCL-NOS, and even fewer have been approved for this indication by the European Medicines Agency.
Patients with PTCL-NOS have a poor prognosis, with a 5-year OS rate of approximately 30%.[8] Those with a higher IPI score usually have an even worse OS.[13]
Follicular T-Cell Lymphoma
Initially classified as a PTCL-NOS variant, although with some clinical and morphologic features similar to those of angioimmunoblastic T-cell lymphoma (AITL), PTCL characterized by expression of follicular helper T cells has been included in the latest WHO classification as a new entity called follicular T-cell lymphoma (FTCL).[4,28] Although the majority of patients present with advanced disease, a subset has localized disease and mild symptoms.[4]
FTCL typically contains an infiltrate of monotonous lymphoid cells with round nuclei and pale cytoplasm. The lymphoma expresses pan T-cell markers with a CD4+ T helper cell phenotype (eg, PD1 [programmed death 1], CXCL13 [C-X-C motif ligand 13], BCL6 [B-cell lymphoma 6], CD10, and ICOS [inducible T-cell costimulatory]). Similar to AITL, interfollicular CD20+ B immunoblasts with Epstein-Barr virus (EBV) reactivity are present in half of cases. About 20% of cases carry a t(5;9)(q33;q22) translocation, leading to an ITK-SYK fusion that appears specific for this entity. The rarity of FTCL makes prognostication difficult, although current data suggest that 50% of patients die within 2 years.[4,28]
AITL
AITL is the second most prevalent PTCL. It occurs most often in Europe and North America in persons who are between 60 and 70 years of age.[8] Most patients are symptomatic, with lymphadenopathy, constitutional and associated B symptoms, and often with advanced-stage disease and bone marrow infiltration (more than 70% of cases).[1,2,6,7,18,29,30] AITL has a particular signature, which is associated with hepatosplenomegaly, dysgammaglobulinemia, immune compromise, and cutaneous manifestations (eg, rash).[31,32] The diagnosis often follows an immune event, such as exposure to a medication, an infection, or an allergic reaction.[33] The autoimmune phenomena typical of AITL are likely related to the similarity between neoplastic and follicular helper T cells.[34]
Pathologic diagnosis is often difficult due to the presence of atypical B cells that are often EBV-positive and simulate Reed-Sternberg cells.[34] As in Hodgkin lymphoma, neoplastic cells are in the minority and the microenvironment of AITL is composed of an infiltration of reactive small lymphocytes, eosinophils, plasma cells, epithelioid cells, immunoblasts, histiocytes, and follicular dendritic cells.[34,35] The hyperplasia of follicular dendritic cells and the high concentration of endothelial venules are also typical histologic changes of AITL; patients with FTCL usually do not have these characteristics, helping us to differentiate between the two groups.[4,8,28] However, the immunohistochemical and genetic abnormalities are similar in both, demonstrating a concordant cellular origin.[28,34] RHOA, TET2, and DNMT3A mutations are seen in the majority of patients.[36]
First-line therapy for patients with AITL remains an anthracycline-based regimen, similar to the regimen used for the majority of patients with T-cell lymphomas.[23,24] Complete responses are expected in only half of patients, and relapses are common.[9,17] For this reason, and similar to PTCL-NOS and anaplastic lymphoma kinase (ALK)-negative anaplastic large-cell lymphoma (ALCL), high-dose chemotherapy followed by autoSCT has been utilized to consolidate treatment in chemosensitive patients. Those who achieve a complete response have better outcomes. Timing of high-dose chemotherapy and autoSCT remains controversial.[7,12,21,22,30,37,38]
Older or unfit patients should not receive intensive treatment. Although cyclosporine with or without prednisone has provided some short-term benefit, results are not optimal.[13]
Patients with chemotherapy-refractory AITL, similar to those with refractory PTCL-NOS, may respond to a variety of new drugs, available as mono- or combination therapy (Table 4).[25,29,37,39]
ALCL
ALCL, in particular the ALK-positive subtype, affects a younger population (median age, 35 years).[5,8] Clinically, ALCL can be divided into three subtypes: cutaneous, systemic, and breast implant–associated (BIA).[4,8] Patients with systemic disease usually have generalized lymphadenopathy, characteristic of stage IV disease, and extranodal involvement. Bone marrow, bone, and lung are the sites most often affected.[13] Although ALCL has variable morphologic features, the presence of large, highly irregular cells with wreath-like or horseshoe-shaped nuclei is a hallmark.[40]
CD30 and ALK protein expression are the signature markers of this distinctive entity; these give ALCL unique clinical features and a distinctive prognosis. The rearrangement of the ALK gene is a classic biomarker, present in > 50% of ALCLs and with prognostic significance. The most common rearrangement-t(2;5)(p23;q35)-creates a fusion gene composed of nucleophosmin and ALK.[13] Patients with ALK-positive ALCL have a higher OS rate than ALK-negative patients (OS at 5 years: 70% vs 49%).[8,20,41] However, this survival difference is not seen in patients younger than 40 years.[13]
Other prognostic markers, seen in ALK-negative ALCL, are rearrangements of DUSP22 and T63; these are associated with a better and worse prognosis, respectively.[20]
The CHOP-like regimens are also used for ALCL, as first-line treatment in both ALK-positive and ALK-negative patients.[23,37] Patients with ALK-positive ALCL typically have a good outcome.[23,24] For this reason, autoSCT is only indicated for relapse.[37,42] AutoSCT can be considered in ALK-negative patients without rearrangement of DUSP22 (Table 2). To achieve more consistent and durable responses in the first line, studies have explored combining new drugs, such as brentuximab vedotin (an anti-CD30 immunoconjugate) and crizotinib (oral ALK inhibitor), with CHOP. Targeted agents are also used for salvage treatment.[12,29,30,39]
BIA-ALCL
The correlation between breast implants and ALCL has recently been recognized, and BIA-ALCL has been incorporated into the WHO classification as a new provisional entity (Table 1).[4] Different from primary breast lymphoma, BIA-ALCL does not compromise the parenchyma; it presents clinically as a localized seroma involving the implant and is associated with pain and swelling.[4,11] A minority of patients may present with a mass, and in these cases the disease is much more aggressive.[40,43] Irrespective of presentation, systemic symptoms are rare.[44]
There are several theories regarding the etiology and pathogenesis of this rare entity. An inadequate response of the immune system to the implant could explain the lymphomatous proliferation.[43] Implants with a more textured surface are more susceptible to bacterial proliferation, which activates lymphocytes and causes a chronic inflammatory process secondary to a bacterial biofilm infection around the implant. Currently, this is the most compelling theory that has been put forth to explain the development of BIA-ALCL.[43,44] Ralstonia species, gram-negative bacilli found in soil and water, have been associated with nosocomial infections, especially implant-related infection.[11,43]
Similar to ALK-negative ALCL, BIA-ALCL has an anaplastic morphology, with an immunophenotype that includes expression of CD30, CD4, CD43, CD45, and CD2, and the absence of ALK.[11,44] The expression of SOCS3 (suppressor of cytokine signaling 3) is also identified in BIA-ALCL cases, as in systemic ALCL.[44]
Most often, complete surgical excision, including removal of the implant and capsulectomy, results in an excellent outcome.[40] In contrast, when the lymphoma invades the capsule or is systemic, primary treatment should be complemented with chemotherapy. In these cases, relapse is not uncommon and the prognosis is worse.[11]
How to Make a Treatment Decision
To help in therapeutic decision making, there are algorithms based on diagnosis, molecular characterization, and prognosis that provide treatment options for newly diagnosed and relapsed/refractory patients. As mentioned, autoSCT is very important in treatment of PTCL; therefore, the distinction between patients who are “fit/eligible” and those who are “unfit/ineligible” for autoSCT is fundamental when deciding on the best therapeutic approach.[38]
In very unfit or frail patients, delivery of optimal therapy may be impossible; thus, alternative palliative treatments must be considered.[29,38]
Allogeneic Stem Cell Transplantation
Despite the availability of several new drugs, salvage therapy remains a challenge. So far, with the vast majority of new compounds (with the exception of brentuximab vedotin), only short-lasting remissions have been achieved in ALCL. In contrast, allogeneic stem cell transplantation (alloSCT) seems to be associated with promising outcomes (the 5-year freedom from relapse and OS rates are about 50%). AlloSCT should be considered mainly in younger patients with a human leukocyte antigen–matched sibling donor.[13,45] In this context, these new drugs may assume the role of a bridge to transplantation.[45]
However, there are challenges related to alloSCT, including patient eligibility, donor availability, and treatment-related toxicity and mortality; these affect about 40% of cases.[45-47] Advances in alloSCT include an extension of the donor pool-utilizing matched unrelated donors, umbilical stem cell transplants, and haploidentical transplants-to ensure sources for more patients. Reduced-intensity conditioning nonmyeloablative transplants have extended the age and comorbidities of patients who may be considered as candidates for treatment. Improvements in the management of graft vs host disease and the infusion of donor lymphocytes at the time of residual disease and/or relapse have also had a profound effect.[25]
Currently, alloSCT has to be considered for patients with bone marrow involvement, those in partial remission, and those with relapsed/refractory disease. Advances in clinical care, eg, reduced-intensity conditioning and management of graft-vs-host disease, have been associated with a lower mortality rate, making alloSCT a more realistic approach for PTCL patients.[25]
It is important to emphasize that patients with active disease at transplant have worse outcomes, impacting OS.[25] Before advocating transplantation, one must take into account a patient’s performance status and comorbidities.[29,38]
Conclusions
The low incidence and heterogeneity of PTCLs pose a significant challenge in developing effective therapies. Fortunately, advances in our understanding of the critical pathways, the cellular targets, and the role of the microenvironment in these diseases have led to the emergence of both small-molecule agents and biologic approaches that may have a profound impact on their prognosis. In addition, important strides in immunotherapy, including chimeric antigen receptor T-cell therapy and checkpoint inhibitors, potentially in conjunction with stem cell transplantation, hold great promise. PTCLs lend themselves to the application of precision medicine and may serve as a paradigm for future investigators.
Financial Disclosure:Dr. Zain serves as a consultant for Spectrum Pharmaceuticals, and serves as a consultant and on the speakers bureau for Seattle Genetics. The other authors have no significant financial interest in or other relationship with the manufacturer of any product or provider of any service mentioned in this article.
References:
1. Hsi ED, Horwitz SM, Carson KR, et al. Analysis of peripheral T-cell lymphoma diagnostic workup in the United States. Clin Lymphoma Myeloma Leuk. 2017;17:193-200.
2. Al-Zahrani M, Savage KJ. Peripheral T-cell lymphoma, not otherwise specified: a review of current disease understanding and therapeutic approaches. Hematol Oncol Clin North Am. 2017;31:189-207.
3. Abouyabis AN, Shenoy PJ, Lechowicz MJ, Flowers CR. Incidence and outcomes of the peripheral T-cell lymphoma subtypes in the United States. Leuk Lymphoma. 2008;49:2099-107.
4. Swerdlow SH, Campo E, Pileri SA, et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016;127:2375-90.
5. Bellei M, Sabattini E, Pesce EA, et al. Pitfalls and major issues in the histologic diagnosis of peripheral T-cell lymphomas: results of the central review of 573 cases from the T-Cell Project, an international, cooperative study. Hematol Oncol. 2017;35:630-6.
6. Bellei M, Chiattone CS, Luminari S, et al. T-cell lymphomas in South America and Europe. Rev Bras Hematol Hemoter. 2012;34:42-7.
7. Carson KR, Horwitz SM, Pinter-Brown LC, et al. A prospective cohort study of patients with peripheral T-cell lymphoma in the United States. Cancer. 2017;123:1174-83.
8. Phan A, Veldman R, Lechowicz MJ. T-cell lymphoma epidemiology: the known and unknown. Curr Hematol Malig Rep. 2016;11:492-503.
9. Teras LR, DeSantis CE, Cerhan JR, et al. 2016 US lymphoid malignancy statistics by World Health Organization subtypes. CA Cancer J Clin. 2016 Sep 12. [Epub ahead of print]
10. Petrich AM, Helenowski IB, Bryan LJ, et al. Factors predicting survival in peripheral T-cell lymphoma in the USA: a population-based analysis of 8802 patients in the modern era. Br J Haematol. 2015;168:708-18.
11. Clemens MW, Miranda RN. Coming of age: breast implant-associated anaplastic large cell lymphoma after 18 years of investigation. Clin Plast Surg. 2015;42:605-13.
12. Coiffier B, Federico M, Caballero D, et al. Therapeutic options in relapsed or refractory peripheral T-cell lymphoma. Cancer Treat Rev. 2014;40:1080-8.
13. Armitage JO. The aggressive peripheral T-cell lymphomas: 2017. Am J Hematol. 2017;92:706-15.
14. Sholl LM, Longtine J, Kuo FC. Molecular analysis of genetic markers for non-Hodgkin lymphomas. Curr Protoc Hum Genet. 2017;93:10.4.1-.29.
15. Vose J, Armitage J, Weisenburger D; Project IT-CL. International peripheral T-cell and natural killer/T-cell lymphoma study: pathology findings and clinical outcomes. J Clin Oncol. 2008;26:4124-30.
16. Lin Y, Chen WM, Wang C, Chen XY. MicroRNA profiling in peripheral T-cell lymphoma, not otherwise specified. Cancer Biomark. 2017;18:339-47.
17. Bellei M, Nabhan C, Pesce EA, et al. The value and relevance of the T cell lymphoma registries and international collaborations: the case of COMPLETE and the T-Cell Project. Curr Hematol Malig Rep. 2015;10:448-55.
18. Gallamini A, Stelitano C, Calvi R, et al. Peripheral T-cell lymphoma unspecified (PTCL-U): a new prognostic model from a retrospective multicentric clinical study. Blood. 2004;103:2474-9.
19. Laginestra MA, Piccaluga PP, Fuligni F, et al. Pathogenetic and diagnostic significance of microRNA deregulation in peripheral T-cell lymphoma not otherwise specified. Blood Cancer J. 2014;4:259.
20. Wang X, Boddicker RL, Dasari S, et al. Expression of p63 protein in anaplastic large cell lymphoma: implications for genetic subtyping. Hum Pathol. 2017;64:19-27.
21. Burudpakdee C, Lin HM, Wang W, et al. Clinical and economic burden of peripheral T-cell lymphoma in commercially insured patients in the United States: findings using real-world claims data. J Med Econ. 2016;19:965-72.
22. Broccoli A, Zinzani PL. Peripheral T-cell lymphoma, not otherwise specified. Blood. 2017;129:1103-12.
23. Horwitz SM, Zelenetz AD, Gordon LI, et al. NCCN guidelines insights: non-Hodgkin’s lymphomas, version 3.2016. J Natl Compr Canc Netw. 2016;14:1067-79.
24. NCCN Clinical Practice Guidelines in Oncology. T-cell lymphoma. Version 4.2018. https://www.nccn.org/professionals/physician_gls/pdf/cll.pdf. Accessed June 24, 2018.
25. Zain J, Palmer JM, Delioukina M, et al. Allogeneic hematopoietic cell transplant for peripheral T-cell non-Hodgkin lymphoma results in long-term disease control. Leuk Lymphoma. 2011;52:1463-73.
26. Zain J, O’Connor OA. New strategies to optimize outcomes in patients with T-cell lymphoma. Clin Lymphoma Myeloma Leuk. 2010;10(suppl 2):S84-S87.
27. Iyer SP, Foss FF. Romidepsin for the treatment of peripheral T-cell lymphoma. Oncologist. 2015;20:1084-91.
28. Pileri SA. Follicular helper T-cell-related lymphomas. Blood. 2015;126:1733-4.
29. Zhang Y, Xu W, Liu H, Li J. Therapeutic options in peripheral T cell lymphoma. J Hematol Oncol. 2016;9:37.
30. Lage LA, Cabral TC, Costa RO, et al. Primary nodal peripheral T-cell lymphomas: diagnosis and therapeutic considerations. Rev Bras Hematol Hemoter. 2015;37:277-84.
31. Ma H, Abdul-Hay M. T-cell lymphomas, a challenging disease: types, treatments, and future. Int J Clin Oncol. 2017;22:18-51.
32. Sakata-Yanagimoto M, Nakamoto-Matsubara R, Komori D, et al. Detection of the circulating tumor DNAs in angioimmunoblastic T-cell lymphoma. Ann Hematol. 2017;96:1471-5.
33. Mosalpuria K, Bociek RG, Vose JM. Angioimmunoblastic T-cell lymphoma management. Semin Hematol. 2014;51:52-8.
34. Lemonnier F, Mak TW. Angioimmunoblastic T-cell lymphoma: more than a disease of T follicular helper cells. J Pathol. 2017;242:387-90.
35. Matsumoto Y, Nagoshi H, Yoshida M, et al. Expression of master regulators of T-cell, helper T-cell and follicular helper T-cell differentiation in angioimmunoblastic T-cell lymphoma. Intern Med. 2017;56:2851-6.
36. Fukumoto K, Nguyen TB, Chiba S, Sakata-Yanagimoto M. Review of the biologic and clinical significance of genetic mutations in angioimmunoblastic T-cell lymphoma. Cancer Sci. 2017;109:490-6.
37. Moskowitz AJ, Lunning MA, Horwitz SM. How I treat the peripheral T-cell lymphomas. Blood. 2014;123:2636-44.
38. Ellin F, Jerkeman M, Törnqvist J, et al. Impact of comorbidity on survival in peripheral T-cell lymphomas: a Swedish Lymphoma Registry study. Hematol Oncol. 2018;36:159-65.
39. Marchi E, Raufi AG, O’Connor OA. Novel agents in the treatment of relapsed or refractory peripheral T-cell lymphoma. Hematol Oncol Clin North Am. 2017;31:359-75.
40. Hapgood G, Savage KJ. The biology and management of systemic anaplastic large cell lymphoma. Blood. 2015;126:17-25.
41. Parrilla Castellar ER, Jaffe ES, Said JW, et al. ALK-negative anaplastic large cell lymphoma is a genetically heterogeneous disease with widely disparate clinical outcomes. Blood. 2014;124:1473-80.
42. Kharfan-Dabaja MA, Kumar A, Ayala E, et al. Clinical practice recommendations on indication and timing of hematopoietic cell transplantation in mature T-cell and NK/T-cell lymphomas: an international collaborative effort on behalf of the Guidelines Committee of the American Society for Blood and Marrow Transplantation. Biol Blood Marrow Transplant. 2017;23:1826-38.
43. Hu H, Johani K, Almatroudi A, et al. Bacterial biofilm infection detected in breast implant-associated anaplastic large-cell lymphoma. Plast Reconstr Surg. 2016;137:1659-69.
44. Kadin ME, Deva A, Xu H, et al. Biomarkers provide clues to early events in the pathogenesis of breast implant-associated anaplastic large cell lymphoma. Aesthet Surg J. 2016;36:773-81.
45. Chihara D, Fanale MA, Miranda RN, et al. The survival outcome of patients with relapsed/refractory peripheral T-cell lymphoma-not otherwise specified and angioimmunoblastic T-cell lymphoma. Br J Haematol. 2017;176:750-8.
46. Corradini P, Dodero A, Zallio F, et al. Graft-versus-lymphoma effect in relapsed peripheral T-cell non-Hodgkin’s lymphomas after reduced-intensity conditioning followed by allogeneic transplantation of hematopoietic cells. J Clin Oncol. 2004;22:2172-6.
47. Wei J, Xu J, Cao Y, et al. Allogeneic stem-cell transplantation for peripheral T-cell lymphoma: a systemic review and meta-analysis. Acta Haematol. 2015;133:136-44.
48. Perry AM, Diebold J, Nathwani BN, et al. Non-Hodgkin lymphoma in the developing world: review of 4539 cases from the International Non-Hodgkin Lymphoma Classification Project. Haematologica. 2016;101:1244-50.
49. Di Napoli A, Jain P, Duranti E, et al. Targeted next generation sequencing of breast implant-associated anaplastic large cell lymphoma reveals mutations in JAK/STAT signalling pathway genes, TP53 and DNMT3A. Br J Haematol. 2018;180:741-4.
50. US Food & Drug Administration. Approved drug products with therapeutic equivalence evaluations. 38th ed. https://www.fda.gov/drugs/informationondrugs/ucm129662.htm. Accessed June 26, 2018.
Navigating AE Management for Cellular Therapy Across Hematologic Cancers
A panel of clinical pharmacists discussed strategies for mitigating toxicities across different multiple myeloma, lymphoma, and leukemia populations.