Perioperative Treatment of Gastrointestinal Stromal Tumors
Gastrointestinal stromal tumors (GISTs) originate from the interstitial cells of Cajal or a precursor and are the most common mesenchymal neoplasms of the gastrointestinal (GI) tract.[1] Although GISTs often present as localized masses, they are typified by a high risk of metastatic relapse, most commonly in the liver and peritoneum.
This review describes the current multidisciplinary management of gastrointestinal stromal tumor (GIST), which is the most common sarcoma of the gastrointestinal tract. Before 2001, surgery was the only effective therapy for GIST. The discovery of the central role of KIT proto-oncogene mutations in the pathogenesis of this tumor, and the development of specific inhibitors of KIT tyrosine kinase (TK) function, has changed the paradigm of treatment for GISTs. Imatinib and sunitinib are TK inhibitors with activity against GISTs. Their major established role in GIST is in the treatment of advanced disease. A growing body of literature and clinical experience support the potential perioperative use of these drugs. The adjuvant use of imatinib is based on retrospective series and limited prospective studies demonstrating that imatinib reduces the risk of recurrence. Ongoing studies are further defining the length of adjuvant therapy, as well as identifying the patients that could achieve the best results. Neoadjuvant treatment often decreases the tumor size, allowing a less morbid surgery, appears to be safe and beneficial for some patients, and therefore deserves further study.
Gastrointestinal stromal tumors (GISTs) originate from the interstitial cells of Cajal or a precursor and are the most common mesenchymal neoplasms of the gastrointestinal (GI) tract.[1] Although GISTs often present as localized masses, they are typified by a high risk of metastatic relapse, most commonly in the liver and peritoneum. The pathologic characterization of GIST as a unique form of GI sarcomas was first described in 1983 by Mazur and Clark.[2] Subsequently Nishida et al,[3] Hirota et al,[4] and later Heinrich[5] demonstrated that GISTs often possess activating mutations in the KIT or platelet-derived growth factor receptor (PDGFR) proto-oncogenes. The identification of these mutations and their relationships with the genesis and progression of GISTs allowed for the development of effective, targeted therapeutic drugs, strongly improving the prognosis of this disease.[6,7]
Epidemiology
Knowledge about the epidemiology of GIST has advanced markedly over the past few years. However, the true frequency of these tumors is unknown. Epidemiologic data are difficult to interpret because the early definition of GIST was derived from criteria published in 1990, and before this, GISTs were often histologically misclassified as other mesenchymal neoplasms derived from soft tissues, especially leiomyosarcomas.
In general, GISTs tend to have low growth rates, with a subsequent long time to the development of symptoms. It is no surprise, therefore, that small GISTs may remain undetected for protracted periods of time and may never progress to symptomatic or metastatic disease.
The most reliable data are derived from recent population-based studies. Investigators in Iceland examined all patients diagnosed in that country with a gastrointestinal mesenchymal tumor from 1990 to 2003. These patients were evaluated with an immunohistochemical panel including staining for c-kit, confirming an incidence rate of 11 per million.[8] Similarly, Swedish scientists investigated all potential cases of GIST diagnosed between 1983 and 2000, reporting an incidence rate of 14.5 per million, and a prevalence rate of 129 per million.[9]
Japanese investigators studied 100 patients whose whole stomachs were resected due to gastric cancer. The organs were sectioned at 5-mm intervals and examined by light microscopy and immunochemistry for KIT (CD117). They found 50 microscopic GISTs in a sample of 35 individuals, and 90% were located in the upper stomach. The authors suggested that, considering the annual incidence of clinical GIST, only a few microscopic GISTs grow into a clinically meaningful size with malignant potential.[10]
A study based on the US Surveillance, Epidemiology and End Results (SEER) registry data from 1992 to 2000 found the age-adjusted yearly incidence of GIST to be 6.8 per million, although that number has been questioned as being too low.[11] The incidence of GISTs has substantially changed over time, possibly due to the constant evolution of the diagnostic criteria and the improvement in diagnostic methods, which allows for earlier and more complete detection.
Estimation of Recurrence Risk
The estimation of recurrence risk following complete resection of GIST is of paramount importance when selecting patients who could possibly benefit from adjuvant therapy. In the past decade, several different criteria have been proposed to classify malignant potential. Although the initial diagnosis of GIST may rely heavily on molecular characteristics, the mitotic rate and tumor size, with or without location of the primary tumor, have gained the greatest acceptance as being predictive of outcome. Certainly the terms benign and malignant should not be applied to GISTs, since they all have the potential to recur and/or metastasize.
In a landmark study, DeMatteo et al reported on 200 GIST patients referred to Memorial Sloan-Kettering Cancer Center,[12] 80 of whom had localized disease and underwent a complete resection. A total of 65 (81%) of these patients had negative microscopic margins. All patients were followed prospectively. In patients who underwent complete resection of gross disease, the 5-year survival rate was 54%. Data regarding the pattern of recurrence were available for 27 patients. Local recurrence alone occurred in 9 (33%), metastasis alone in 13 (48%), and both in 5 (19%) patients. Recurrence was predominantly intra-abdominal. On multivariate analysis, only tumor size greater than 10 cm was a significant risk factor for recurrence, with a relative risk of 2.5 (confidence interval [CI] = 1.2–5.5).
Recently, the same authors published an extended review with similar results regarding tumor size, but this time exploring the mitotic index, which is considered another classic risk factor. After a median follow-up of 4.7 years, recurrence-free survival was 83%, 75%, and 63% at 1, 2, and 5 years, respectively. On multivariate analysis, recurrence was predicted by > 5 mitoses/50 high-power fields (HPF), tumor size > 10 cm, and tumor location (with the worst outcomes in patients with small bowel GIST). A high mitotic rate conferred the most important risk factor, with a hazard rate of 14.6 (95% CI = 6.5–32.4).
The Armed Forces Institute of Pathology studied 1,765 cases of gastric GIST and demonstrated that the outcome was strongly related to tumor size and mitotic activity. Less than 3% of tumors smaller than 10 cm and with fewer than 5 mitoses/50 HPFs metastasized, whereas 86% of tumors > 10 cm and > 5 mitoses/50 HPFs metastasized. However, tumors > 10 cm with mitotic activity < 5/50 HPFs and those < 5 cm with mitoses > 5/50 HPFs had a relatively low metastatic rate (11% and 15%, respectively). Tumor location in the fundus or in the gastroesophageal junction, coagulative necrosis, ulceration, and mucosal invasion were significant unfavorable factors (P < .001), whereas tumor location in the antrum was favorable (P < .001).[13]
TABLE 1
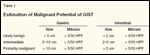
Estimation of Malignant Potential of GIST
The same group also reported on 906 patients with small bowel GIST. In this review, tumor-related mortality was 39%-twice what was observed in the gastric GIST review. A similarly strong correlation was seen between outcome and both tumor size and mitotic activity (Table 1). Fewer than 3% of tumors < 5 cm and ≤ 5 mitoses/50 HPF metastasized, whereas distant spread was observed in 86% of tumors > 10 cm and > 5 mitoses/50 HPF. However, in stark contrast to the corresponding intermediate-risk gastric tumors, small bowel tumors > 10 cm with mitotic activity ≤ 5/50 HPF and those ≤ 5 cm with mitoses > 5/50 HPF had a high metastatic rate (> 50%). Even tumors > 5 cm ≤ 10 cm with a low mitotic rate had a 24% metastatic rate.[14]
TABLE 2
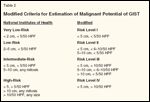
Modified Criteria for Estimation of Malignant Potential of GIST
In general, tumors arising from the small bowel, colon, rectum, or mesentery are generally associated with less favorable outcomes than those arising from the stomach.[15,16] Thus, based on the more recent review, the most commonly used criteria to assess the risk of recurrence include the primary tumor diameter, the mitotic count, and the location of the resected tumor.[15] Additionally, other factors may be prognostic. Patients whose tumors have ruptured into the abdominal cavity have a very high risk of tumor recurrence.[7] Recently, Huang et al reviewed the data from 289 patients with localized GIST and proposed a modification in the consensus risk stratification.[17] Very low-risk and low-risk GISTs were combined into a single new risk level I group, and intermediate-risk GISTs were designated as risk level II. GISTs > 5 cm with > 10 mitoses/50 HPF were designated risk level IV. All other high-risk GISTs were defined as risk level III. The cumulative 5-year rate of disease-specific survival for patients with GISTs classified as risk levels I to IV were 100%, 96%, 67%, and 25% at 5 years, respectively. Despite the relatively small study population, the differences in outcome were striking between patients in risk level II and III (P < .0001) and between those in risk level III and IV (P = .0002).[17] These impressive results suggest that this new prognostic criteria could be superior to the commonly used National Institutes of Health consensus criteria, especially to stratify high-risk patients (Table 2).[18]
Basis for Treatment With Imatinib
rosine kinase (TK) inhibitor that blocks KIT- or PDGFR-alpha polypeptide (PDGFRA)-mediated signaling. The incorporation of this drug into early GIST trials completely changed the treatment for this disease. Imatinib obstructs signaling by binding to the ATP pocket required for phosphorylation and activation of the TK receptor. Imatinib was first approved for the treatment of chronic myelogenous leukemia,[19,20] in which an aberrant TK (bcr-ABL) results from molecular rearrangement. The finding that mutational activation of KIT stimulates growth of GIST cancer cells, coupled with imatinib’s ability to preclinically inhibit KIT in GIST cell lines,[21] led to the development of several clinical investigations. These started with a successful case report,[22] which was quickly followed by phase II and III studies.
Van Oosterom and colleagues reported the results of a phase I trial that included patients with metastatic GIST, demonstrating that doses up to 400 mg twice a day were tolerable, with an outstanding 82% overall clinical benefit and a very acceptable toxicity profile. The most common side effects were periorbital edema (40%), peripheral edema (37.5%), fatigue (30%), skin rash (30%), and nausea/vomiting (25%). Myelosuppression was also seen occasionally.[23]
Demetri and associates conducted a phase II trial randomizing 147 patients to receive imatinib at 400 or 600 mg daily. A total of 79 patients (53.7 %) had a partial response, 41 patients (27.9 %) had stable disease, and responses could not be evaluated in 7 patients (4.8%). No significant differences were seen in toxicity or response between the two doses.[24] This group recently published the long-term results from this trial.[25] In 71 months, 2 patients (1.4%) achieved a complete response and 98 (66.7%) had a partial response, for a total response rate of 68.1%. A total of 23 patients (15.6%) had prolonged stable disease for more than 1 year. The median duration of response was 29 months, and the median survival was 57 months for all patients. Overall, 46 patients (31% of the original cohort) were still taking imatinib at 5 years.[25]
Phase III trials have been conducted to determine ideal treatment duration[26] and optimal dose.[27,28] Most recently, important data from a meta-analysis of two large trials included two nearly identical randomized studies comparing 400 mg of daily imatinib to 800 mg daily for the treatment of incurable GIST. A total of 1,640 patients were included, with the analysis showing a small progression-free survival advantage for high-dose imatinib, but no overall survival advantage.[29] Interestingly, the progression-free survival benefit derived solely from patients with exon 9 mutations.
Based on such data, the current standard imatinib regimen for metastatic GIST remains a daily dose of 400 mg, given continuously, except for exon 9 patients, who should quickly be dose-escalated to 800 mg daily (see below). The results yielded by the use of imatinib against GIST represented a dramatic paradigm shift away from ineffectual chemotherapy, and highlighted the potential of TK inhibitors as a treatment for solid cancers.
Tumor Genotype and Response to Therapy
Since GISTs commonly possess activating mutations in KIT or PDGFR, information about the influence of genetic subtype on the clinical response to imatinib has been of great interest. An early publication was based on the 127 patients enrolled in the phase II clinical study of imatinib detailed above.[30] Archival pretreatment pathology specimens were obtained from those patients, sections were prepared from formalin-fixed, paraffin-embedded pretreatment specimens trimmed to enrich for tumor cells. Polymerase chain reaction amplification of genomic DNA for KIT and PDGFRA was performed, and amplicons were analyzed for mutations. Mutation types were clearly correlated with clinical outcome. Activating mutations of KIT or PDGFRA were found in 112 (88.2%) and 6 (4.7%) patients, respectively. Most KIT mutations involved exon 9 (n = 23) or exon 11 (n = 85).
In patients with GISTs harboring exon 11 KIT mutations, the partial response rate was 83.5%, whereas patients with tumors containing an exon 9 KIT mutation had a partial response rate of 47.8% (P = .0006). No responses were observed in patients with PDGFR mutations or no detectable mutation of KIT. Patients whose tumors contained exon 11 KIT mutations had a longer event-free and overall survival than those whose tumors expressed exon 9 KIT mutations or had no detectable kinase mutation.[30,31]
Later published data confirmed the importance of genotype regarding the response rate and overall outcomes in GIST, but with different conclusions. In the European-Australasian phase III study, pretreatment tumor specimens from 377 patients were analyzed for mutations of KIT and PDGFRA (when KIT-negative). Activating KIT mutations were detected in 315 of 377 tumors (83.6%), including mutations of exon 11 in 248 (65.8%), exon 9 in 58 (15.4%), exon 13 in 6 (1.6%), and exon 17 in 3 (0.8%). PDGFRA genotyping performed for 62 tumors without activating KIT mutations identified PDGFRA mutants in 10 (16.1%), usually involving point mutations or deletions in exon 18.[32,33]
In the North American randomized phase III trial, KIT mutations were identified in 280 patients (86.4%) and PDGFRA mutations in 3 (0.9%). A total of 41 patients demonstrated no KIT or PDGFRA mutations. Clinical response to imatinib was related to tumor mutational status in both phase III studies. Response rates for patients with mutations on KIT exon 11 or exon 9, or without KIT and PDGFRA mutations were respectively 69%, 34%, and 25% in the European-Australasian study, and 67%, 40%, and 39% in the North American trial.[34]
It is clear that the patients who achieve the best response rates with imatinib are those with exon 11 mutations. Those with exon 9 mutations may derive some benefit from higher initial imatinib doses, with an increased response rate and a possible benefit in overall survival. In addition, about one-third of patients with PDGFR mutations may respond to imatinib therapy.[35]
Response Criteria
Response Evaluation Criteria in Solid Tumors (RECIST) remains the most commonly used system to define objective responses in GIST. This standard measures only the longest diameter of the lesions, with a partial response being defined as a 30% decrease in the sum of the longest dimensions of the measurable tumors. Progressive disease is defined as a 20% increase in the tumor length.[36] However, it is rapidly becoming evident that the RECIST criteria are inappropriate to follow GIST responses to the new TK inhibitors, which may induce an early decrease in tumor density, with size increase, followed only later by a slow regression in tumor size.
There has been great interest in evaluating the metabolism of tumors treated with imatinib and other TK inhibitors using 18F-fluorodeoxyglucose positron-emission tomography (FDG-PET). Early data have demonstrated that FDG-PET is very sensitive in detecting early responses, as quickly as after a single dose of treatment.[37] In one small study, 17 patients with GIST received 400 mg/d of imatinib. An FDG-PET response was observed in 13 patients (11 complete responders and 2 partial responders). A subsequent computed tomography (CT) response by RECIST was confirmed in 10 of those 11 patients. FDG-PET–stable or progressive disease was observed in eight patients, none of whom achieved a subsequent response by conventional tomography. An FDG-PET response was also associated with a longer progression-free survival (92% vs 12% at 1 year, P = .00107).[38] However, FDG-PET is still expensive and unavailable in many areas of the world, generating great interest in new tomography modalities that could yield similar results.
Recently, Choi and colleagues conducted a study to evaluate whether specific CT findings of GIST after imatinib treatment correlated with tumor responses by FDG-PET. A total of 40 patients with metastatic GIST treated with imatinib were evaluated with both imaging techniques, and a multivariate analysis was performed using tumor size and density (Hounsfield unit) on CT, and maximum standardized uptake value (SUV) on FDG-PET. A decrease in tumor size of more than 10% or a decrease in tumor density of more than 15% on CT had a sensitivity of 97% and a specificity of 100% in identifying FDG-PET responders vs 52% and 100% when RECIST criteria were used. Such data suggest that CT using the new Choi criteria is an excellent method of assesing treatment response in GIST, with a far lower cost than using FDG-PET.[39,40]
Adjuvant Therapy
In modern oncology, the term adjuvant therapy usually applies to treatment given in addition to surgery, usually following resection, when all detectable disease has been removed. Considering the strong data supporting the use of imatinib as a treatment for metastatic GIST, the favorable safety profile associated with its use, and the high recurrence rate associated with this tumor even following complete resection, a strong theoretical basis existed for the investigation of imatinib after resection in patients with GIST.[41,42]
An early phase II trial assessed 107 patients with high-risk KIT-expressing resected primary GIST. These patients were treated with 1 year of imatinib, 400 mg/d, starting 2 months after surgical resection. Imatinib therapy was well tolerated in this patient population. After a median follow-up of 4 years, the 1-, 2-, and 3-year overall survival rates were 99%, 97%, and 97%, respectively. The 1-, 2-, and 3-year recurrence-free survival rates were 94%, 73%, and 61%, respectively.[43,44]
A Chinese group also evaluated adjuvant imatinib in a phase II study with similar results.[45] In this trial, 51 patients were included in the intention-to-treat analysis and 43 patients (75.4%) finished at least 12 months of imatinib treatment. Tumor relapses or metastases were identified in two patients (3.92%) at 350 and 680 days postoperation. The median disease-free survival was 385 days. No serious adverse events were reported. The score in quality of life showed no statistically significant difference between the baseline and the follow-up visits.
Randomized trials have also been conducted in this setting. The American College of Surgeons Oncology Group (ACOSOG) evaluated the benefit of adjuvant therapy in patients following complete resection of intermediate- or high-risk GIST.[46] Patients with tumors measuring 3 cm or greater were randomly assigned to 1 year of adjuvant imatinib at 400 mg daily or placebo. The only stratification criterion was tumor size (< 6 cm, 6–10 cm, > 10 cm). A planned interim analysis of 644 patients from 230 centers followed for a median of 14 months showed that patients who were randomized to treatment had significantly fewer recurrences (3% vs 17%). As expected, patients with a larger tumor at diagnosis achieved the best risk reduction with therapy in the subgroup analysis. A total of 38 recurrences occurred in the 158 patients with tumors larger than 10 cm-30 in the placebo arm and 8 in the imatinib arm (P < .001; hazard ratio [HR] = 0.19; CI = 0.09–0.41).
In the subgroup with intermediate-size tumors (6–10 cm), 217 patients were treated and 30 recurrences occurred, 21 in the placebo arm (P = .01; HR = 0.37; CI = 0.17–0.81). In the subgroup of those with tumors less than 6 cm in diameter only (n = 263), 15 recurrences were observed-4 in the imatinib recipients and 11 in the placebo recipients, with no statistically significant difference between these groups.
At the time the data were released, no survival difference was noted between patients treated with imatinib vs placebo. The toxicity profile was similar to that observed in other imatinib trials with the exception of a virtual absence of tumor bleeding.[46] Additional trials will be necessary to address the value of longer durations of imatinib following complete surgical resection, as there were many late recurrences after imatinib was stopped. The European Organisation for Research and Treatment of Cancer (EORTC) is leading a phase III trial that randomizes patients to 2 years of adjuvant imatinib (400 mg) or placebo. Another European study by the Scandinavian Sarcoma Group (SSGXVIII) is evaluating the use of adjuvant imatinib for 1 or 3 years in 240 patients with high-risk GIST after resection.
Neoadjuvant Therapy
In contrast to standard adjuvant therapy, neoadjuvant therapy is given before the main (usually surgical) treatment. It is used not only to eliminate circulating tumor cells but also to reduce the size of the tumor, potentially facilitating surgery, and perhaps increasing the chance of organ preservation. Since imatinib results in tumor shrinkage in at least 50% of treated patients,[23,47] its use in the neoadjuvant setting is a logical next step in the development of the drug.
TABLE 3
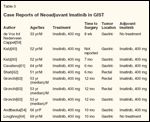
Case Reports of Neoadjuvant Imatinib in GIST
GISTs may present as unresectable disease or as resectable tumors requiring extensive organ disruption. Additionally, recurrence of locally advanced disease remains the norm. Thus, trying to achieve tumor downsizing with imatinib, followed by resection, followed (perhaps) by more imatinib could be an attractive approach. Since 2003, several case reports related to the use of neoadjuvant treatment in GIST have been published (Table 3), and one phase II Intergroup trial has been completed. The usual therapeutic schema involves a short course of imatinib, commonly 3 to 12 months, with frequent imaging studies and reevaluation of the best time for surgery. The decision of when to operate-at first respectability vs after maximum response-remains controversial, particularly since progression can occur rapidly even after a substantial response.
Despite careful patient management, the risk of disease progression is always present, and this possibility should be discussed before the start of treatment, particularly with patients who have borderline-resectable GISTs. In case of progression, a clinical dilemma is established. If radical salvage surgery is possible, it remains a reasonable therapeutic option (as opposed to a salvage systemic therapy, which would likely possess little chance of achieving substantial tumor shrinkage). Unfortunately, the results of surgery are probably worse for more extensive and refractory disease.
Retrospective Data
Retrospective published data demonstrate that resection of metastatic progressive disease appears to benefit only patients with focal progression, and it has little to offer to those who experience generalized disease progression while receiving imatinib.[48-55] For example, in 69 consecutive patients who underwent surgery for advanced GISTs at Dana-Farber Cancer Institute, 12-month progression-free survival rates were 80%, 33%, and 0%, respectively, for patients who presented before the procedure with stable disease, limited progression, and generalized progression (P < .0001). Overall survival at the same time was also strongly influenced by the presurgical response status, at 95%, 86%, and 0% for patients whose presented with stable disease, limited progression, and generalized progression (P < .0001).[52]
A Memorial Sloan-Kettering series of 13 patients with focal resistance showed similar conclusions: disease progression occurred at a median of 12 months after surgery, and the 2-year overall survival was 36%. In contrast, 7 patients with multifocal resistance showed disease progression at a median of 3 months postoperatively and had a 1-year overall survival rate of 36%.[50] Even if complete, resection does not eliminate the need for continued treatment with imatinib in patients with metastatic disease. Progression-free survival is significantly shorter in patients who discontinue imatinib, as compared to those who continue the drug after resection. In general, treatment of resistant nonsurgical GIST can be approached in different ways. At least two conventional therapeutic strategies can be adapted to this situation: The first alternative is to try to circumvent imatinib resistance by increasing the dose.[27] The second choice is to change the drug, and currently, sunitinib (Sutent) may be the best option in this setting.[56] Despite recent advances with the use of molecular targeted agents, surgical resection remains the only curative therapy for patients with GIST. Although 95% of salvage surgeries for GIST fail, the long-term control obtained with imatinib in a substantial fraction of patients with metastatic disease makes secondary surgery coupled with indefinitely administered imatinib attractive. No prospective trials have tested this approach, but it seems to be safe and may improve patient prognosis.
The role of surgery as part of the treatment plan for metastatic or unresectable GIST in the imatinib era has been explored in a few retrospective series. The group at the Institut Gustave Roussy reviewed results from 180 patients with metastatic or unresectable GIST treated with imatinib, 400 to 800 mg/d, finding that surgical treatment was eventually possible in 22 patients, 5 of whom had nonmetastatic locally advanced disease.[48] The 2-year overall survival rate after surgery was 62%. The median progression-free survival calculated from the initiation of imatinib therapy was 18.7 months for all patients who underwent surgery, and 23.4 months for the 17 patients who had planned surgery. Such data suggest that tumors that become amenable to surgery with the use of imatinib therapy could benefit from secondary surgery.
In 2003, a group at M.D. Anderson Cancer Center published a retrospective study of 126 patients with unresectable c-KIT–positive GIST treated with imatinib prior to surgical resection. They reported that 17 patients had subsequent surgical resections after a median of 10 months of neoadjuvant treatment. Of these patients, 2 had complete pathologic responses, 11 had partial pathologic responses, and 16 underwent complete surgical resection of disease.[57]
RTOG 0132
REFERENCE GUIDE
Therapeutic Agents
Mentioned in This Article
Imatinib (Gleevec)
Sunitinib (Sutent)
Brand names are listed in parentheses only if a drug is not available generically and is marketed as no more than two trademarked or registered products. More familiar alternative generic designations may also be included parenthetically.
In order to strengthen the preliminary data suggesting the benefits of neoadjuvant treatment with imatinib, the Radiation Therapy Oncology Group (RTOG) conducted a phase II trial (RTOG 0132).[58] To be included, patients needed to have a biopsy-proven diagnosis of malignant KIT-positive GIST-either potentially resectable primary disease (≥ 5 cm) or potentially resectable locally recurrent or metastatic disease (≥ 2 cm). Between February and June 2006, 63 patients from 18 institutions were enrolled and treated with preoperative imatinib (600 mg/d) for 8 to 12 weeks, followed by surgical resection and 2 additional years of postoperative imatinib therapy.
Among the 52 patients analyzed, 30 presented with locally advanced disease and 22 presented with recurrent or metastatic disease. The stomach was the primary disease site in 48% of patients; disease in the liver, small bowel, and pelvis accounted for 12%, 10%, and 10% of the cases. The toxicity profile was quite similar to that verified in other trials, with no grade 5 toxicities and 12% grade 4. A surgical procedure was performed in 45 of 52 patients, and only 1 patient died because of an infectious complication.
Among patients who initially presented with locally advanced disease, response to preoperative imatinib (by RECIST criteria) was observed in 2 patients (7%), 25 (83%) achieved stable disease, and none showed disease progression during treatment. Among patients who initially presented with recurrent or metastatic disease, 1 (5%) achieved a partial response and 20 (91%) had stable disease, with only one patient in this group (and the entire trial) showing disease progression during the course of treatment. Within 2 years of follow-up, progression-free and overall survival rates for patients who presented with locally advanced disease were 82% and 93%, respectively. For those with recurrent or metastatic disease, progression-free and overall survival rates were 73% and 91%.
This trial showed that preoperative treatment with imatinib is safe, with a minimal incidence of drug-related toxicity and surgical morbidity. Only one patient had disease progression on treatment, and the majority underwent surgical resection. Progression-free and overall survival are favorable for this group of high-risk patients receiving GIST, especially those with recurrent or metastatic disease. Despite these interesting results, no strong data support the use of neoadjuvant imatinib. This strategy is therefore not recommended outside of a clinical trial. The only reasonable exception would be the use of imatinib by an experienced multidisciplinary team when an objective response could result in organ preservation.
Conclusions
The use of TK inhibitors has resulted in a remarkable improvement in the management of GIST, and the impact of the use of imatinib after surgery seems to be positive. However, it is virtually impossible to draw any firm conclusions about the efficacy of this strategy yet, and well-designed, prospective trials are absolutely necessary. Surgery for residual disease should still be considered an investigational option, despite the growing popularity of this strategy. After changing the paradigm of treatment for metastatic GIST, imatinib mesylate is being increasingly viewed as an option in the adjuvant setting, and possibly in the neoadjuvant treatment of GIST. Ongoing and future trials will need to be conducted and completed before these strategies become the new standard of care for this tumor.
Financial Disclosure:The authors have no significant financial interest or other relationship with the manufacturers of any products or providers of any service mentioned in this article.
References:
1. Fletcher CD, Berman JJ, Corless C, et al: Diagnosis of gastrointestinal stromal tumors: A consensus approach. Int J Surg Pathol 10:81-89, 2002.
2. Mazur MT, Clark HB: Gastric stromal tumors. Reappraisal of histogenesis. Am J Surg Pathol 7:507-519, 1983.
3. Nishida T, Hirota S, Taniguchi M, et al: Familial gastrointestinal stromal tumours with germline mutation of the KIT gene. Nat Genet 19:323-324, 1998.
4. Hirota S, Isozaki K, Moriyama Y, et al: Gain-of-function mutations of c-kit in human gastrointestinal stromal tumors. Science 279:577-580, 1998.
5. Heinrich MC, Corless CL, Demetri GD, et al: Kinase mutations and imatinib response in patients with metastatic gastrointestinal stromal tumor. J Clin Oncol 21:4342-4349, 2003.
6. van Oosterom AT, Verweij J: New drugs for the treatment of sarcomas. Hematol Oncol Clin North Am 9:909-925, 1995.
7. Joensuu H: Gastrointestinal stromal tumor (GIST). Ann Oncol 17(suppl 10):x280-286, 2006.
8. Tryggvason G, Gislason HG, Magnusson MK, et al: Gastrointestinal stromal tumors in Iceland, 1990-2003: The Icelandic GIST study, a population-based incidence and pathologic risk stratification study. Int J Cancer 117:289-293, 2005.
9. Nilsson B, Bumming P, Meis-Kindblom JM, et al: Gastrointestinal stromal tumors: the incidence, prevalence, clinical course, and prognostication in the preimatinib mesylate era-a population-based study in western Sweden. Cancer 103:821-829, 2005.
10. Kawanowa K, Sakuma Y, Sakurai S, et al: High incidence of microscopic gastrointestinal stromal tumors in the stomach. Hum Pathol 37:1527-1535, 2006.
11. Tran T, Davila JA, El-Serag HB: The epidemiology of malignant gastrointestinal stromal tumors: An analysis of 1,458 cases from 1992 to 2000. Am J Gastroenterol 100:162-168, 2005.
12. DeMatteo RP, Gold JS, Saran L, et al: Tumor mitotic rate, size, and location independently predict recurrence after resection of primary gastrointestinal stromal tumor (GIST). Cancer 112:608-615, 2008.
13. Miettinen M, Sobin LH, Lasota J: Gastrointestinal stromal tumors of the stomach: A clinicopathologic, immunohistochemical, and molecular genetic study of 1765 cases with long-term follow-up. Am J Surg Pathol 29:52-68, 2005.
14. Miettinen M, Makhlouf H, Sobin LH, et al: Gastrointestinal stromal tumors of the jejunum and ileum: A clinicopathologic, immunohistochemical, and molecular genetic study of 906 cases before imatinib with long-term follow-up. Am J Surg Pathol 30:477-489, 2006.
15. Miettinen M, Lasota J: Gastrointestinal stromal tumors: Pathology and prognosis at different sites. Semin Diagn Pathol 23:70-83, 2006.
16. Emory TS, Sobin LH, Lukes L, et al: Prognosis of gastrointestinal smooth-muscle (stromal) tumors: Dependence on anatomic site. Am J Surg Pathol 23:82-87, 1999.
17. Huang HY, Li CF, Huang WW, et al: A modification of NIH consensus criteria to better distinguish the highly lethal subset of primary localized gastrointestinal stromal tumors: A subdivision of the original high-risk group on the basis of outcome. Surgery 141:748-756, 2007.
18. Fletcher CD, Berman JJ, Corless C, et al: Diagnosis of gastrointestinal stromal tumors: A consensus approach. Hum Pathol 33:459-465, 2002.
19. Kantarjian H, Sawyers C, Hochhaus A, et al: Hematologic and cytogenetic responses to imatinib mesylate in chronic myelogenous leukemia. N Engl J Med 346:645-652, 2002.
20. Druker BJ, Guilhot F, O’Brien SG, et al: Five-year follow-up of patients receiving imatinib for chronic myeloid leukemia. N Engl J Med 355:2408-2417, 2006.
21. Tuveson DA, Willis NA, Jacks T, et al: STI571 inactivation of the gastrointestinal stromal tumor c-KIT oncoprotein: Biological and clinical implications. Oncogene 20:5054-5058, 2001.
22. Joensuu H, Roberts PJ, Sarlomo-Rikala M, et al: Effect of the tyrosine kinase inhibitor STI571 in a patient with a metastatic gastrointestinal stromal tumor. N Engl J Med 344:1052-1056, 2001.
23. van Oosterom AT, Judson I, Verweij J, et al: Safety and efficacy of imatinib (STI571) in metastatic gastrointestinal stromal tumours: A phase I study. Lancet 358:1421-1423, 2001.
24. Demetri GD, von Mehren M, Blanke CD, et al: Efficacy and safety of imatinib mesylate in advanced gastrointestinal stromal tumors. N Engl J Med 347:472-480, 2002.
25. Blanke CD, Demetri GD, von Mehren M, et al: Long-term results from a randomized phase II trial of standard- versus higher-dose imatinib mesylate for patients with unresectable or metastatic gastrointestinal stromal tumors expressing KIT. J Clin Oncol 26:620-625, 2008.
26. Blay JY, Le Cesne A, Ray-Coquard I, et al: Prospective multicentric randomized phase III study of imatinib in patients with advanced gastrointestinal stromal tumors comparing interruption versus continuation of treatment beyond 1 year: The French Sarcoma Group. J Clin Oncol 25:1107-1113, 2007.
27. Blanke CD, Rankin C, Demetri GD, et al: Phase III randomized, intergroup trial assessing imatinib mesylate at two dose levels in patients with unresectable or metastatic gastrointestinal stromal tumors expressing the kit receptor tyrosine kinase: S0033. J Clin Oncol 26:626-632, 2008.
28. Zalcberg JR, Verweij J, Casali PG, et al: Outcome of patients with advanced gastro-intestinal stromal tumours crossing over to a daily imatinib dose of 800 mg after progression on 400 mg. Eur J Cancer 41:1751-1757, 2005.
29. Van Glabbeke MM, Owzar K, Rankin C, et al: Comparison of two doses of imatinib for the treatment of unresectable or metastatic gastrointestinal stromal tumors (GIST): A meta-analyis based on 1,640 patients (pts) (abstract 10004). J Clin Oncol 25(18S):546s, 2007.
30. Heinrich MC, Corless CL, Demetri GD, et al: Kinase mutations and imatinib response in patients with metastatic gastrointestinal stromal tumor. J Clin Oncol 21:4342-4349, 2003.
31. Heinrich MC, Corless CL, Blanke CD, et al: Molecular correlates of imatinib resistance in gastrointestinal stromal tumors. J Clin Oncol 24:4764-4774, 2006.
32. Verweij J, Casali PG, Zalcberg J, et al: Progression-free survival in gastrointestinal stromal tumours with high-dose imatinib: Randomised trial. Lancet 364:1127-1134, 2004.
33. Debiec-Rychter M, Sciot R, Le Cesne A, et al: KIT mutations and dose selection for imatinib in patients with advanced gastrointestinal stromal tumours. Eur J Cancer 42:1093-1103, 2006.
34. Patel S, Zalcberg JR: Optimizing the dose of imatinib for treatment of gastrointestinal stromal tumours: Lessons from the phase 3 trials. Eur J Cancer 44:501-509, 2008.
35. Corless CL, Schroeder A, Griffith D, et al: PDGFRA mutations in gastrointestinal stromal tumors: Frequency, spectrum and in vitro sensitivity to imatinib. J Clin Oncol 23:5357-5364, 2005.
36. Husband JE, Schwartz LH, Spencer J, et al: Evaluation of the response to treatment of solid tumours-a consensus statement of the International Cancer Imaging Society. Br J Cancer 90:2256-2260, 2004.
37. Antoch G, Kanja J, Bauer S, et al: Comparison of PET, CT, and dual-modality PET/CT imaging for monitoring of imatinib (STI571) therapy in patients with gastrointestinal stromal tumors. J Nucl Med 45:357-365, 2004.
38. Stroobants S, Goeminne J, Seegers M, et al: 18FDG-Positron emission tomography for the early prediction of response in advanced soft tissue sarcoma treated with imatinib mesylate (Glivec). Eur J Cancer 39:2012-2020, 2003.
39. Choi H, Charnsangavej C, Faria SC, et al: Correlation of computed tomography and positron emission tomography in patients with metastatic gastrointestinal stromal tumor treated at a single institution with imatinib mesylate: Proposal of new computed tomography response criteria. J Clin Oncol 25:1753-1759, 2007.
40. Benjamin RS, Choi H, Macapinlac HA, et al: We should desist using RECIST, at least in GIST. J Clin Oncol 25:1760-1764, 2007.
41. Buemming P, Meis-Kindblom JM, Kindblom LG, et al: Is there an indication for adjuvant treatment with imatinib mesylate in patients with aggressive gastrointestinal stromal tumors (GISTs) (abstract 3289)? Proc Am Soc Clin Oncol 22:818, 2003.
42. Nilsson BE, Bumming P, Meis-Kindblom JM, et al: Treatment of gastrointestinal stromal tumors GISTs) with imatinib in neoadjuvant, adjuvant and palliative settings, a centre-based study of 17 patients (abstract 3337). Proc Am Soc Clin Oncol 22:830, 2003.
43. Dematteo RP, Antonescu CR, Chadaram V, et al: Adjuvant imatinib mesylate in patients with primary high risk gastrointestinal stromal tumor (GIST) following complete resection: Safety results from the U.S. Intergroup Phase II trial ACOSOG Z9000 (abstract 9009). J Clin Oncol 23:818s, 2005.
44. DeMatteo RP, Owzar K, Antonescu CR, et al: Efficacy of adjuvant imatinib mesylate following complete resection of localized, primary gastrointestinal stromal tumor (GIST) at high risk of recurrence: The U.S. Intergroup phase II trial ACOSOG Z9000 (abstract 8). Presented at the 2008 Gastrointestinal Cancers Symposium; Orlando, Fla; Jan 25-27, 2008.
45. Zhan WH, for the China Gastrointestinal Cooperative Group: Efficacy and safety of adjuvant post-surgical therapy with imatinib in patients with high risk of relapsing GIST (abstract 10045). J Clin Oncol 25:556s, 2007.
46. DeMatteo R, Owzar K, Maki R, et al: Adjuvant imatinib mesylate increases recurrence free survival (RFS) in patients with completely resected localized primary gastrointestinal stromal tumor (GIST): North American Intergroup phase III trial ACOSOG Z9001 (abstract 10079). Presented at the Annual Meeting of the American Society of Clinical Oncology, Chicago, June 1-5, 2007. Available at www.asco.org. Accessed December 4, 2008.
47. Gold JS, Dematteo RP: Combined surgical and molecular therapy: The gastrointestinal stromal tumor model. Ann Surg 244:176-184, 2006.
48. Hasegawa J, Kanda T, Hirota S, et al: Surgical interventions for focal progression of advanced gastrointestinal stromal tumors during imatinib therapy. Int J Clin Oncol 12:212-217, 2007.
49. Bonvalot S, Eldweny H, Pechoux CL, et al: Impact of surgery on advanced gastrointestinal stromal tumors (GIST) in the imatinib era. Ann Surg Oncol 13:1596-1603, 2006.
50. DeMatteo RP, Maki RG, Singer S, et al: Results of tyrosine kinase inhibitor therapy followed by surgical resection for metastatic gastrointestinal stromal tumor. Ann Surg 245:347-352, 2007.
51. Rutkowski P, Nowecki Z, Nyckowski P, et al: Surgical treatment of patients with initially inoperable and/or metastatic gastrointestinal stromal tumors (GIST) during therapy with imatinib mesylate. J Surg Oncol 93:304-311, 2006.
52. Raut CP, Posner M, Desai J, et al: Surgical management of advanced gastrointestinal stromal tumors after treatment with targeted systemic therapy using kinase inhibitors. J Clin Oncol 24:2325-2331, 2006.
53. Al-Batran SE, Hartmann JT, Heidel F, et al: Focal progression in patients with gastrointestinal stromal tumors after initial response to imatinib mesylate: A three-center-based study of 38 patients. Gastric Cancer 10:145-152, 2007.
54. Andtbacka RH, Ng CS, Scaife CL, et al: Surgical resection of gastrointestinal stromal tumors after treatment with imatinib. Ann Surg Oncol 14:14-24, 2007.
55. Pantaleo MA, Di Battista M, Catena F, et al: Surgical debulking of gastrointestinal stromal tumors: Is it a reasonable option after second-line treatment with sunitinib? J Cancer Res Clin Oncol 134:625-630, 2008.
56. Joensuu H: Sunitinib for imatinib-resistant GIST. Lancet 368:1303-1304, 2006.
57. Scaife CL, Hunt KK, Patel SR, et al: Is there a role for surgery in patients with “unresectable” cKIT+ gastrointestinal stromal tumors treated with imatinib mesylate? Am J Surg 186:665-669, 2003.
58. Eisenberg BL, Harris J, Blanke C, et al: Phase II trial of neoadjuvant/adjuvant imatinib mesylate (IM) for advanced primary and recurrent operable GI stromal tumor (GIST)-early results of RTOG 0132 (abstract 80). Presented at the Society of Surgical Oncology’s 61st Annual Cancer Symposium; Chicago; March 13-16, 2008.
59. de Vos tot Nederveen Cappel RJ, van Hillegersberg R, Rodenhuis S, et al: Downstaging of an advanced gastrointestinal stromal tumor by neoadjuvant imatinib. Dig Surg 21:77-79, 2004.
60. Katz D, Segal A, Alberton Y, et al: Neoadjuvant imatinib for unresectable gastrointestinal stromal tumor. Anticancer Drugs 15:599-602, 2004.
61. Cavaliere D, Vagliasindi A, Mura G, et al: Downstaging of a gastric GIST by neoadjuvant imatinib and endoscopic assisted laparoscopic resection. Eur J Surg Oncol 33:1044-1046, 2007.
62. Shah JN, Sun W, Seethala RR, et al: Neoadjuvant therapy with imatinib mesylate for locally advanced GI stromal tumor. Gastrointest Endosc 61:625-627, 2005.
63. Gronchi A, Fiore M, Miselli F, et al: Surgery of residual disease following molecular-targeted therapy with imatinib mesylate in advanced/metastatic GIST. Ann Surg 245:341-346, 2007.
64. Loughrey MB, Mitchell C, Mann GB, et al: Gastrointestinal stromal tumour treated with neoadjuvant imatinib. J Clin Pathol 58:779-781, 2005.