PET Scans Alter Management of Colorectal Cancer Recurrence
EAST MELBOURNE, Australia-A new prospective study has confirmed the usefulness of 18F-FDG PET in treatment planning for patients with confirmed or suspected colorectal cancer recurrence. In this study, 60% of planned surgeries were found to be unnecessary as the result of PET.
EAST MELBOURNE, AustraliaA new prospective study has confirmed the usefulness of 18F-FDG PET in treatment planning for patients with confirmed or suspected colorectal cancer recurrence. In this study, 60% of planned surgeries were found to be unnecessary as the result of PET.
The study, led by Victor Kalff, MB, BS, and his colleagues in the Department of Diagnostic Imaging, Peter MacCallum Cancer Institute, East Melbourne, involved 102 patients referred for PET scan to evaluate suspected or confirmed regional recurrences of colorectal cancer. For 96 of these patients, their physicians had indicated a proposed treatment plan based on their current (pre-PET) status, and for 6 patients, their physicians preferred to wait for the PET results before creating a treatment plan. All were potential candidates for aggressive therapy if localized disease was confirmed.
The study was designed "to replicate as closely as possible the likely niche of PET in a clinical setting as an investigation performed after structural imaging," the authors said. Thus, patients with CT-confirmed disseminated metastases were excluded because PET was unlikely to alter their management even if additional disease sites were detected.
Patients were subdivided into five diagnostic subgroups: limited (solitary or adjacent) metastases amenable to aggressive local therapy; rising CEA levels with either normal or equivocal CT findings; increasing local symptoms; known recurrences but extent characterization needed for treatment planning; and new mass or residual mass suggestive of recurrence but unconfirmed by biopsy.
The following definitions were used for patient management: Active treatment (any combination of surgery, radiotherapy, or chemotherapy given for proven recurrence); supportive treatment (recurrence was proven but no active treatment was given); and observation (no recurrence found and routine surveillance planned).
Study Results
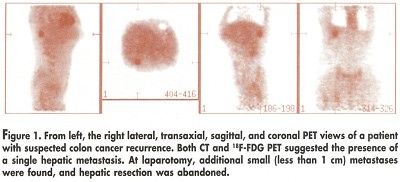
PET was shown to influence the management of 60 of the 102 patients (59%). In all 6 of the patients without a treatment plan, PET correctly guided management. Of the remaining 96 patients, the information provided by PET directly changed the planned management of 54 patients (56%) (J Nucl Med 43:492-499, 2002).
Disease status as defined by PET was confirmed in 52 of the 57 patients for whom management was influenced by PET and clinical follow-up was available: there were 7 true-negative and 45 true-positive PET results.
Only one patient had a false-positive PET result, relating to a pelvic abscess, but the patient was appropriately managed by surgery. In another 5 patients, the PET finding was true-positive but underestimated the extent of disease. Thus, the authors said, 49 (98%) of 50 evaluable patients with positive PET findings had confirmation of relapse.
There were four false-negative PET findings. In two cases, the error was recognized because of a biopsy-confirmed small hepatic metastasis on CT. In both cases, exclusion of extrahepatic disease by PET allowed hepatic resection to proceed. The other two patients had small peritoneal deposits that were missed by both PET and CT; in both cases, the lesions were directly visualized by invasive procedures.
In two patients, PET correctly identified relapse (an isolated liver metastasis) but underestimated the extent of disease. "Nevertheless," the authors said, "inappropriate hepatic resection was avoided in both patients by subsequent evaluation." The authors warned that, with PET, "underestimation of disease extent is not uncommon, and negative results need ongoing surveillance as a minimum."
Changes By Diagnostic Subgroup
"Substantial changes in management were observed for every diagnostic subgroup," the authors said. The percentage of patients for whom treatment changed ranged from 42% for those with a new mass up to 71% for those with increasing symptoms. In the largest diagnostic subgrouppatients with limited metastasestreatment was changed in 20 of 34 patients (59%). Among the 54 patients for whom the pre-PET treatment plan was changed by PET, the most common type of change was to vary the active treatment, which occurred in 26 patients.
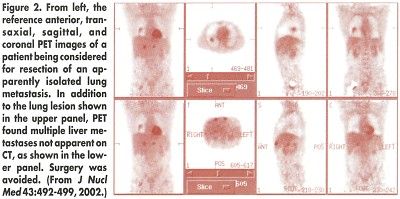
In 5 patients, the change was from active treatment to observation; in 11, from active treatment to supportive care; and in 12, from observation to active treatment. PET prevented surgery in 26 (60%) of 43 patients for whom it had been planned.