Prognosis Good for Local Recurrence After Lumpectomy
SAN ANTONIO-Patients who develop a local recurrence after conservative surgery and radiation therapy for early-stage breast cancer generally have a good long-term prognosis, particularly if treated with mastectomy, lead researcher Sharon Galper, MD, told ONI. In this study, 59% of patients with a local recurrence were alive at 10 years, said Dr. Galper, assistant professor of radiation oncology, Brigham and Women’s Hospital, Dana-Farber Cancer Institute, and Harvard Medical School.
SAN ANTONIOPatients who develop a local recurrence after conservative surgery and radiation therapy for early-stage breast cancer generally have a good long-term prognosis, particularly if treated with mastectomy, lead researcher Sharon Galper, MD, told ONI. In this study, 59% of patients with a local recurrence were alive at 10 years, said Dr. Galper, assistant professor of radiation oncology, Brigham and Women’s Hospital, Dana-Farber Cancer Institute, and Harvard Medical School.
Jay R. Harris, MD, chief of radiation oncology at Dana-Farber and professor of radiation oncology at Harvard, presented the study results at the 24th Annual San Antonio Breast Cancer Symposium (abstract 14).
From 1970 to 1987, 2,102 patients with clinical stage I/II breast cancer were treated with complete excision and radiation therapy. Among these patients, there were 318 local recurrences, defined as any recurrence within the ipsilateral breast, with or without simultaneous regional nodal or distant metastasis.
Patients were considered at risk for local recurrence until the occurrence of distant metastases, contralateral breast cancer, or second nonbreast malignancy. The final study population consisted of 288 patients.
The median time to local recurrence (the radiation therapy-local recurrence interval) was 64.5 months (range, 1 to 220); median follow-up after local recurrence was 95 months (range, 12 to 271); and median age at initial diagnosis was 45 years (range, 25 to 88).
Local recurrence was noninvasive for 38 patients (13%), invasive for 225 (78%), and unknown for 25 (9%). Local therapy after local recurrence consisted of mastectomy in 235 patients (82%), local excision with or without radiation therapy in 22 (8%), and none in 31 (10%). Systemic therapy was given to 46% of patients at the time of local recurrence.
Dr. Harris reported that of the 288 local recurrences, 268 occurred in isolation, 5 with simultaneous opposite breast failure, and 15 with simultaneous ipsilateral regional-nodal failure.
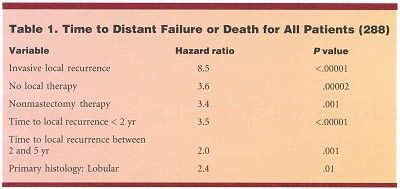
Variables significantly associated with time to distant failure or death for all patients in a proportional hazards model are shown in Table 1.
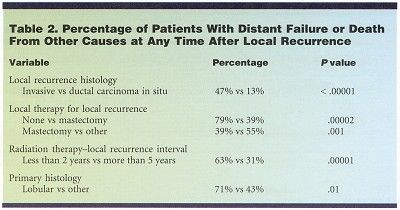
The actuarial risk of distant failure or death from other causes 10 years after local recurrence was 48%, Dr. Harris said. Variables significantly associated with time to distant failure or death from other causes in the final proportional hazards model and the percentages with distant failure or death from other causes at any time are shown in Table 2.
Possible limitations of the study, Dr. Harris said, included the fact that it was a retrospective series, potential misclassifications, lack of information regarding size of local recurrences, and possible selection bias in salvage of local recurrence. In addition, he said, the older methods of detection and treatment used in the study may limit the applicability of the data to current patients.
The Harvard group concluded that patients with local recurrence after conservative surgery and radiation therapy can have prolonged disease-free survival. Patients with a noninvasive local recurrence, longer interval to local recurrence, nonlobular histology, and treatment with mastectomy had a longer time to distant failure or death from other causes than other patients.