Primary Focal Therapy for Localized Prostate Cancer: A Review of the Literature
Focal therapy for prostate cancer could balance undertreatment and overtreatment of localized prostate cancer for highly selected patients. Long-term oncologic outcomes are not yet available for any modality. Patients should be informed regarding currently available outcomes, the necessity of adherence to a stringent follow-up protocol, and the possible need for additional targeted therapy or future radical treatment in case of recurrence.
Hayes is a resident physician in the Department of Urology at Oregon Health & Science University in Portland, OR.

Lin-Brande is a resident physician in the Department of Urology at Oregon Health & Science University in Portland, OR.

Isharwal is an assistant professor in the Department of Urology at Oregon Health & Science University in Portland, OR.

Introduction
Prostate cancer (PCa) is the most common noncutaneous cancer in men in the United States. Approximately 191,930 men will be diagnosed and 33,330 men will die from PCa in 2020.1 With the introduction of widespread prostate-specific antigen (PSA) screening, most men are diagnosed at the localized PCa stages. Several well-established treatment options, such as radical prostatectomy, radiation therapy, and whole-gland cryotherapy, are available for localized PCa. Although these treatment modalities are highly effective in providing a cure at the localized stage, they are often associated with debilitating adverse effects (AEs) such as erectile dysfunction and urinary incontinence. As a result, patients often delay or defer treatment of their PCa altogether.
In the past decade, active surveillance (AS) has increased for low- and very low-risk PCa, which has reduced overtreatment and sequelae of definitive treatment. However, as noted in the PROTECT trial, approximately 50% of AS patients will ultimately require treatment due to disease progression.2 Additionally, some patients will progress to the nonlocalized disease stages during the surveillance period and miss the opportunity for a cancer cure. Risk-stratification methods to better select and monitor patients for AS is an area of active investigation. Yet, for many patients, both the increased oncologic risks associated with AS and the quality-of-life concerns related to whole-gland treatment are understandably unacceptable. As a result, the evolving literature around focal therapy has garnered much attention among patients and providers.
Focal treatment modalities treat the diseased area of the organ while preserving the normal surrounding tissue to preserve organ function and minimize AEs. Focal treatment of malignancies has been successfully implemented in breast, thyroid, lung, colon, and kidney cancers among others, with oncologic outcomes comparable with those of radical surgical resection. Recently, focal treatment modalities have been applied to PCa. Although PCa is largely a multifocal disease, a single focus of cancer, often called the index lesion, is thought to drive progression and to harbor the genetic precursor cells of advanced late-stage cancer.3 Pretreatment disease localization was previously a challenge in PCa, but significant strides have been made in this area with the advances in multiparametric MRI (mpMRI) for diagnosis and staging. mpMRI is highly sensitive for high-grade PCa and for detecting the index lesion at rates of 72% and 80%, respectively, on examining whole-mount pathology.4 With ultrasound fusion platforms, the disease area can be precisely localized and targeted with a transrectal or transperineal approach. Several devices that deliver ablative energies have become available to target the specific disease area for treatment. Standard-of-care options such as surgery and radiation are also being modified and subsequently investigated to evaluate the safety and efficacy of partial prostate treatment.
This article describes the available focal therapy options for primary treatment of localized PCa, along with their respective outcomes, drawbacks, and applicability.
Oncology (Williston Park). 2021;35(5):261-268.
DOI: 10.46883/ONC.2021.3505.0261
Methods
We reviewed PubMed using multiple permutations of relevant search terms including but not limited to prostate cancer, focal therapy, focal ablation, focal high-intensity focused ultrasound (HIFU)” cryoablation, focal laser ablation, irreversible electroporation, photodynamic therapy, brachytherapy, radiofrequency ablation, partial prostatectomy, and focal transurethral ultrasound ablation (TULSA). We focused on the studies describing the primary treatment of PCa. Studies of salvage focal therapies were excluded. A full-text review of all selected articles was performed.
Results
Rationale for the Use of Focal Therapy
In 2012, in response to increasing concerns over harms caused by PCa overtreatment, the US Preventative Services Task Force (USPSTF) discouraged the use of PSA screening to detect PCa. The USPSTF has since reversed its PSA screening position, due to longer follow-up of clinical trial patients that showed a decrease in number necessary to screen to prevent 1 death from PCa, and due to more frequent adoption of AS to avoid overtreatment of indolent disease. Now the USPSTF makes a grade C recommendation for PSA screening based on shared decision-making between physicians and patients. Although increased adoption of AS for low-risk disease has decreased overtreatment and related AEs, the decision of any patient and their physician to cease AS and pursue definitive whole-gland treatment remains challenging. Discontinuation of AS occurs both because of progression to aggressive disease and because of patient and physician anxiety about untreated cancer. A clear unmet need exists for a more nuanced balance of treatment options, falling between AS and radical therapies, to optimally treat visible cancer with minimal AEs.
Between 13% and 38% of radical prostatectomy specimens contain a single focus of cancer.5 The histopathology of index lesions predicts PCa’s natural history in the vast majority of patients.6 Advances in MRI technology, including improved protocols and the introduction of the 3 Tesla machine, allow better localization of PCa lesions. Whole-mount pathology of prostatectomy specimens has demonstrated concordance of the lesion with a visible lesion on MRI.4 Further, systematic biopsy combined with MRI-targeted biopsy allows optimal sampling of the prostate to determine the extent and multifocality of PCa. Image-guided localization enables investigators to target and treat these lesions with a multitude of ablative energies, radiation, and partial-gland surgery. These treatment modalities allow the preservation of anatomical structures sustaining continence and erectile function, thus minimizing AEs.
Focal Therapy Treatment Modalities
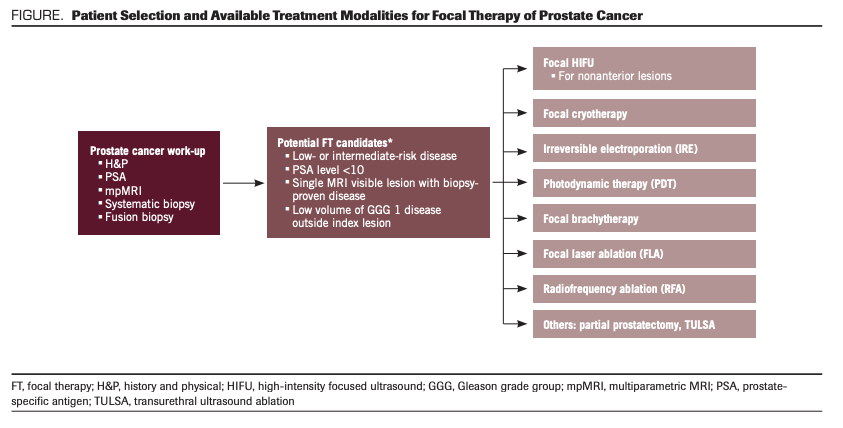
Several focal treatment modalities are available to selectively treat the disease area in the prostate. They differ in terms of energy source and their effects on the prostate tissue. Selection of the treatment modality for focal treatment of PCa depends on the availability of the focal treatment modality at the treatment center, training of the physician, size of the prostate, location of the index lesion, extent of disease outside the index lesion, calcifications in the prostate, and patient-specific factors. Widely used patient selection criteria, as well as common focal treatments, are summarized in the Figure.
FIGURE. Patient Selection and Available Treatment Modalities for Focal Therapy of Prostate Cancer
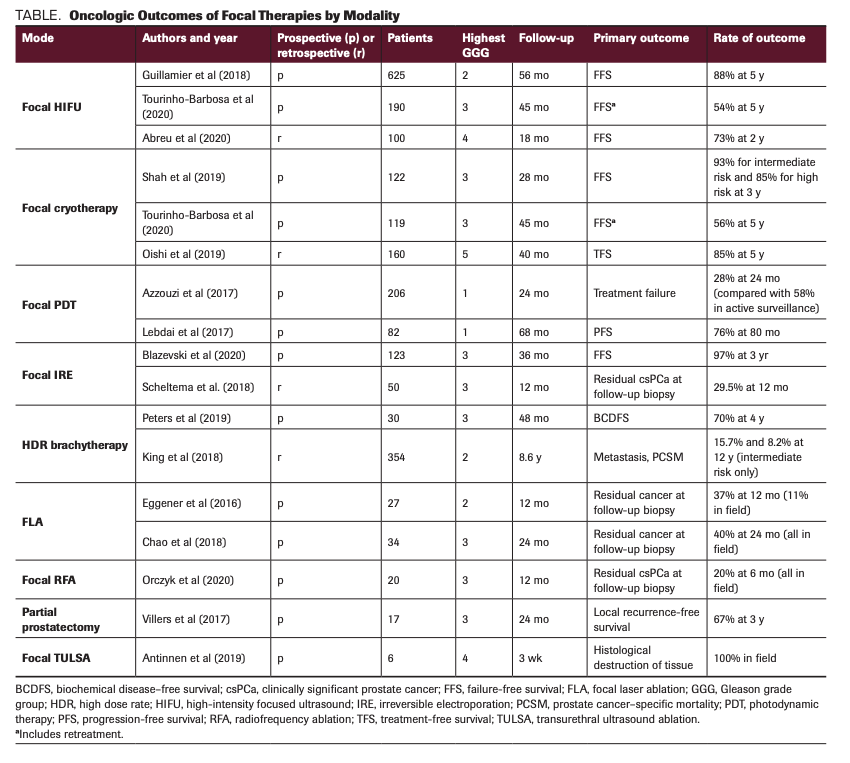
Here, we summarize available treatment modalities, proposed mechanisms, and findings from the pivotal studies. Important oncologic outcomes from the studies are noted in the Table.
TABLE. Oncologic Outcomes of Focal Therapies by Modality
Focal High-Intensity Focused Ultrasound
HIFU uses high-energy ultrasound to target and ablate a parabolic-shaped area of prostate tissue. The prostate is imaged via a transrectal ultrasound probe, and the PCa lesion is mapped out. Ultrasound energy then induces cell necrosis by thermal energy, heating the tissue up to 100°C.7
Several devices are commercially available and have been studied, including Ablatherm, Focal One, and Sonablate 500. HIFU has been studied in primary whole-gland treatment, salvage treatment, and primary focal therapy settings. National Comprehensive Cancer Network (NCCN) guidelines recommend salvage HIFU for radio-recurrent PCa. However, no guideline recommendations exist for the use of HIFU in the primary setting. The FDA approved HIFU for tissue ablation in 2015, but it was not approved for PCa treatment due to inadequate data for its efficacy in the primary setting.
A multicenter study reported 5-year outcomes for 625 men who received primary focal HIFU. Patients with localized Gleason 9 or less, cT3b or lower, and PSA ≤30 ng/mL were included in the study. The primary outcome was failure-free survival (FFS), a composite outcome of avoiding whole-gland therapy, systemic therapy, metastasis, and PCa–specific death. In the study, 83% of the cohort had Gleason 6 or 7 disease, and 75% had PSA <10 ng/mL. FFS was 88% at 5 years for all patients. In a prespecified subgroup analysis, FFS for low-, intermediate-, and high-risk patients was 96%, 88%, and 84%, respectively, and metastasis-free survival was 96%, 99%, and 97%, respectively. The most common complication was urinary tract infection at a rate of 10.4%. The most severe complication was rectourethral fistula formation in 2 patients (0.3%), 1 of whom required reconstruction. At 2 to 3 years of follow-up, 80% of patients reported no urinary leakage at all, and 98% were pad-free. Erectile function and retreatment rates were not reported.8
Recently, Abreu and colleagues evaluated the use of hemigland HIFU in the primary setting in 100 men with localized PCa. By NCCN risk stratification, 20% had low-risk, 50% had intermediate favorable, 17% had intermediate unfavorable, and 5% had high-risk disease. The 2-year survival rates specific for freedom from treatment failure, local recurrence of Gleason 7 or greater, repeat focal HIFU, and radical treatment were 73%, 76%, 90%, and 91%, respectively. Of the men who underwent posttreatment biopsy, 17% had in-field recurrence and 14% had out-of-field recurrence with Gleason grade group 2 and higher. No declines in potency, measured by the International Index of Erectile Function (IIEF), were noted after treatment. Posttreatment continence was also excellent.9 In another study by Nahar and colleagues, 52 patients were treated with primary focal HIFU, of whom 67% harbored Gleason score 7 or higher. In-field (17%) and out-of-field recurrences (13%) were noted. Approximately 10% of patients had grade 3 or higher complications. In all patients with available data, urinary and sexual function returned to baseline at 3 to 6 months and at 12 months, respectively.10
Based on the available short- to intermediate-term studies, HIFU is marked by good efficacy, low rates of in-field and out-of-field recurrences, and preservation of urinary and sexual function. Several limitations are noted for focal HIFU, however. The patient must be free of limiting rectal pathology that would preclude use of a transrectal probe for delivery. Large glands >40 g may be a contraindication for HIFU using some older devices, as the focal length may not be adequate.11 Anterior lesions treated with primary HIFU have been shown to require additional treatment at a higher rate than posterior lesions, as the penetration depth of the ultrasound energy is limited.12 Widespread calcifications may also be a limitation; they can cause acoustic shadowing, which does not allow passage of the therapeutic sound waves. Further efforts are under way to identify patients who will fail the focal HIFU treatment, so they may be offered a different focal modality or whole-gland treatment.
Focal Cryoablation
Cryoablation is rapid cooling performed by transperineal needle placement down to temperatures of –40 °C. It results in the formation of an ice ball and subsequent tumor lysis. Preclinical trials suggested that margins of at least 1 cm around the target tissue are needed to ensure cancer ablation.13
Most of the data for the focal prostate cryoablation studies come from the COLD (Cryo On-Line Data) registry. The largest prospective registry of focal cryoablation reported early outcomes of 122 men; largely, they had intermediate-risk disease, confirmed with mpMRI targeted biopsy or transperineal mapping, with a maximum cancer core length of 6 mm. These patients were explicitly selected due to unsuitability for HIFU (because of anterior disease, anterior-posterior height of greater than 3 cm, or widespread calcifications). Standard FFS was the primary outcome, at a rate of 90.5% at 3 years. Stratified by risk, FFS was better in intermediate-risk disease (93%) compared with high-risk disease (84%). A total of 6.5% required additional focal cryotherapy at last follow-up. In a subgroup analysis of 2 groups stratified by PSA, those with PSA <10 ng/mL had higher FFS (97%) compared with patients with PSA >10 ng/mL (84%).14
Complications were reported in 27.8% of men; urinary tract infection and temporary urinary retention were the most common. Serious complications included osteomyelitis in 1 patient who was managed conservatively, and no rectourethral fistulas were reported. At 3 years, 87% and 89% had returned to baseline International Prostate Symptom Scores (IPSS) and IIEF scores, respectively.15
Another prospective single-institution registry of 119 men who received primary focal cryotherapy reported slightly lower FFS, 73% and 56% at 3 and 5 years, respectively. Radical treatment–free survival was also reported, at rates of 83% and 70% at 3 and 5 years, respectively.16 Similar outcomes have been noted with hemigland ablation. In a retrospective study of 160 patients with largely intermediate-risk cancer, FFS without retreatment was 85% at 5 years. High baseline PSA was predictive of failure.17
Cryotherapy is not the first energy modality of choice for posterior or apical tumors, as surrounding tissue damage can occur, affecting the neurovascular bundles and subsequently erectile function.18 As such, patient selection is critical in the success of focal cryotherapy. Similarly, cryotherapy may also not be well suited for small glands, as the expanding ice ball may extend beyond the prostate.18 However, although these preferences for tumor location and prostate size are repeatedly seen in the literature, trials with well-defined selection criteria do not support or refute those preferences.
Photodynamic Therapy
Photodynamic therapy (PDT) uses oral or intravenous drugs that are inactive until they are photosensitized, at which time they form reactive oxygen species leading to tissue destruction. A laser fiber is targeted at the prostate, which is typically placed using transrectal ultrasound guidance. Several types of photosensitizing drugs are used and are usually categorized as either tissue-based or vascular-based, depending on where the drugs are activated. The drugs can take up to several days to reach maximum dose in the tissue, while vascular-based drugs activate within minutes after photosensitization.19
In a large phase 3 randomized controlled trial, patients with low-risk PCa were randomized to either AS or padeliporfin vascular-targeted PDT. The median follow-up was 24 months and 206 men were randomized to PDT. The primary outcome was time to progression, a composite outcome of having 4 or more positive cores, any Gleason pattern 4 or greater, at least 1 cancer core length greater than 5 mm, PSA >10 ng/mL on 3 consecutive measures, any T3 PCa, or metastasis. The study measured the median time for the PCa to progress from low-risk to moderate-risk or high-risk; this time was longer in the PDT group than the AS group, at 28.3 months vs 14.1 months (P <.0001). When compared with the AS group, more men in the PDT group had negative biopsies at 24 months (49% vs 14%; P <.0001) and fewer men in the PDT group underwent radical therapy of either radiation or surgery (6% vs 29%; P <.0001). Erectile and urinary function were similar between the 2 groups at 24 months. AEs in the PDT group were pain, urethral stricture, urge incontinence, and urinary retention.20
Other studies of relatively small cohorts have shown similar short-term outcomes. In one prospective trial, 82 men with low-risk PCa were treated with PDT. The primary end point was progression-free survival (PFS), defined as an intermediate-risk or high-risk group by D’Amico classification or radical therapy. Median PFS was 86 months, and only 24% of patients underwent radical treatment.21
Overall, PDT is effective in delaying the progression of low-risk cancer compared with AS. Potential drawbacks to PDT include the need to avoid direct sunlight following the procedure for 48 hours to reduce AEs and the potential of an allergic reaction to the photosensitized agent.
Irreversible Electroporation
Irreversible electroporation (IRE) uses microsecond electrical pulses to generate pores in the cell membrane. While reversible electroporation allows for temporary changes to the cell, IRE leads to cell destruction as the cells cannot maintain homeostasis. Compared with other ablative modalities, IRE appears to spare surrounding nerves and vessels from collateral damage.22 In theory, this property suggests that IRE is better suited for focal treatment of PCa compared with other ablative modalities. During IRE of the prostate tumor, patients are placed in the lithotomy position under general anesthesia with full muscle paralysis to reduce muscle spasms. Needle probes are placed transperineally, typically using a brachytherapy template.23
Valerio and colleagues studied the safety and feasibility of focal IRE. A total of 34 patients, primarily with low- and intermediate-risk PCa, underwent focal IRE. No grade 3 complications were noted. At 6 months follow-up, from a functional perspective, 100% of men were continent and 95% were potent after focal IRE. Approximately 20% had residual cancer, as evaluated by mpMRI.24 In a phase 1/2 study, van den Bos and colleagues evaluated the histopathology of the prostate tissues of men who underwent IRE, and all cells within the electrode zone were completely ablated. No skip lesions were noted, demonstrating the effectiveness of the IRE as an ablation modality.25
Blazevski and colleagues evaluated their experience with IRE in 123 men with PCa, a majority (91%) with intermediate-risk disease, at a median follow-up of 3 years. FFS, defined by whole-gland treatment, systemic disease, or death, was 96% at 3 years. In up to 9% of the patients, in-field recurrences were noted. Eighteen men required retreatment: 12 underwent repeat IRE and 6 had whole-gland treatment. Functional outcomes were excellent, with 98% of men remaining pad free and 76% having no change in erectile function.26
There are no randomized trial comparisons of IRE with radical prostatectomy in the literature. However, Scheltema and colleagues made a pair match comparing 50 men with cT1c-T2b, unifocal disease who underwent IRE with 50 men who underwent robot-assisted nerve-sparing radical prostatectomy. No significant differences emerged in the baseline oncologic and functional characteristics. At 12 months, urinary continence and sexual function were superior in the men who underwent IRE treatment compared with those who had robot-assisted laparoscopic radical prostatectomy (RARP), but higher local failure (29.5%) was noted in the men treated with IRE.27
IRE is a promising focal therapy treatment. However, further larger studies with appropriate control arms are needed to establish its role in PCa treatment, as well as to define potential selection criteria and drawbacks.
Focal Brachytherapy
Whole-gland brachytherapy and salvage brachytherapy have been used to treat localized PCa and have been recommended in the NCCN guidelines to treat low-risk disease. However, little evidence exists for primary MRI-guided brachytherapy for focal therapy of PCa. Although the field has anticipated the promise of focal high dose rate (HDR) brachytherapy for PCa, clinical trials have not, in many cases, delivered promising outcomes.28
King and colleagues reviewed their experience with focal MRI-guided brachytherapy in a large cohort of 354 men: 40%, 39%, and 21% of patients had very low-risk, low-risk, and intermediate-risk disease, respectively. At a median of 11 years follow-up, 22 men (6.2%) had developed metastatic disease. The 12-year metastasis rates for patients with very low-risk, low-risk, and intermediate-risk disease were 0.8%, 8.7%, and 15.7%, respectively.
More importantly, the 12-year PCa-specific mortality estimates were 1.6% in very low-risk, 1.4% in low-risk, and 8.2% in intermediate-risk disease, respectively. Due to the high rate of metastasis and PCa-specific mortality rates, the authors concluded that partial gland ablation with brachytherapy might not be appropriate for patients with intermediate-risk disease.29
Other prospective studies with shorter-term follow-up have shown concordant results. Biochemical recurrence-free survival after focal HDR brachytherapy was poor in one study with 4 years of follow-up, at a rate of 70% in 30 patients.30 No other relevant oncologic outcomes, such as FFS or salvage whole-gland treatment, were reported in this study.
Focal Laser Ablation
Focal laser ablation (FLA) is an MRI-guided technique that uses a low-powered laser fiber to deliver thermal energy transrectally to the soft-tissue target. The tissue ablation temperature exceeds 60°C. This technology was adapted from use in intracranial neoplasms.31
Only a few small studies have reported outcomes from use in the primary treatment of PCa. One phase 2 trial of 27 men, primarily with low-risk disease, received FLA for up to 2 MRI-visible lesions. No residual cancer was noted in 96% of men, utilizing MRI-targeted biopsy 3 months after treatment, but residual cancer was detected in 37% at a follow-up systematic biopsy at 12 months. The complication profile was favorable, with hematuria, perineal ecchymosis, and urinary retention as the most common AEs.32 No significant difference was seen in IPSS or Sexual Health Inventory for Men (SHIM) scores between baseline and at 12 months. In another study by Lepor and colleagues, 25 men with Gleason score <8, cT1c-T2a, and PSA <10 ng/mL were treated with FLA and monitored with MR thermometry. No decline in IPSS or SHIM score was noted at 3 months, with 96% of men noted to have a negative ablation-zone biopsy.33
In a larger prospective trial of 120 patients who underwent FLA for primarily low- or intermediate-risk disease, 15% harbored residual clinically significant disease upon follow-up MRI-targeted biopsy; 17% required retreatment of some sort. A change in technique significantly limited this study during the study period.34 Two-year oncologic outcomes were reported in another prospective study of primary FLA, and 18.8% harbored clinically significant PCa at follow-up biopsy.35
Prostate volume limitations and contraindications to FLA are not well defined in the literature.36
Focal Radiofrequency Ablation
Focal radiofrequency ablation (RFA) has been studied as a treatment for cancer in various organs, including the liver and kidney. It delivers thermal energy using medium-frequency alternating current by way of a transperineal probe.37
Only 1 prospective phase 2 study exists in the literature. It recently reported the short-term outcomes of 20 men who underwent bipolar RFA, 90% of whom had Gleason 7 disease. At a 6-month follow-up targeted biopsy, 80% of men were free of clinically significant PCa within the treated lesion. Utilizing the Expanded Prostate Cancer Index Composite questionnaire, 89% of patients who had no baseline urinary dysfunction were found to be free of incontinence at
12 months. Using responses to the IIEF, the investigators found that 91.7% of patients with no baseline erectile dysfunction reported the ability to achieve adequate erections with or without phosphodiesterase-5 inhibitors.38 No serious AEs were reported.
Due to the paucity of literature for focal RFA in this setting, additional research is needed to establish selection criteria and drawbacks.
Partial Prostatectomy
Partial prostatectomy is a subtotal surgical resection of a prostate tumor, and cancer control outcomes of this approach have been sparsely recorded in the literature. However, recently, the short-term results of a single-arm multicenter prospective trial of robotic partial prostatectomy for anterior tumors were reported.39 Seventeen patients, primarily with anterior preurethral tumors visible on MRI, were enrolled. All patients underwent robotic partial prostatectomy via a transperitoneal approach. Perioperative outcomes were excellent, with no grade 3 complications reported. Three-month continence and erectile function rates were 100% and 83%, respectively. Long-term oncologic outcomes were not reported. However, the local recurrence-free survival rate was 67% at 3 years, and 24% of men underwent a completion radical prostatectomy.
Although this is a novel approach for the treatment of anterior zone PCa, only a few men would be eligible to meet the inclusion criteria of preurethral tumors, and with a high local failure rate, some would require whole-gland therapy soon after.
Focal Transurethral Ultrasound Ablation
MRI-guided TULSA is a novel procedure in which prostate tissue is ablated in a continuous sweeping fashion by the directed ultrasound. The ablation zone is monitored with MR thermometry. It has been studied mainly as a whole-gland therapy for PCa.
Recently, the TULSA-PRO (designated for the technology’s manufacturer, Profound Medical) Ablation Clinical Trial protocol was developed, and the single-arm multicenter trial was completed for the whole-gland treatment of PCa. Patients with Gleason 6 and 7, cT1 to cT2b, and MRI visible tumors, with PSA <15 ng/mL, were enrolled in the study. Patients with prostate volume >90 cc, intraprostatic calcifications >1 mm, and prostate tumors within 3 mm of the prostate apex on MRI were excluded. The trial’s primary objectives were safety and efficacy, defined as PSA decline equal to or greater than 75%. The secondary oncologic objective was disease improvement at repeat biopsy, defined as no cancer or reduced cancer grade on 10-core biopsy at 12 months. Urinary function was evaluated with IPSS, and erectile dysfunction was evaluated with the IIEF score. A total of 115 men, 33% with low-risk disease and 67% with intermediate-risk disease, underwent whole-gland therapy. At 12 months, 8% of patients had grade 3 complications, with urinary tract infection and urethral stricture being the most common. A total of 96% of patients met the primary objective of PSA decline >75%. A total of 23% of patients developed moderate erectile dysfunction requiring medical management. No cancer was noted at 12-month biopsy in 75% to 80% of men. The risk factors for treatment failure were noted to be intraprostatic calcification, failure to achieve thermal dose coverage >96%, and Prostate Imaging–Reporting and Data System >3 lesion at 12 months.40
TULSA-PRO is awaiting FDA approval, and further studies are under way to study its role in the focal therapy of PCa. The results of multiple treat-then-resect studies have been reported, indicating the safety and potential efficacy of focal TULSA. A phase 1 study investigated the feasibility of MRI-guided TULSA. Six men with 1 to 2 MRI-visible lesions far from the neurovascular bundles were enrolled. No treatment-related complications were reported in the 3 weeks leading up to RARP. At surgical pathology, no residual in-field cancer was seen.41
Discussion
Treatment of localized PCa reduces the risks of progression and PCa-specific death, but significant adverse long-term functional outcomes of prostatectomy and radiation therapy for localized PCa treatment have been well characterized. Up to 18% of patients report significant bother from urinary leakage, and 43% are bothered by sexual dysfunction at 15 years.42 AS may preserve functionality for some well-selected patients at the cost of a higher risk of progression before definitive treatment can be performed. For many intermediate-risk patients for whom the risk of progression with AS is unacceptably high, but for whom quality of life with whole-gland treatment would be too low, focal therapy offers a possible solution. This potential benefit with regard to functional preservation is well supported by the data we have discussed. Incontinence and erectile dysfunction rates for focal therapy are milder in both the maximum degree and duration of recovery when compared with rates for whole-gland therapy. Even in the most contemporary nerve-sparing robotic prostatectomy series, severe incontinence and erectile dysfunction are reported at detectable rates that are not seen in any of the focal therapy cohorts.43
However, many questions remain unanswered for every mode of focal therapy for PCa. The longest-term oncologic outcomes are 5 years for HIFU and cryoablation. Metastasis-free and cancer-specific survival are very high, as would be expected with intermediate-term outcomes. Radical whole-gland treatment is avoided in most patients, and FFS is as high as 88% in men with intermediate-risk disease 5 years following focal HIFU.8 Similarly, high radical treatment–free survival is seen with focal cryotherapy over a medium-term period, but it has been reported as low as 70% at 5 years. Many patients receiving both cryotherapy and HIFU will need repeat focal treatment for definitive cancer control.44 The majority of patients who undergo focal treatment avoid radical therapy, likely at a rate lower than those with intermediate-risk disease who initially pursue AS in contemporary protocols.2,45 However, to our knowledge, only 1 randomized trial comparing any focal therapy to AS has reported this outcome, and this was for a low-risk cohort.28 As for energy modalities beyond HIFU and cryoablation, it is unclear at this point whether similar intermediate-term outcomes will be seen.
Other considerations are the outcomes of patients who require salvage treatment after focal therapy, our understanding of which is limited to small retrospective series. Marra and colleagues conducted a systematic review of short-term oncologic and functional outcomes following radical salvage treatment after focal therapy; they found little significant difference between outcomes following primary radical treatment, but the overall quality of evidence was low.46 Another more recent series of 45 men who underwent post-HIFU prostatectomy found that one-third of men required either additional radiation or androgen deprivation therapy at 12 months postoperatively, and only 65% were pad free, suggesting worse outcomes compared with primary prostatectomy.47
Patient selection criteria for focal therapy continue to evolve as the literature matures. Various cancer risk groups have been evaluated in many of the above studies, and as would be expected, high-risk patients do not fare as well as the patients with intermediate- or low-risk disease.48 Ideal tumor location has been widely described but poorly studied. A recent retrospective article comparing focal HIFU outcomes for anterior tumors and posterior tumors found that anterior location was predictive of treatment failure on multivariate analysis.12 This has been postulated in the literature previously. Prostate swelling during treatment can shift target lesions, and this effect has been described as having an exaggerated effect on anterior lesions.13 Comparable tumor location studies for cryotherapy have not been published. However, posterior tumors are thought to be unfavorable for this modality of treatment, due to collateral tissue destruction of the neurovascular bundle that is not seen with focal HIFU.13 The effects of other clinical factors have been described as well, such as PSA >10 ng/mL; this has been demonstrated as a risk factor for treatment failure in multiple studies.48
In the AS era, a Delphi consensus statement has claimed that the ideal focal therapy candidate is a patient with a small unifocal mpMRI-visible lesion with biopsy-proven intermediate-risk disease and a maximum volume of 3 mL if confined to a single hemigland.48 What is known is that due to the intensive follow-up imaging and biopsies necessary, and the possible need for retreatment in most protocols, a high level of long-term patient adherence is required. Current guidelines do not recommend primary focal therapy outside the context of a clinical trial.
Conclusions
Focal therapy for PCa could balance undertreatment and overtreatment of localized PCa for highly selected patients. Long-term oncologic outcomes are not yet available for any modality. Intermediate-term oncologic outcomes appear promising for HIFU and cryoablation, and functional outcomes are superior to those of any form of whole-gland therapy. Patient selection remains key in the success of focal treatment modalities. Patients should be informed regarding currently available outcomes, the necessity of adherence to a stringent follow-up protocol, and the possible need for additional targeted therapy or future radical treatment in case of recurrence.
Financial Disclosure: The authors have no significant financial interest in or other relationship with the manufacturer of any product or provider of any service mentioned in this article.
References
1. Key statistics for prostate cancer. American Cancer Society. Revised January 12, 2021. Accessed April 6, 2021. https://bit.ly/31SBwPG
2. Hamdy FC, Donovan JL, Lane JA, et al; ProtecT Study Group. 10-year outcomes after monitoring, surgery, or radiotherapy for localized prostate cancer. N Engl J Med. 2016;375(15):1415-1424. doi:10.1056/NEJMoa1606220
3. Ahmed HU. The index lesion and the origin of prostate cancer. N Engl J Med. 2009;361(17):1704-1706. doi:10.1056/NEJMcibr0905562
4. Le JD, Tan N, Shkolyar E, et al. Multifocality and prostate cancer detection by multiparametric magnetic resonance imaging: correlation with whole-mount histopathology. Eur Urol. 2015;67(3):569-576. doi:10.1016/j.eururo.2014.08.079
5. Eggener SE, Scardino PT, Carroll PR, et al; International Task Force on Prostate Cancer and the Focal Lesion Paradigm. Focal therapy for localized prostate cancer: a critical appraisal of rationale and modalities. J Urol. 2007;178(6):2260-2267. doi:10.1016/j.juro.2007.08.072
6. Wise AM, Stamey TA, McNeal JE, Clayton JL. Morphologic and clinical significance of multifocal prostate cancers in radical prostatectomy specimens. Urology. 2002;60(2):264-269. doi:10.1016/s0090-4295(02)01728-4
7. Chaussy CG, Thüroff S. High-intensity focused ultrasound for the treatment of prostate cancer: a review. J Endourol. 2017;31(S1):S30-S37. doi:10.1089/end.2016.0548
8. Guillaumier S, Peters M, Arya M, et al. A multicentre study of 5-year outcomes following focal therapy in treating clinically significant nonmetastatic prostate cancer. Eur Urol. 2018;74(4):422-429. doi:10.1016/j.eururo.2018.06.006
9. Abreu AL, Peretsman S, Iwata A, et al. High intensity focused ultrasound hemigland ablation for prostate cancer: initial outcomes of a United States series. J Urol. 2020;204(4):741-747. doi:10.1097/ju.0000000000001126
10. Nahar B, Bhat A, Reis IM, et al. Prospective evaluation of focal high intensity focused ultrasound for localized prostate cancer. J Urol. 2020;204(3):483-489. doi:10.1097/ju.0000000000001015
11. Ganzer R, Arthanareeswaran VKA, Ahmed HU, et al. Which technology to select for primary focal treatment of prostate cancer? – European Section of Urotechnology (ESUT) position statement. Prostate Cancer Prostatic Dis. 2018;21(2):175-186. doi:10.1038/s41391-018-0042-0
12. Huber PM, Afzal N, Arya M, et al. Focal HIFU therapy for anterior compared to posterior prostate cancer lesions. World J Urol. Published online July 7, 2020. doi:10.1007/s00345-020-03297-7
13. Sivaraman A, Barret E. Focal therapy for prostate cancer: an “à la carte” approach. Eur Urol. 2016;69(6):973-975. doi:10.1016/j.eururo.2015.12.015
14. Shah TT, Peters M, Eldred-Evans D, et al. Early-medium-term outcomes of primary focal cryotherapy to treat nonmetastatic clinically significant prostate cancer from a prospective multicentre registry. Eur Urol. 2019;76(1):98-105. doi:10.1016/j.eururo.2018.12.030
15. Shah TT, Peters M, Miah S, et al. Assessment of return to baseline urinary and sexual function following primary focal cryotherapy for nonmetastatic prostate cancer. Eur Urol Focus. 2021;7(2):301-308. doi:10.1016/j.euf.2019.09.004
16. Tourinho-Barbosa RR, Sanchez-Salas R, Claros OR, et al. Focal therapy for localized prostate cancer with either high intensity focused ultrasound or cryoablation: a single institution experience. J Urol. 2020;203(2):320-330. doi:10.1097/ju.0000000000000506
17. Oishi M, Gill IS, Tafuri A, et al. Hemigland cryoablation of localized low, intermediate and high risk prostate cancer: oncologic and functional outcomes at 5 years. J Urol. 2019;202(6):1188-1198. doi:10.1097/ju.0000000000000456
18. Coleman JA, Scardino PT. Targeted prostate cancer ablation: energy options. Curr Opin Urol. 2013;23(2):123-128. doi:10.1097/MOU.0b013e32835d9e94
19. Moore CM, Pendse D, Emberton M. Photodynamic therapy for prostate cancer—a review of current status and future promise. Nat Clin Pract Urol. 2009;6(1):18-30. doi:10.1038/ncpuro1274
20. Azzouzi A-R, Vincendeau S, Barret E, et al; PCM301 Study Group. Padeliporfin vascular-targeted photodynamic therapy versus active surveillance in men with low-risk prostate cancer (CLIN1001 PCM301): an open-label, phase 3, randomised controlled trial. Lancet Oncol. 2017;18(2):181-191. doi:10.1016/s1470-2045(16)30661-1
21. Lebdai S, Bigot P, Leroux P-A, Berthelot L-P, Maulaz P, Azzouzi A-R. Vascular targeted photodynamic therapy with padeliporfin for low risk prostate cancer treatment: midterm oncologic outcomes. J Urol. 2017;198(2):335-344. doi:10.1016/j.juro.2017.03.119
22. Thomson KR, Kavnoudias H, Neal RE II. Introduction to irreversible electroporation—principles and techniques. Tech Vasc Interv Radiol. 2015;18(3):128-134. doi:10.1053/j.tvir.2015.06.002
23. Kiełbik A, Szlasa W, Saczko J, Kulbacka J. Electroporation-based treatments in urology. Cancers (Basel). 2020;12(8):2208. doi:10.3390/cancers12082208
24. Valerio M, Stricker PD, Ahmed HU, et al. Initial assessment of safety and clinical feasibility of irreversible electroporation in the focal treatment of prostate cancer. Prostate Cancer Prostatic Dis. 2014;17(4):343-347. doi:10.1038/pcan.2014.33
25. van den Bos W, Jurhill RR, de Bruin DM, et al. Histopathological outcomes after irreversible electroporation for prostate cancer: results of an ablate and resect study. J Urol. 2016;196(2):552-559. doi:10.1016/j.juro.2016.02.2977
26. Blazevski A, Scheltema MJ, Yuen B, et al. Oncological and quality-of-life outcomes following focal irreversible electroporation as primary treatment for localised prostate cancer: a biopsy-monitored prospective cohort. Eur Urol Oncol. 2020;3(3):283-290. doi:10.1016/j.euo.2019.04.008
27. Scheltema MJ, Chang JI, Böhm M, et al. Pair-matched patient-reported quality of life and early oncological control following focal irreversible electroporation versus robot-assisted radical prostatectomy. World J Urol. 2018;36(9):1383-1389. doi:10.1007/s00345-018-2281-z
28. Peach MS, Trifiletti DM, Libby B. Systematic review of focal prostate brachytherapy and the future implementation of image-guided prostate HDR brachytherapy using MR-ultrasound fusion. Prostate Cancer. Published online May 16, 2016. doi:10.1155/2016/4754031
29. King MT, Nguyen PL, Boldbaatar N, et al. Long-term outcomes of partial prostate treatment with magnetic resonance imaging–guided brachytherapy for patients with favorable-risk prostate cancer. Cancer. 2018;124(17):3528-3535. doi:10.1002/cncr.31568
30. Peters M, van Son MJ, Moerland MA, et al. MRI-guided ultrafocal HDR brachytherapy for localized prostate cancer: median 4-year results of a feasibility study. Int J Radiat Oncol Biol Phys. 2019;104(5):1045-1053. doi:10.1016/j.ijrobp.2019.03.032
31. Jethwa PR, Barrese JC, Gowda A, Shetty A, Danish SF. Magnetic resonance thermometry–guided laser-induced thermal therapy for intracranial neoplasms: initial experience. Neurosurgery. 2012;71(1 Suppl Operative):133-144; 144-145. doi:10.1227/NEU.0b013e31826101d4
32. Eggener SE, Yousuf A, Watson S, Wang S, Oto A. Phase II evaluation of magnetic resonance imaging guided focal laser ablation of prostate cancer. J Urol. 2016;196(6):1670-1675. doi:10.1016/j.juro.2016.07.074
33. Lepor H, Llukani E, Sperling D, Fütterer JJ. Complications, recovery, and early functional outcomes and oncologic control following in-bore focal laser ablation of prostate cancer. Eur Urol. 2015;68(6):924-926. doi:10.1016/j.eururo.2015.04.029
34. Walser E, Nance A, Ynalvez L, et al. Focal laser ablation of prostate cancer: results in 120 patients with low- to intermediate-risk disease. J Vasc Interv Radiol. 2019;30(3):401-409.e2. doi:10.1016/j.jvir.2018.09.016
35. Chao B, Llukani E, Lepor H. Two-year outcomes following focal laser ablation of localized prostate cancer. Eur Urol Oncol. 2018;1(2):129-133. doi:10.1016/j.euo.2018.03.011
36. van Luijtelaar A, Greenwood BM, Ahmed HU, et al. Focal laser ablation as clinical treatment of prostate cancer: report from a Delphi consensus project. World J Urol. 2019;37(10):2147-2153. doi:10.1007/s00345-019-02636-7
37. Valerio M, Cerantola Y, Eggener SE, et al. New and established technology in focal ablation of the prostate: a systematic review. Eur Urol. 2017;71(1):17-34. doi:10.1016/j.eururo.2016.08.044
38. Orczyk C, Barratt D, Brew-Graves C, et al. Prostate Radiofrequency Focal Ablation (ProRAFT) trial: a prospective development study evaluating a bipolar radiofrequency device to treat prostate cancer. J Urol. 2021;205(4):1090-1099. doi:10.1097/ju.0000000000001567
39. Villers A, Puech P, Flamand V, et al. Partial prostatectomy for anterior cancer: short-term oncologic and functional outcomes. Eur Urol. 2017;72(3):333-342. doi:10.1016/j.eururo.2016.08.057
40. Klotz L, Pavlovich CP, Chin J, et al. MRI-guided transurethral ultrasound ablation of prostate cancer. J Urol. 2021;205(3):769-779. doi:10.1097/ju.0000000000001362
41. Anttinen M, Mäkelä P, Suomi V, et al. Feasibility of MRI-guided transurethral ultrasound for lesion-targeted ablation of prostate cancer. Scand J Urol. 2019;53(5):295-302. doi:10.1080/21681805.2019.1660707
42. Resnick MJ, Koyama T, Fan KH, et al. Long-term functional outcomes after treatment for localized prostate cancer. N Engl J Med. 2013;368(5):436-445. doi:10.1056/NEJMoa1209978
43. Bhat KRS, Raghunath SK, Srivatsa N, Tejus C, Vishruth K, Kumar RA. Outcomes of minimally invasive radical prostatectomy – a contemporary review. Indian J Surg Oncol. 2020;11(4):580-588. doi:10.1007/s13193-020-01125-3
44. Stabile A, Orczyk C, Hosking-Jervis F, et al. Medium-term oncological outcomes in a large cohort of men treated with either focal or hemi-ablation using high-intensity focused ultrasonography for primary localized prostate cancer. BJU Int. 2019;124(3):431-440. doi:10.1111/bju.14710
45. Carlsson S, Benfante N, Alvim R, et al. Long-term outcomes of active surveillance for prostate cancer: the Memorial Sloan Kettering Cancer Center experience. J Urol. 2020;203(6):1122-1127. doi:10.1097/ju.0000000000000713
46. Marra G, Gontero P, Walz JC, et al. Complications, oncological and functional outcomes of salvage treatment options following focal therapy for localized prostate cancer: a systematic review and a comprehensive narrative review. World J Urol. 2019;37(8):1517-1534. doi:10.1007/s00345-019-02642-9
47. Thompson JE, Sridhar AN, Tan WS, et al. Pathological findings and magnetic resonance imaging concordance at salvage radical prostatectomy for local recurrence following partial ablation using high intensity focused ultrasound. J Urol. 2019;201(6):1134-1143. doi:10.1097/ju.0000000000000135
48. Tay KJ, Scheltema MJ, Ahmed HU, et al. Patient selection for prostate focal therapy in the era of active surveillance: an International Delphi Consensus Project. Prostate Cancer Prostatic Dis. 2017;20(3):294-299. doi:10.1038/pcan.2017.8
Prolaris in Practice: Guiding ADT Benefits, Clinical Application, and Expert Insights From ACRO 2025
April 15th 2025Steven E. Finkelstein, MD, DABR, FACRO discuses how Prolaris distinguishes itself from other genomic biomarker platforms by providing uniquely actionable clinical information that quantifies the absolute benefit of androgen deprivation therapy when added to radiation therapy, offering clinicians a more precise tool for personalizing prostate cancer treatment strategies.