Squamous Cell Carcinoma of the Kidney: A Large Case Series
Syed Arslan Shehzad Shah, MD, and colleagues present findings from a broad investigation into this rare neoplasm of the kidney, including data on patient demographics and mean survival.
ABSTRACT
Objectives: We present our experience with and data about a very rare neoplasm of the kidney, squamous cell carcinoma (SCC).
Methods: A total of 14 patients with a diagnosis of SCC were identified on the basis of a retrospective analysis of medical records of patients who underwent surgery for renal cancers between 2015 and 2021 at the Sindh Institute of Urology and Transplantation. IBM SPSS v25 was used to record and analyze data.
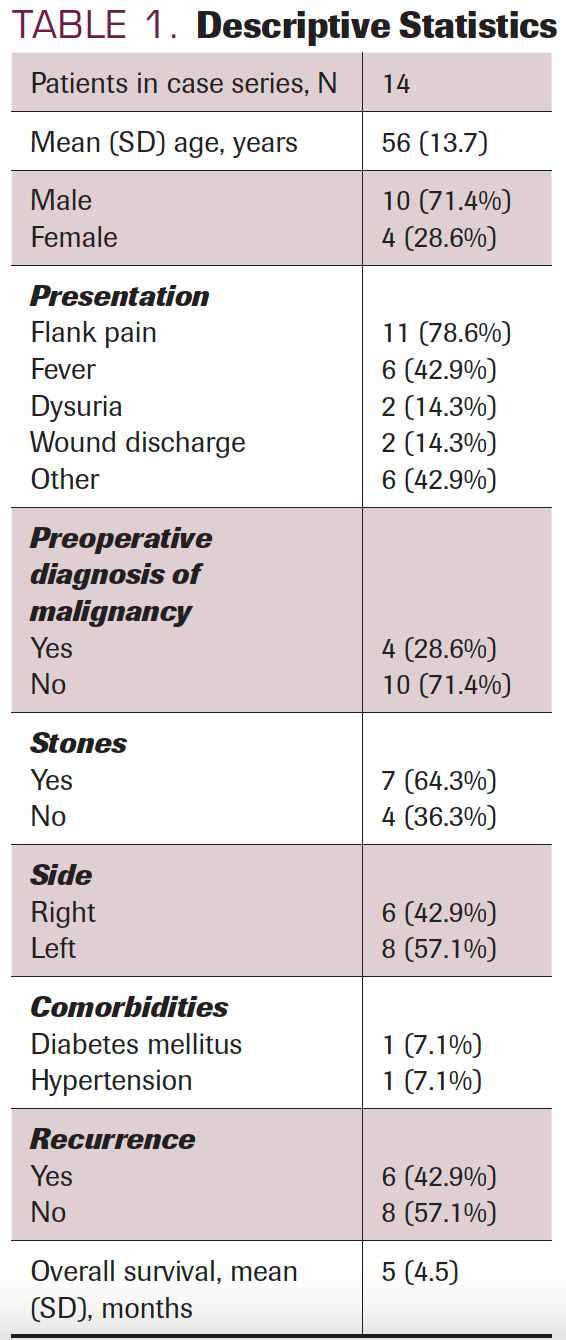
Results: Most patients found to have SCC of the kidney were male (71.4%). The mean (SD) patient age was 56 (13.7) years. Flank pain was the most common presenting symptom (n = 11; 78.6%) followed by fever (n = 6; 42.9%). Only 4 (28.5%) of the 14 patients had a preoperatively established diagnosis of SCC; the remaining 10 (71.4%) had an incidental finding of SCC on their histopathology specimen. The mean (SD) overall survival was 5 (4.5) months.
Conclusions: SCC of the kidney is a rare upper urinary tract neoplasm reported in the literature. The gradual onset of vague symptoms, lack of pathognomonic signs, and inconclusive radiological features make the disease unsuspected in most cases, therefore delaying diagnosis and treatment. It usually presents at an advanced stage, and the prognosis is often poor. A high index of suspicion is warranted in patients with chronic kidney stone disease.
Oncology (Williston Park). 2023;37(6):246-249.
DOI: 10.46883/2023.25920997
Introduction
Squamous cell carcinoma (SCC) of the kidney is an extremely rare neoplasm and accounts for less than 1% of all malignant renal tumors.1-4 The gradual onset of vague symptoms, lack of pathognomonic signs, and inconclusive radiological features make the disease unsuspected in most cases, therefore delaying diagnosis and treatment.5 The disease is reported to be associated with renal calculi, radiotherapy, infections, and other factors that chronically irritate the urothelium. Because of its rarity and lack of specific clinical and radiological features, it is diagnosed only after a nonfunctioning kidney has been removed for local symptoms.2,3,5 Here, we report a case series of incidentally detected SCC of the kidney. To the best of our knowledge, only a few similar cases have previously been published.
Methods
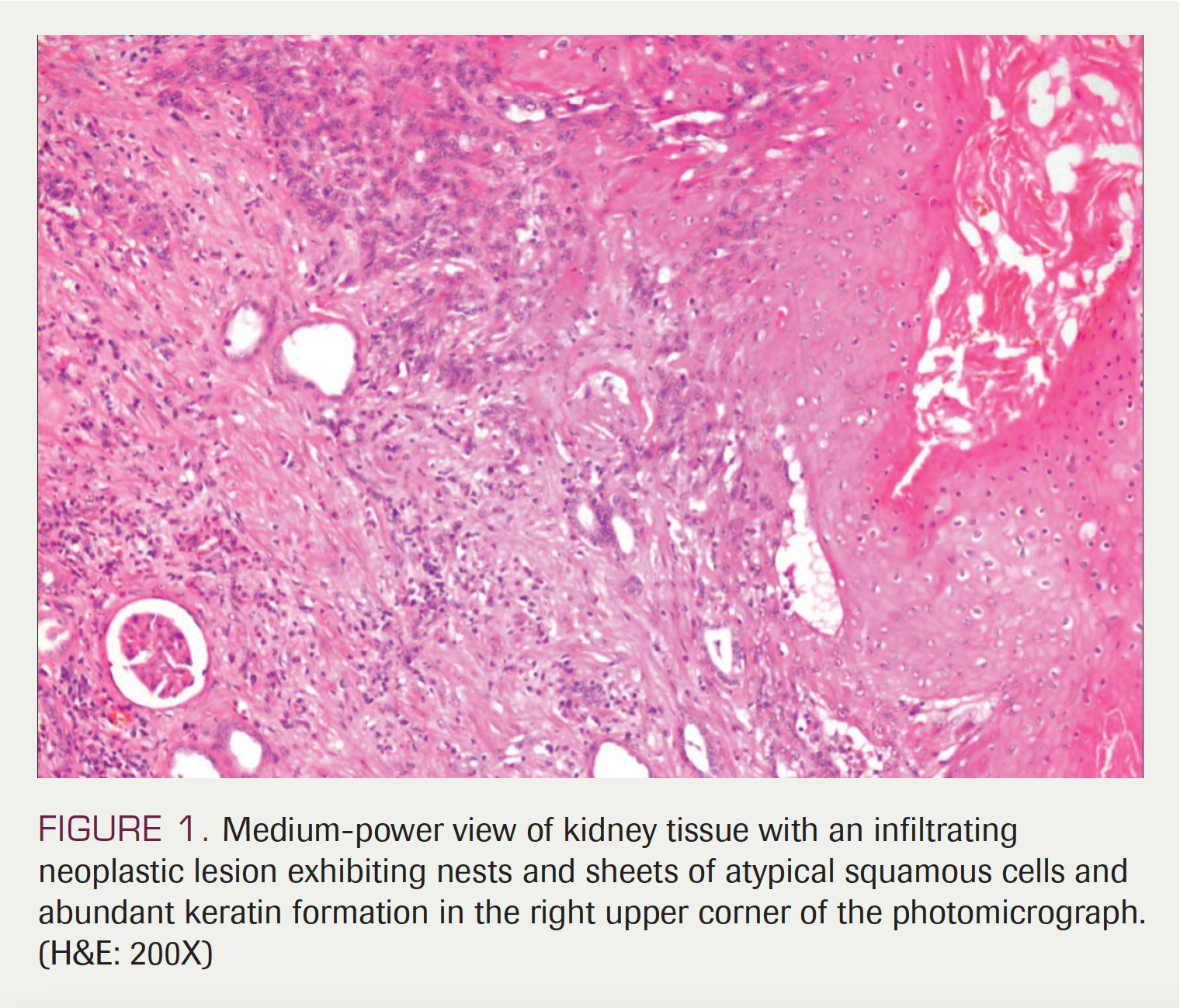
Among the 2534 patients who underwent nephrectomy at the Sindh Institute of Urology and Transplantation between January 2015 and December 2021, 14 cases of SCC of the kidney were identified. All patients’ medical records were reviewed retrospectively. The majority of the patients had an incidental finding of SCC of the kidney on postoperative histopathological examination of the specimen for simple nephrectomy of the nonfunctioning or pyonephrotic kidney, secondary to long-standing kidney stone disease. All patients received regular laboratory and radiological evaluations, including an ultrasound of the renal bed and a plain chest x-ray on follow-up. Patients who had an incidental finding of SCC on histopathology underwent more extensive postoperative radiological examination with contrast-enhanced CT scans of the chest, abdomen, and pelvis to rule out local recurrence and distant metastasis. Contrast-enhanced CT scans were also performed for patients who had signs of recurrence on a follow-up ultrasound. The surgery and postoperative course of most patients remained uneventful; 2 patients developed purulent discharge from wounds that mimicked discharging sinus. Six patients whose nonfunctioning kidneys were surgically removed were found to have residual disease on postoperative radiological examination, and they underwent residual disease excision. Two of the 10 patients who had an incidental finding of SCC on histopathology (Figure 1) were found to have metastatic nodules in the lungs. None of the patients consented for chemotherapy; 6 patients received radiation therapy as part of pain management for secondary bony metastases. All 14 patients died because of extensive disease metastasis. IBM SPSS v25 was used to analyze the data.
Results
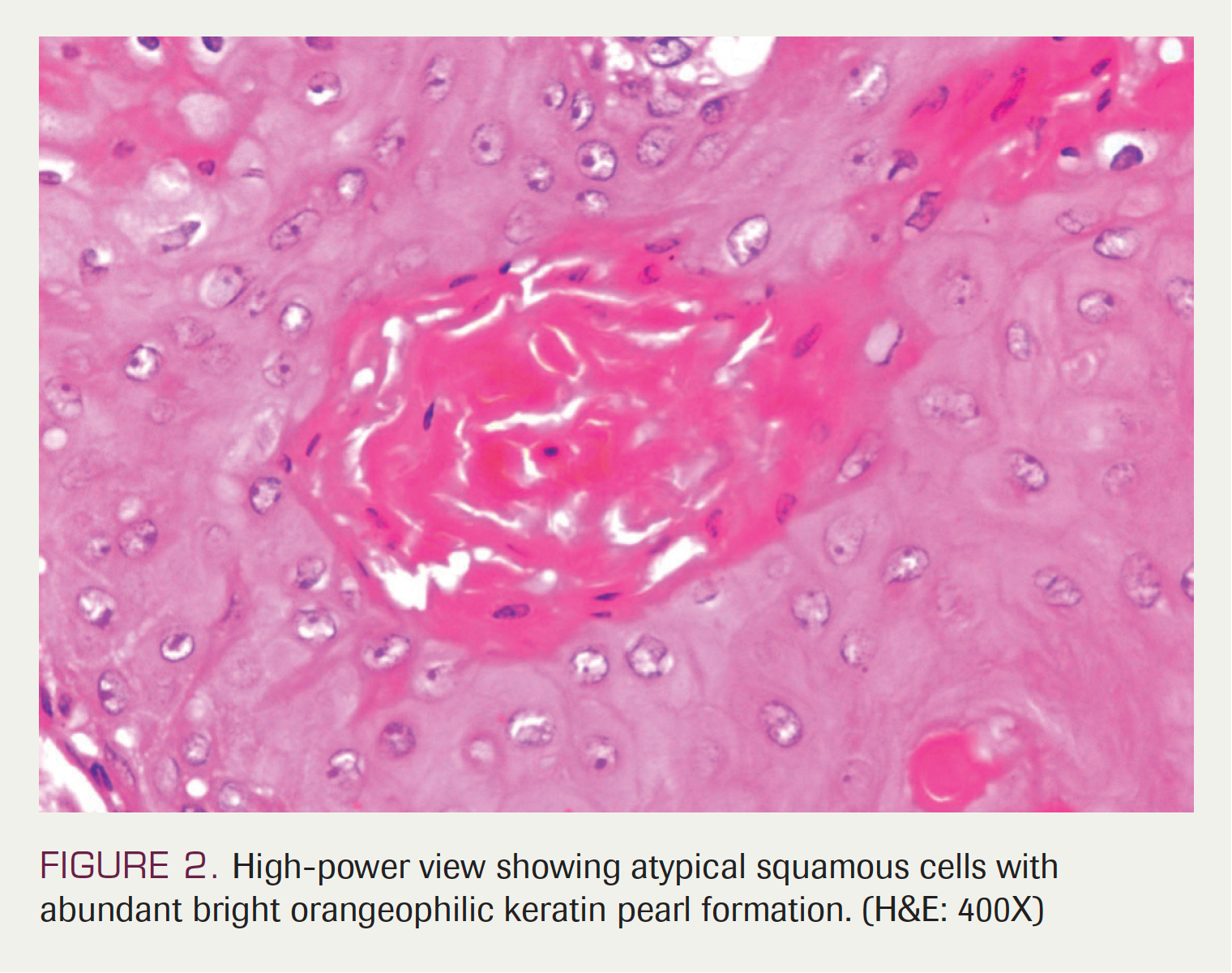
The mean (SD) age of the 14 patients was 56 (13.7) years, and 10 (71.4%) were male. Only 2 patients had reported comorbidities; one had diabetes and the other had hypertension. The modes of presentation were flank pain (n = 11; 78.6%), fever (n = 6; 42.9%), dysuria (n = 2; 14.3%), and wound discharge after surgery (n = 2; 14.3%). A history of renal stones was found in 9 (64.3%) patients, and 5 (35.7%) patients had renal failure. In 2 cases (14.3%), there was a suspicion of renal cell carcinoma (RCC), and in another 2 (14.3%) patients, transitional cell carcinoma of the kidney was suspected before surgery. The other 10 patients (71.4%) were having surgery to remove a nonfunctioning kidney; SCC was later diagnosed when the histopathological evaluation was completed (Figure 1 and Figure 2). The disease recurred in 6 (42.9%) of the patients. The mean (SD) overall survival (OS) of patients was 5 (4.5) months. For descriptive statistics see Table 1.
Discussion
Cancers of the kidney parenchyma and pelvis are the ninth and 12th most common causes of all cancer-related deaths.6 SCC of the renal pelvis is an extremely rare, and an aggressive tumor that presents at an advanced stage and is known to arise from the collecting system. It accounts for less than 1% of all renal malignancies. Tumors arising from the urothelium of the renal pelvis and ureter are relatively rare neoplasms, making up 5% to 10% of all urothelial tumors. Approximately 85% to 90% of upper urinary tract malignancies are urothelial carcinomas, while pure SCCs account for just 0.5% to 7.0%.1,5,7
Despite the rarity of this kidney tumor, this differential diagnosis should be investigated when a renal mass is accompanied by longstanding renal calculi. Factors that enhance the likelihood of SCC are chronic irritation, inflammation, and infections that promote squamous metaplasia of the renal pelvic epithelium. Chronic pyelonephritis or nephrolithiasis is frequently present in the pertinent medical history of SCC.8
Clinically, SCC tends to manifest in middle age (the fifth to seventh decades of life),6,9 with a mean age at diagnosis of 56 years, and it affects males and females about equally. Our study found similar results, with a mean (SD) age of 56 (13.7) years. However, in our study, 10 of 14 of patients (71.4%) were male.
The modes of presentation reported in the literature include flank pain, hematuria, fever, anorexia, and weight loss.5 These symptoms are often indistinguishable from those of the most common types of renal cancer. Most of the patients included in this series presented with flank pain, fever, dysuria, and wound discharge. Significantly, most instances of primary renal SCC are misdiagnosed, at least initially, because of the vague clinical symptoms and lack of distinct radiological diagnostic characteristics.8,9
The nonspecific nature of symptoms makes diagnosis and subsequent treatment difficult. There are currently no standard guidelines or treatment protocols for the management of patients with primary renal SCC.
According to research, factors that promote chronic urothelial injuries, such as renal calculi, radiotherapy, analgesic abuse, and infection, cause squamous metaplasia, which can progress to SCC.10 In our study, renal stones were found in 64.3% of patients.
Unfortunately, a correct preoperative diagnosis of SCC is usually not made because patients’ symptoms and radiological findings often mirror those of simple nonfunctioning kidneys secondary to stones or infection. SCC can be definitively diagnosed only when it is confirmed that a tumor exhibits squamous differentiation and specific histological signs, including the production of keratin pearls, intercellular bridges, and keratotic debris. A solid renal pelvic or ureteric mass, hydronephrosis, calcifications, or localized lymphadenopathy are radiological signs of renal pelvis SCC. These are nonspecific features that could be challenging to differentiate from those of other upper urinary tract neoplasms or other chronic inflammatory illnesses such as tuberculosis or xanthogranulomatous pyelonephritis.11,12,13,14
Ultrasonography typically reveals only hydronephrosis. However, CT is an important tool and can provide high-resolution imaging to evaluate masses and stages in renal malignancies.13,15 Therefore ultrasound results only in incomplete staging and subsequent surgical planning for the removal of a presumed noncancerous kidney. In this series, only 4 cases (28.6%) were suspected of having malignancy—2 (14.3%) each of transitional cell carcinoma and RCC—before surgery, and the rest of the cases (71.4%) were operated on for a presumed nonfunctioning kidney. All of these cases turned out to be SCC after complete histopathological assessment.
Skin lesions caused by renal SCC are relatively uncommon. A fistula between the skin of the lumbar region and the kidney pole has been described in few case reports.14 Two (14.3%) patients in our case series also developed postoperative cutaneous discharging sinus.
The cornerstone of SCC therapy has been radical surgery (ie, radical nephroureterectomy) for patients with disease localized to the kidney.7-10,12,13,16 Nephrectomy is often necessary for metastatic disease to control symptoms and sometimes to establish the pathological diagnosis. Adjuvant cisplatin-based chemotherapy and palliative radiotherapy in metastatic cases have also been advocated for the control of symptoms, but their effect on survival is unknown.5 Further large studies are required to establish the appropriate treatment for such patients. None of the patients in our case series consented for chemotherapy, but radiation therapy was offered to and received by 6 patients who had developed bony metastases.
It has been reported that the probability of 5-year survival is less than 10% and the mean OS is around 7 months.17 In this series, disease recurrence was noted in 42.9% of patients at 3 months, and the mean (SD) OS was 5 (4.5) months.
The scarcity of data, lack of guidelines, and retrospective nature of this case series remain the study’s main limitations, which influenced our ability to draw conclusions regarding OS as well as to make concrete recommendations about when and how to apply diagnostic and treatment tools.
Conclusions
SCC of the renal pelvis is a rare tumor and is most often diagnosed postoperatively after nephrectomy for a presumed noncancerous kidney. The index of suspicion of malignancy should be high in cases of nonfunctioning kidneys with a long history of renal stones and infections. Such cases should be evaluated preoperatively by contrast-enhanced CT scans to establish the diagnosis of malignancy and achieve complete staging.
AUTHOR AFFILIATIONS:
Syed Arslan Shehzad Shah, MD;1 Naveed Ahmed Mahar, MMBS, FCPS;2 Harris Hassan Qureshi, MMBS, FCPS;3 Muddasir Hussain, MMBS, FCPS;4 Gauhar Sultan, MMBS, FCPS;5 Rehan Mohsin, MMBS, FCPS;6 Altaf Hashmi, MMBS, MS7
1Department of Urology, Sindh Institute of Urology and Transplantation, Karachi, Pakistan; syedarslanshehzad@gmail.com
2Department of Urology, Sindh Institute of Urology and Transplantation, Karachi, Pakistan; navidmahardowite@gmail.com
3Department of Urology, Sindh Institute of Urology and Transplantation, Karachi, Pakistan; dr_hhq@live.com
4Department of Urology, Sindh Institute of Urology and Transplantation, Karachi, Pakistan; mudassir. hussain120@gmail.com
5Department of Urology, Sindh Institute of Urology and Transplantation, Karachi, Pakistan; gauhar.sultan66@gmail.com
6Department of Urology, Sindh Institute of Urology and Transplantation, Karachi, Pakistan; rhmohsin@yahoo.com
7Department of Urology, Sindh Institute of Urology and Transplantation, Karachi, Pakistan; hashmi.altaf@gmail. com
CORRESPONDING AUTHOR:
Syed Arslan Shehzad Shah, MD
Resident Urology
Department of Urology
Sindh Institute of Urology & Transplantation
Sardar Yaqoob Ali Khan Road, Near Civil Hospital
Karachi, Pakistan
Tel: +92300.8761792
Email: syedarslanshehzad@gmail.com
ORCID ID: 0000-0002-1656-1887
Conflict of Interest: None of the authors have any conflict of interest to disclose.
Financial Disclosures: None
REFERENCES
- Brits NF, Bulane S, Wadee R. Primary squamous cell carcinoma of the kidney: a case report and review of the literature. Afr J Urol. 2020;26(79). doi:10.1186/s12301-020-00088-9
- Palmer CJ, Atty C, Sekosan M, Hollowell CMP, Wille MA. Squamous cell carcinoma of the renal pelvis. Urology. 2014;84(1):8-11. doi:10.1016/j.urology.2013.11.020
- Paonessa J, Beck H, Cook S. Squamous cell carcinoma of the renal pelvis associated with kidney stones: a case report. Med Oncol. 2011;28 Suppl 1:S392-S324. doi:10.1007/s12032-010-9704-z
- Jiang P, Wang C, Chen S, Li J, Xiang J, Xie L. Primary renal squamous cell carcinoma mimicking the renal cyst: a case report and review of the recent literature. BMC Urol. 2015;15:69. doi:10.1186/s12894-015-0064-z
- Nachiappan M, Litake MM, Paravatraj VG, Sharma N, Narasimhan A. Squamous cell carcinoma of the renal pelvis, a rare site for a commonly known malignancy. J Clin Diagn Res. 2016;10(1):PD04-PD06. doi:10.7860/JCDR/2016/17846.7081
- Singh V, Sinha RJ, Sankhwar SN, Mehrotra B, Ahmed N, Mehrotra S. Squamous cell carcinoma of the kidney—rarity redefined: case series with a review of the literature. J Cancer Sci Ther. 2010;2(4):82-85. doi:10.4172/1948-5956.1000028
- Holmäng S, Lele SM, Johansson SL. Squamous cell carcinoma of the renal pelvis and ureter: incidence, symptoms, treatment and outcome. J Urol. 2007;178(1):51-56. doi:10.1016/j.juro.2007.03.033
- Hosseinzadeh M, Mohammadzadeh S. Primary pure squamous cell carcinoma of kidney associated with multiple stag horn stones. Int Med Case Rep J. 2020;13:261-263. doi:10.2147/IMCRJ.S261022
- Blacher EJ, Johnson DE, Abdul-Karim FW, Ayala AG. Squamous cell carcinoma of renal pelvis. Urology. 1985;25(2):124-126. doi:10.1016/0090-4295(85)90526-6
- Busby JE, Brown GA, Tamboli P, et al. Upper urinary tract tumors with nontransitional histology: a single-center experience. Urology. 2006;67(3):518-523. doi:10.1016/j.urology.2005.09.010
- Bandyopadhyay R, Biswas S, Nag D, Ghosh AK. Squamous cell carcinoma of the renal pelvis presenting as hydronephrosis. J Cancer Res Ther. 2010;6(4):537-539. doi:10.4103/0973-1482.77060
- Hameed ZBM, Pillai SB, Hegde P, Talengala BS. Squamous cell carcinoma of the renal pelvis presenting as sacral bone metastasis. BMJ Case Rep. 2014;2014:bcr2013201719. doi:10.1136/bcr-2013-201719
- Zhang X, Zhang Y, Ge C, Zhang J, Liang P. Squamous cell carcinoma of the renal parenchyma presenting as hydronephrosis: a case report and review of the recent literature. BMC Urol. 2020;20(1):107. doi:10.1186/s12894-020-00676-5
- Sun X, Li Y. Incidental squamous cell carcinoma of renal pelvis presenting as skin invasion: a case report. J Med Case Rep. 2020;14(1):244. doi:10.1186/s13256-020-02530-6
- Lynch CF, West MM, Davile JA, Pletz CE. Cancers of the kidney and renal pelvis. In: Ries LAG, Young JL, Keel GE, Eisner MP, Lin YD, Horner M-J, eds. SEER Survival Monograph: Cancer Survival Among Adults: U.S. SEER Program, 1988-2001, Patient and Tumor Characteristics. National Cancer Institute; 2007.
- Booth CM, Cameron KM, Pugh RC. Urothelial carcinoma of the kidney and ureter. Br J Urol. 1980;52(6):430-435. doi:10.1111/j.1464-410x.1980.tb03083.x
- Holmäng S, Johansson SL. Impact of diagnostic and treatment delay on survival in patients with renal pelvic and ureteral cancer. Scand J Urol Nephrol. 2006;40(6):479-484. doi:10.1080/00365590600864093