Radiation Therapy in the Management of Diffuse Large B-Cell Lymphoma: Still Relevant?
The effectiveness of RT in the palliative setting is sometimes overlooked; however, RT can provide excellent palliation for patients whose disease becomes refractory to other modalities.
Diffuse large B-cell lymphoma (DLBCL) is the most common subtype of non-Hodgkin lymphoma in the United States. Historically, radiation therapy (RT) was the primary treatment for patients with localized disease. Several randomized trials have demonstrated that the addition of systemic therapy improves outcomes. Additional randomized trials have shown that the combination of RT and systemic therapy is superior to systemic therapy alone. The role of RT in advanced-stage DLBCL has not been firmly established, but some prospective phase III trials, as well as retrospective studies, suggest a benefit for advanced disease also. For patients with relapsed or primary refractory disease, autologous stem cell transplantation is the treatment of choice. Here too, consolidation RT appears to improve outcomes compared with autologous stem cell transplant alone. Finally, for patients with advanced DLBCL who are no longer responsive to systemic therapy, RT may provide rapid and durable palliation of local lymphoma-related symptoms.
Diffuse large B-cell lymphoma (DLBCL) is the most common subtype of non-Hodgkin lymphoma in the United States, comprising approximately 30% to 40% of cases.[1] Currently, the World Health Organization recognizes multiple entities with distinct clinical or pathological features that were previously identified nonspecifically as DLBCL, including primary mediastinal DLBCL and T-cell/histiocyte-rich B-cell lymphoma. Furthermore, gene expression microarray or immunohistochemistry analyses can identify distinct subtypes of DLBCL (eg, germinal center B-cell–like, activated B-cell–like, etc), which have prognostic relevance.[2,3]
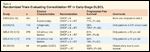
TABLE 1

Randomized Trials Evaluating the Addition of Chemotherapy in Non-Hodgkin Lymphoma (NHL)
Historically, radiation therapy (RT) was the primary treatment for patients with localized DLBCL. Several randomized trials conducted in the 1970s demonstrated that the addition of chemotherapy, primarily CVP (cyclophosphamide, vincristine, prednisone), to RT significantly decreased the risk of relapse for patients with stage I-II disease (Table 1).[4-7] Outcomes were further improved by the addition of anthracyclines. The major advance in systemic therapy in the last two decades, however, has been the introduction of the anti-CD20 antibody rituximab.[8,9] The addition of rituximab to a variety of combination chemotherapy programs significantly improves outcomes, such that R-CHOP (rituximab plus cyclophosphamide, adriamycin, vincristine, prednisone) has now become the systemic therapy of choice for both localized and advanced disease.
The rationale for consolidation RT for both localized and advanced disease is based on the observation that the majority of patients who relapse after receiving chemotherapy alone for DLBCL fail at originally involved sites. Multiple randomized trials have shown that consolidation RT decreases the risk of relapse and improves clinical outcomes. This benefit has been observed in both localized and advanced disease but is sometimes obscured by the peculiarities and complexities of the individual studies. This review endeavors to clarify the role of RT in the current management of patients with DLBCL by critically evaluating and putting into context the individual studies.
Stage I-II Disease
Historically, RT alone was the treatment of choice for localized DLBCL, producing complete response rates of 85% to 95% and long-term freedom from relapse in 30% to 55% of patients.[6,7,10,11] Patients with stage I disease fared considerably better than patients with stage II disease.[10,12] Adjuvant chemotherapy was added in an attempt to improve these outcomes, with positive results-first for the combination of CVP, then for the addition of anthracyclines to the CVP program (Table 1).
TABLE 2
Randomized Trials Evaluating Consolidation RT in Early-Stage DLBCL
After improved outcomes were seen with the combination of chemotherapy and RT for localized disease, the question was raised whether chemotherapy alone would be sufficient. Studies were carried out comparing combination chemotherapy with and without RT. Five randomized trials have now addressed this question (Table 2). All of these studies antedate the use of rituximab and the widespread use of functional imaging.
The optimal study design to assess the value of consolidation RT would be to randomly assign patients to RT or observation after receipt of the same chemotherapy regimen. Two of the above trials used this strategy (Eastern Cooperative Oncology Group [ECOG] 1484 and Group d’tude des Lymphomas de l’Adulte [GELA] LNH 93-4). Three of the trials evaluated whether RT would allow for fewer cycles of chemotherapy (Southwest Oncology Group [SWOG] 8736 and International Extranodal Lymphoma Study Group [IELSG] 4) or less intense chemotherapy (GELA 93-1). These studies are more difficult to interpret because the randomization scheme has two variables in the experimental arm-the addition of RT and the subtraction of some chemotherapy.
ECOG 1484
This study enrolled patients with early-stage (bulky stage I, IE, or II), diffuse aggressive lymphomas; DLBCL constituted 80% of cases.[13] Of the 352 eligible patients, 68% had stage II disease and 31% had disease larger than 10 cm-a population with a more unfavorable prognosis compared with the those of the SWOG and GELA 93-4 studies discussed below. All patients received 8 cycles of CHOP. If a complete response was achieved (as assessed by CT imaging), patients were randomly assigned to either consolidation RT (30 Gy) or observation. All patients who achieved a partial response received RT to a somewhat higher dose (40 Gy). The primary endpoint was disease-free survival; the study was powered to detect a 20% improvement at 2 years in patients who received RT after achieving a complete response with chemotherapy.
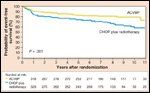
FIGURE 1
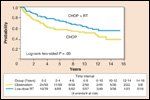
Comparison of CHOP Followed by Observation Versus CHOP Followed by Consolidation RT in Patients With Early-Stage, Diffuse Aggressive Lymphomas
The addition of consolidation RT in patients who achieved a complete response to CHOP was associated with improved disease-free survival (Figure 1). Disease-free survival at 6 years was 73% with consolidation RT versus 56% with observation (P = .05). Crude rates of local failure were 4% with consolidation RT vs 16% with observation (P = .06). While short-term survival was statistically improved with consolidation RT, with longer follow-up (and smaller numbers of patients at risk) that benefit diminished. Overall survival at 5, 10, and 15 years was 87%, 68%, and 60% with consolidation RT vs 73%, 65%, and 44% with observation (P = .24).
Of the patients with a partial response after chemotherapy, 31% converted to a complete response with RT. Disease-free survival in patients who received RT (40 Gy) after achieving a partial response to chemotherapy was ~60% at 6 years. These excellent results in partial-response patients may reflect the efficacy of consolidation RT as well as the limitations of CT imaging to assess response to chemotherapy.
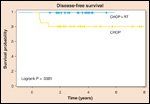
FIGURE 2
Comparison of CHOP Versus CHOP Followed by Consolidation RT in Patients With Early-Stage, Aggressive Non-Hodgkin Lymphoma
GELA LNH 93-4
This study enrolled older patients (aged 60 years or older) with early-stage aggressive non-Hodgkin lymphoma (80% DLBCL) without risk factors such as elevated lactate dehydrogenase level or poor performance status.[14] Patients (n=576) were randomly assigned to receive either 4 cycles of CHOP or 4 cycles of CHOP plus consolidation RT (40 Gy). The median age was 68, and 65% had stage I disease. The primary endpoint was event-free survival, and the study was powered to detect a 10% improvement at 2 years.
With a median follow-up of 7 years, there was no difference in event-free survival (61% vs 64%, P = .6) (Figure 2) or overall survival (72% vs 68%, P = .5) between patients receiving consolidation RT and those not receiving it. Crude rates of local failure were lower in patients who received RT (7% vs 18%).
SWOG 8736
This study evaluated whether the addition of consolidation RT would allow for fewer cycles of chemotherapy. Patients with intermediate- or high-grade non-Hodgkin lymphoma (75% DLBCL) with stage I or non-bulky (smaller than 10 cm) stage II disease were eligible.[15] Patients were randomly assigned to receive either 8 cycles of CHOP or 3 cycles of CHOP plus consolidation RT (40 to 55 Gy, depending on response to chemotherapy). Among the 401 eligible patients, 67% had stage I disease.
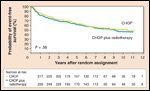
FIGURE 3
Comparison of 8 cycles of CHOP Versus 3 cycles of CHOP Plus RT in Patients With Intermediate- or High-Grade Non-Hodgkin Lymphoma
As expected, life-threatening toxicity, primarily neutropenia and decreased left ventricular function, was higher among patients who received 8 cycles of CHOP (40% vs 30%, P = .06). When the study was initially published, the combination of 3 cycles of CHOP plus consolidation RT was associated with improved 5-year progression-free survival (77% vs 64%, P = .03) (Figure 3) and overall survival (82% vs 72%, P = .02). With longer follow-up, 5-year overall survival remained significantly different (82% vs 74%), but mortality related to relapse between years 5 and 10 was increased in the CHOP × 3 plus RT group. These late relapses negated the initial improvement in outcomes.[16] These later results have only been reported in abstract form, necessitating caution in interpreting the “final” results of this study. Nevertheless, the SWOG update suggests that a limited number of chemotherapy cycles may be inadequate to control systemic disease long term in some early-stage patients.
GELA 93-1
This study enrolled younger patients (no older than 61 years) with stage I-II aggressive non-Hodgkin lymphoma (81% DLBCL) without risk factors.[17] Patients were randomly assigned to receive either an aggressive induction chemotherapy regimen (3 cycles of ACVBP [doxorubicin, cyclophosphamide, vindesine, bleomycin, and prednisone] followed by consolidation chemotherapy consisting of methotrexate, etoposide, ifosfamide and cytarabine) or 3 cycles of CHOP and consolidation RT (40 Gy). The primary endpoint of the study was 2-year event-free survival; the study was powered to detect an absolute improvement of 10% with intense chemotherapy without RT.
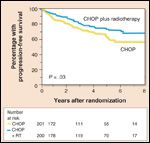
FIGURE 4
Comparison of ACVBP × 3 Plus Consolidation Chemotherapy Versus CHOP × 3 Plus Consolidation RT in Younger Patients With Stage I-II Aggressive Non-Hodgkin Lymphoma
Although a complete response occurred in ~93% of patients in both groups, event-free survival was better in the intensive chemotherapy arm. Five-year estimates were 82% in the intense chemotherapy arm vs 74% with CHOP plus RT (P < .01) (Figure 4). Five-year survival was also better in the intense chemotherapy arm (90% vs 81%, P = .001). The proportion of first failures that included originally involved sites was lower in the patients receiving RT (28% vs 62%). It is also of interest that the total number of relapses in the intense chemotherapy arm comprised 13% of the patients in that group (42/318), while the number of relapses in non-irradiated sites in the CHOP plus RT arm involved 17% of the patients in that group (56/329)-again pointing toward a failure of limited chemotherapy to control systemic disease.
As with the SWOG study, the intensive chemotherapy arm experienced greater toxicity, with grade III infection in 11% of patients-compared with 1% of patients in the CHOP plus RT arm. Because of the substantial toxicity seen with the intense chemotherapy regimen, this program has not been widely adopted. In addition, it is likely that 3 cycles of CHOP is inadequate therapy; outcomes might have been better with 4 to 6 cycles of CHOP plus RT.
IELSG 4 (Gastric DLBCL)
This multicenter study, reported by Martinelli and colleagues, enrolled patients with high-grade non-Hodgkin lymphoma of the stomach (stage I-II) who achieved a complete response as assessed by CT and endoscopy after an anthracycline-containing regimen.[18] Patients who achieved a complete response after 4 cycles of chemotherapy were randomly assigned to receive either consolidation RT (minimum of 30 Gy) or 2 additional cycles of chemotherapy. Patients with a partial response after 4 cycles received an additional 2 cycles of chemotherapy, and if they then achieved a complete response, they were randomly assigned to either radiation or observation. The primary endpoint was 2-year disease-free survival; the study was powered to detect a 30% improvement with RT. Due to poor accrual, the study was closed after 55 of a planned 125 patients had been enrolled.
FIGURE 5
Comparison of 2 Additional Cycles of Chemotherapy Versus Consolidation RT in Patients With High-Grade Non-Hodgkin Lymphoma of the Stomach Who Achieved a CR With Initial Chemotherapy
Consolidation RT was well tolerated without major complications. Four patients in the chemotherapy-alone arm experienced failure (3 local failures and 1 distant failure); however, there were no failures after consolidation RT, resulting in a disease-free survival of 100% with RT-compared with 82% in patients without RT (P = .04) (Figure 5). There was no difference in overall survival.
Taken together, these studies support the following conclusions:
• Consolidation RT decreases the risk of relapse at treated sites and hence the overall risk of relapse.
• For adequate systemic control, more than 3 cycles of CHOP (or R-CHOP) are probably required, except in the most favorable cases.
• Increasingly effective systemic therapies may decrease the absolute benefit of consolidation RT, but possibly at the expense of increased toxicity.
• Older patients, especially those whose disease has a favorable prognosis and/or who have serious medical comorbidities, may derive less benefit from consolidation RT than younger patients.
Rituximab
The addition of the anti-CD20 antibody rituximab has improved the efficacy of systemic therapy and improves survival in DLBCL.[8, 9] There have been no randomized studies evaluating the role of consolidation RT when rituximab is also administered. In a phase II SWOG study, patients with aggressive non-Hodgkin lymphoma with at least one adverse risk factor were treated with 3 cycles of R-CHOP plus involved-field RT.[19] Progression-free survival was excellent (88% at 4 years). A matched population from the previous SWOG study of 3 cycles of CHOP plus involved-field RT had a progression-free survival of 78%, suggesting superiority of R-CHOP plus consolidation RT. Whether the addition of rituximab increases the absolute benefit of RT (by decreasing the risk of systemic failure) or decreases the absolute benefit of RT (by decreasing the risk of local failure) is unknown, given the lack of randomized trials.
A retrospective study from M.D. Anderson evaluated 469 patients with both localized and advanced disease who were treated with a rituximab-containing chemotherapy regimen (R-CHOP in 70%).[20] Consolidation RT was used at the discretion of the treating physicians. On multivariate analysis, consolidation RT improved both progression-free and overall survival. This benefit was observed for both localized and advanced disease and for bulky and non-bulky presentations.
Positron Emission Tomography (PET)
Functional imaging,18-fluorine fluorodeoxyglucose PET in particular, is now commonly used before, during, and/or after chemotherapy to stage and assess response. How to incorporate PET-assessed response into the treatment algorithm of DLBCL is unclear. Furthermore, interpretation of PET is subjective, with significant inter- and intra-observer variability. One should exercise caution when changing a planned treatment protocol because of an unexpected finding on PET.
With these caveats, a complete response as assessed by PET represents a good systemic response to chemotherapy- but it does not necessarily mean all cancer has been eradicated. Indeed, a negative PET response probably represents 1 to 2 logs of additional cell kill beyond a complete response as assessed by CT. A negative PET response is often mistakenly interpreted to mean that consolidation RT is unnecessary. On the contrary, if chemotherapy has more effectively eradicated systemic disease, the potential benefit of further local therapy increases (until systemic therapy is so effective that both microscopic systemic disease and macroscopic local disease are completely eradicated and relapse rates approach 0%-a situation that has not yet been realized).
Numerous studies have shown that an incomplete response as assessed by PET is associated with an increased risk of failure, particularly in the setting of chemotherapy alone,[21-23] but also with combined modality regimens.[24] Treatment escalation is often necessary, either with salvage chemotherapy with autologous stem cell transplantation or with full-dose RT (discussed later), depending on the individual circumstances. It is usually advisable to repeat a biopsy before escalating therapy, particularly with a stem cell transplant, given the subjective nature of PET interpretation.
Summary and Recommendations: Stage I-II DLBCL
Until further studies have been completed, we recommend consolidation RT, typically 30 Gy, in most patients with localized DLBCL who achieve a complete response, as assessed by PET, to R-CHOP or similar regimens. Involved-field RT, up to 30 Gy, for DLBCL is generally well tolerated with a relatively low risk of late toxicity, including secondary malignancies.[25, 26] Improved technology, such as intensity-modulated RT, can be particularly helpful in avoiding critical structures and minimizing late morbidity (eg, the parotid gland can be spared when treating cervical lymph nodes).
Stage III-IV Disease
TABLE 3

Randomized Trials Evaluating Consolidation RT in Advanced DLBCL
Patients presenting with stage III or IV DLBCL are at higher risk for treatment failure than patients presenting with more localized disease. Various strategies have been employed to improve outcomes in patients with later stage disease, including more intense chemotherapy[27] and high-dose chemotherapy followed by autologous stem cell transplantation.[28] However, the biggest advance to date has been the addition of rituximab to CHOP chemotherapy.[8] An approach that has not been widely studied is the addition of consolidation RT.
Two randomized trials, both performed by the same group in Mexico, evaluated the addition of RT in patients with stage IV DLBCL who presented with bulky disease (defined as larger than 10 cm). The chemotherapy schedule differed somewhat between the two studies, but rituximab was not included in either. Patients were randomly assigned to observation or RT (~40 Gy) to sites of bulky disease. In both studies, the addition of RT improved both progression-free and overall survival in patients who achieved a complete response after CHOP-like chemotherapy (Table 3).[29,30] PET imaging was not part of either study.
A retrospective study from Italy evaluated 94 patients with advanced DLBCL presenting with bulky (larger than 10 cm) or semibulky (larger than 6 cm) disease.[31] Patients were treated with anthracycline-based chemotherapy regimens. The addition of RT decreased the risk of relapse and significantly improved overall survival (73% vs 57%, P = .05) for bulky disease. There was a non-significant trend for improved overall survival in semibulky disease (59% vs 41%, P = .09). A study from M.D. Anderson also demonstrated improvement in freedom from progression (85% vs 51%, P= .003) in patients with advanced disease who received consolidation RT (~40 Gy) to sites of bulky disease ( larger than 4 cm) after CHOP-like chemotherapy.[32]
We have also reviewed our experience at Duke University, specifically evaluating patients who achieved a complete response as assessed by PET or gallium scanning. Among 56 patients who achieved a complete response to anthracycline-based chemotherapy (R-CHOP in 63%), RT was associated with a trend towards improved in-field control (91% vs 71%, P = .07), progression-free survival (83% vs 68%, P = .06), and overall survival (82% vs 64%, P = .1). Although none of the differences reached statistical significance, the number of patients was small.[33]
Summary and Recommendations: Stage III-IV DLBCL
The role of consolidation RT in advanced DLBCL is not established. In select patients, particularly those who present with large-volume disease and who respond favorably to chemotherapy, consolidation RT should be considered. We recommend a slightly lower dose (~18-20 Gy) compared with that used for localized presentations for several reasons. Patients will have generally received more cycles of chemotherapy, thereby necessitating less RT. Treatment volumes are often larger, with more normal tissue in the field, and this also requires a lower total dose of RT. Finally, keep in mind that an appropriate response to systemic therapy is absolutely necessary for RT to provide benefit in advanced DLBCL; this is not the case with localized disease, in which RT can potentially make up for an incomplete response to chemotherapy.
RT After a Partial Response to Chemotherapy
The randomized trials mentioned previously all used CT imaging to assess response to chemotherapy. Functional imaging, PET in particular, has largely supplanted CT as the preferred modality for evaluating treatment response in DLBCL,[34] because of its ability to better distinguish viable tumor from necrosis or fibrosis within residual masses in the post-treatment setting. Numerous studies have shown that an incomplete response as assessed by PET is associated with an increased risk of treatment failure, particularly in the setting of chemotherapy alone[21-23] but also with combined modality regimens[24], with virtually all failures occurring within residual FDG-avid sites.
How best to proceed in patients who do not achieve a complete response as assessed by PET imaging is not clear. The risk of relapse is generally felt to be high enough that observation is not sufficient. The primary options include salvage chemotherapy followed by autologous stem cell transplant or RT. We studied 99 patients with DLBCL (79% stage I-II, 21% stage III-IV) who underwent post-chemotherapy functional imaging (80% PET, 20% gallium).[24] A post-chemotherapy scan was positive in 21 patients.[24] All patients completed consolidation RT without stem cell transplant. In the PET-negative patients, 5-year in-field control (95%), event-free survival (83%), and overall survival (89%) were excellent and significantly better than those in the patients with residual PET-positive disease after chemotherapy. However, with the addition of RT, outcomes in the PET-positive group were good, with 5-year in-field control of 71%, event-free survival of 65%, and overall survival of 73%. Thus, while a positive PET/gallium scan after chemotherapy was associated with an increased risk of local failure and death, RT still resulted in long-term event-free survival in 65% of patients. Further studies are needed to clarify this issue. In the meantime, for patients who achieve a good, but not complete response as assessed by PET, RT is a reasonable strategy. In general, a higher dose of RT is recommended (~40 Gy).
RT with Stem Cell Transplant
TABLE 4

Select Series Evaluating Consolidation RT After Autotransplantation for DLBCL
With current treatment regimens, the majority of patients with DLBCL are cured with initial therapy. Patients with relapsed-and especially primary refractory-disease can pose a therapeutic challenge. The current standard of care is autologous stem cell transplant in patients who respond to salvage chemotherapy.[35] The role of RT in this setting of stem cell transplant is unclear, primarily because there are no randomized studies to provide guidance. The rationale for RT lies in the observation that the majority of treatment failures after transplant (60% to 80%) occur at originally involved sites,[36-38] especially sites of bulky disease.[39,40] Furthermore, the previously cited randomized studies evaluating consolidation RT in the upfront setting demonstrate improved disease control with RT, which provides a rationale for incorporating RT in the treatment of a patient population at particularly high risk for disease recurrence.
Although the literature is not consistent, most retrospective studies have shown that the addition of consolidation RT before or after stem cell transplant improves local control and often progression-free and overall survival (Table 4). The optimal RT volume, dose, and timing of RT (pre- or post-transplantation) must be customized based on the clinical scenario, including history of prior RT, status of disease before transplant, comorbid conditions, and whether or not total body irradiation is planned. For the typical patient who has not received prior RT, 20 to 30 Gy would be appropriate, depending on sites of involvement, volumes to be irradiated, and the patient’s overall condition. Pre-transplant consolidation RT would generally be preferable to avoid radiation of infused stem cells if larger volumes are necessary.
RT For Palliation
For patients with advanced DLBCL, even when the disease has become refractory to standard chemotherapeutics, RT is effective for palliation. A typical prescription would be 20 to 30 Gy, which often provides relatively rapid symptomatic relief with minimal side effects, depending upon the site treated. Alternatively, very low-dose RT (2 Gy × 2), which is frequently used for follicular lymphoma, has also been successful for high-grade lymphomas, including DLBCL. Response rates of 50% to 80% have been reported with 2 Gy × 2, with a median time to progression of approximately 1 year.[41, 42] While these results are somewhat inferior to those seen with follicular lymphoma, for select patients with DLBCL, this regimen may be considered.
Conclusion
RT continues to have an important role in the management of DLBCL. The majority of the randomized trials have shown that consolidation RT decreases the risk of recurrence and improves progression-free survival in patients with localized DLBCL. Although there are fewer prospective trials evaluating the role of RT in advanced DLBCL, both randomized and retrospective studies suggest improved disease control in patients presenting with large-volume disease. Consolidation RT should also be considered in select patients with relapsed or refractory disease who proceed with autologous stem cell transplantation. The effectiveness of RT in the palliative setting is sometimes overlooked; however, RT can provide excellent palliation for patients whose disease becomes refractory to other modalities.
Financial Disclosure:The authors have no significant financial interest or other relationship with the manufacturers of any products or providers of any service mentioned in this article.
References:
References
1. Armitage JO, Weisenburger DD. New approach to classifying non-Hodgkin’s lymphomas: clinical features of the major histologic subtypes. Non-Hodgkin’s Lymphoma Classification Project. J Clin Oncol. 1998;16:2780-95.
2. Hans CP, Weisenburger DD, Greiner TC, et al. Confirmation of the molecular classification of diffuse large B-cell lymphoma by immunohistochemistry using a tissue microarray. Blood. 2004;103:275-82.
3. Lenz G, Wright G, Dave SS, et al. Stromal gene signatures in large-B-cell lymphomas. N Engl J Med. 2008;359:2313-23.
4. Yahalom J, Varsos G, Fuks Z, et al. Adjuvant cyclophosphamide, doxorubicin, vincristine, and prednisone chemotherapy after radiation therapy in stage I low-grade and intermediate-grade non-Hodgkin lymphoma. Results of a prospective randomized study. Cancer. 1993;71:2342-50.
5. Landberg TG, Hakansson LG, Moller TR, et al. CVP-remission-maintenance in stage I or II non-Hodgkin’s lymphomas: preliminary results of a randomized study. Cancer. 1979;44:831-8.
6. Monfardini S, Banfi A, Bonadonna G, et al. Improved five year survival after combined radiotherapy-chemotherapy for stage I-II non-Hodgkin’s lymphoma. Intl J Rad Oncol Biol Phys. 1980;6:125-34.
7. Nissen NI, Ersboll J, Hansen HS, et al. A randomized study of radiotherapy versus radiotherapy plus chemotherapy in stage I-II non-Hodgkin’s lymphomas. Cancer. 1983;52:1-7.
8. Feugier P, Van Hoof A, Sebban C, et al. Long-term results of the R-CHOP study in the treatment of elderly patients with diffuse large B-cell lymphoma: a study by the Groupe d’Etude des Lymphomes de l’Adulte. J Clin Oncol. 2005;23:4117-26.
9. Habermann TM, Weller EA, Morrison VA, et al. Rituximab-CHOP versus CHOP alone or with maintenance rituximab in older patients with diffuse large B-cell lymphoma. J Clin Oncol. 2006;24:3121-7.
10. Kaminski MS, Coleman CN, Colby TV, et al. Factors predicting survival in adults with stage I and II large-cell lymphoma treated with primary radiation therapy. Ann Int Med. 1986;104:747-56.
11. Vaughan Hudson B, Vaughan Hudson G, MacLennan KA, et al. Clinical stage 1 non-Hodgkin’s lymphoma: long-term follow-up of patients treated by the British National Lymphoma Investigation with radiotherapy alone as initial therapy. Br J Cancer. 1994;69:1088-93.
12. Chen MG, Prosnitz LR, Gonzalez-Serva A, Fischer DB. Results of radiotherapy in control of stage I and II non-Hodgkin’s lymphoma. Cancer. 1979;43:1245-54.
13. Horning SJ, Weller E, Kim K, et al. Chemotherapy with or without radiotherapy in limited-stage diffuse aggressive non-Hodgkin’s lymphoma: Eastern Cooperative Oncology Group study 1484. J Clin Oncol. 2004;22:3032-8.
14. Bonnet C, Fillet G, Mounier N, et al. CHOP alone compared with CHOP plus radiotherapy for localized aggressive lymphoma in elderly patients: a study by the Groupe d’Etude des Lymphomes de l’Adulte. J Clin Oncol. 2007;25:787-92.
15. Miller TP, Dahlberg S, Cassady JR, et al. Chemotherapy alone compared with chemotherapy plus radiotherapy for localized intermediate- and high-grade non-Hodgkin’s lymphoma. N Engl J Med. 1998;339:21-6.
16. Miller TP, LeBlanc M, Spier C. CHOP alone compared to CHOP plus radiotherapy for early stage aggressive non-Hodgkin’s lymphomas: Update of the Southwest Oncology Group (SWOG) randomized trial. Blood. 2001;98:724a.
17. Reyes F, Lepage E, Ganem G, et al. ACVBP versus CHOP plus radiotherapy for localized aggressive lymphoma. N Engl J Med. 2005;352:1197-205.
18. Martinelli G, Gigli F, Calabrese L, et al. Early stage gastric diffuse large B-cell lymphomas: results of a randomized trial comparing chemotherapy alone versus chemotherapy + involved field radiotherapy. (IELSG 4). [corrected]. Leukem Lymphoma. 2009;50:925-31.
19. Persky DO, Unger JM, Spier CM, et al. Phase II study of rituximab plus three cycles of CHOP and involved-field radiotherapy for patients with limited-stage aggressive B-cell lymphoma: Southwest Oncology Group study 0014. J Clin Oncol. 2008;26:2258-63.
20. Phan J, Mazloom A, Medeiros J, et al. Benefit of consolidative radiation therapy in patients with diffuse large B-cell lymphoma treated with R-CHOP chemotherapy. J Clin Oncol. 2010;28:4170-6.
21. Juweid ME, Cheson BD. Role of positron emission tomography in lymphoma. J Clin Oncol. 2005;23:4577-80.
22. Mikhaeel NG, Hutchings M, Fields PA, et al. FDG-PET after two to three cycles of chemotherapy predicts progression-free and overall survival in high-grade non-Hodgkin lymphoma. Ann Oncol. 2005;16:1514-23.
23. Spaepen K, Stroobants S, Dupont P, et al. Prognostic value of positron emission tomography (PET) with fluorine-18 fluorodeoxyglucose ([18F]FDG) after first-line chemotherapy in non-Hodgkin’s lymphoma: is [18F]FDG-PET a valid alternative to conventional diagnostic methods? J Clin Oncol. 2001;19:414-9.
24. Dorth J, Chino J, Prosnitz L, Kelsey C. Positive PET prior to consolidative radiation therapy increases risk of in-field failure in diffuse large B-cell lymphoma. Proceedings of ASTRO; IJROBP. 2009;75:S64.
25. Lavey RS, Eby NL, Prosnitz LR. Impact on second malignancy risk of the combined use of radiation and chemotherapy for lymphomas. Cancer. 1990;66:80-8.
26. Okines A, Thomson CS, Radstone CR, et al. Second primary malignancies after treatment for malignant lymphoma. Br J Cancer. 2005;93:418-24.
27. Fisher RI, Gaynor ER, Dahlberg S, et al. Comparison of a standard regimen (CHOP) with three intensive chemotherapy regimens for advanced non-Hodgkin’s lymphoma. N Engl J Med. 1993;328:1002-6.
28. Gianni AM, Bregni M, Siena S, et al. High-dose chemotherapy and autologous bone marrow transplantation compared with MACOP-B in aggressive B-cell lymphoma. N Engl J Med. 1997;336:1290-7.
29. Aviles A, Delgado S, Nambo MJ, et al. Adjuvant radiotherapy to sites of previous bulky disease in patients stage IV diffuse large cell lymphoma. Intl J Rad Oncol Biol Phys. 1994;30:799-803.
30. Aviles A, Fernandezb R, Perez F, et al. Adjuvant radiotherapy in stage IV diffuse large cell lymphoma improves outcome. Leukem Lymphoma. 2004;45:1385-9.
31. Ferreri AJ, Dell’Oro S, Reni M, et al. Consolidation radiotherapy to bulky or semibulky lesions in the management of stage III-IV diffuse large B cell lymphomas. Oncol. 2000;58:219-26.
32. Schlembach PJ, Wilder RB, Tucker SL, et al. Impact of involved field radiotherapy after CHOP-based chemotherapy on stage III-IV, intermediate grade and large-cell immunoblastic lymphomas. Intl J Rad Oncol Biol Phys. 2000;48:1107-10.
33. Dorth JA, Broadwater G, Prosnitz LR, Kelsey CR. Impact of consolidative radiation therapy in stage III-IV diffuse large B-cell lymphoma. Intl J Rad Oncol Biol Phys (Proceedings of ASTRO). 2010;78:S552.
34. Juweid ME, Stroobants S, Hoekstra OS, et al. Use of positron emission tomography for response assessment of lymphoma: consensus of the Imaging Subcommittee of International Harmonization Project in Lymphoma. J Clin Oncol. 2007;25:571-8.
35. Philip T, Guglielmi C, Hagenbeek A, et al. Autologous bone marrow transplantation as compared with salvage chemotherapy in relapses of chemotherapy-sensitive non-Hodgkin’s lymphoma. N Engl J Med. 1995;333:1540-5.
36. Biswas T, Dhakal S, Chen R, et al. Involved field radiation after autologous stem cell transplant for diffuse large B-cell lymphoma in the rituximab era. Intl J Rad Oncol Biol Phys.77:79-85.
37. Hoppe BS, Moskowitz CH, Zhang Z, et al. The role of FDG-PET imaging and involved field radiotherapy in relapsed or refractory diffuse large B-cell lymphoma. Bone Marrow Transplant. 2009;43:941-8.
38. Mundt AJ, Williams SF, Hallahan D. High dose chemotherapy and stem cell rescue for aggressive non-Hodgkin’s lymphoma: pattern of failure and implications for involved-field radiotherapy. Intl J Rad Oncol Biol Phys. 1997;39:617-25.
39. Rapoport AP, Lifton R, Constine LS, et al. Autotransplantation for relapsed or refractory non-Hodgkin’s lymphoma (NHL): long-term follow-up and analysis of prognostic factors. Bone Marrow Transplant. 1997;19:883-90.
40. Oehler-Janne C, Taverna C, Stanek N, et al. Consolidative involved field radiotherapy after high dose chemotherapy and autologous stem cell transplantation for non-Hodgkin’s lymphoma: a case-control study. Hematol Oncol. 2008;26:82-90.
41. Haas RL, Poortmans P, de Jong D, et al. Effective palliation by low dose local radiotherapy for recurrent and/or chemotherapy refractory non-follicular lymphoma patients. Eur J Cancer. 2005;41:1724-30.
42. Murthy V, Thomas K, Foo K, et al. Efficacy of palliative low-dose involved-field radiation therapy in advanced lymphoma: a phase II study. Clin Lymphoma Myeloma. 2008;8:241-5.
43. Vose JM, Zhang MJ, Rowlings PA, et al. Autologous transplantation for diffuse aggressive non-Hodgkin’s lymphoma in patients never achieving remission: a report from the Autologous Blood and Marrow Transplant Registry. J Clin Oncol. 2001;19:406-13.
44. Friedberg JW, Neuberg D, Monson E, et al. The impact of external beam radiation therapy prior to autologous bone marrow transplantation in patients with non-Hodgkin’s lymphoma. Biol Blood Marrow Transplant. 2001;7:446-53.
45. Wendland MM, Smith DC, Boucher KM, et al. The impact of involved field radiation therapy in the treatment of relapsed or refractory non-Hodgkin lymphoma with high-dose chemotherapy followed by hematopoietic progenitor cell transplant. Am J Clin Oncol. 2007;30:156-62.
46. Kewalramani T, Zelenetz AD, Hedrick EE, et al. High-dose chemoradiotherapy and autologous stem cell transplantation for patients with primary refractory aggressive non-Hodgkin lymphoma: an intention-to-treat analysis. Blood. 2000;96:2399-404.
Navigating AE Management for Cellular Therapy Across Hematologic Cancers
A panel of clinical pharmacists discussed strategies for mitigating toxicities across different multiple myeloma, lymphoma, and leukemia populations.