Unanswered Questions: Monoclonal Antibodies in the Treatment of Advanced Non–Small-Cell Lung Cancer
Despite the fact that bevacizumab and cetuximab are both in an advanced stage of clinical development for use in treatment for unresectable NSCLC (with bevacizumab already licensed for the use in clinical practice), several unanswered questions regarding these drugs remain. A number of ongoing trials have been specifically addressed to answer them, however, the first priority should be to personalize treatment, through clinical or biological markers, in order to better select patients who could benefit from targeted therapy with decreased toxicity.
First-line platinum-based doublets is established as the standard of care for advanced non–small-cell lung cancer (NSCLC). Nevertheless, in this field a plateau of effectiveness has been reached during the last years. One new area of exploration in NSCLC therapeutics lies in the use of tyrosine-kinase inhibitors (TKIs) or monoclonal antibodies (mAbs) to target vascular endothelial growth factor (VEGF) and its receptors, and epidermal growth factor receptor (EGFR). The results of randomized trials testing mAbs against VEGF (bevacizumab) and EGFR (cetuximab) are challenging the paradigm of the platinum doublets as the gold standard in advanced NSCLC. Despite the interesting results that have thus far been collected, the benefit of these new agents, both in terms of balancing between advantages and toxicity and the associated health economic burden, is modest. Here we discuss the use of bevacizumab and cetuximab, the mAbs for which the largest amount of data in the treatment of advanced NSCLC exists. However, despite our having a significant amount of data on these two mAbs, we still have much to learn: Which patients are appropriate for these treatments; for how long are the treatments beneficial, and what are the molecular and clinical predictors? We must continue to study these important problems in treating NSCLC.
Introduction
The treatment of advanced non–small-cell lung cancer (NSCLC), including squamous cell carcinoma, adenocarcinoma, and large cell carcinoma has reached a plateau of effectiveness with platinum-based doublets, which today are considered the standard of care.[1-3] However, the development of targeted therapies-in particular against the vascular endothelial growth factor (VEGF) and its receptors and the epidermal growth factor receptor (EGFR)-seems likely to improve overall outcomes of advanced NSCLC. In particular, tyrosine-kinase inhibitors (TKIs) and monoclonal antibodies (mAbs) can both be used to block these molecular targets. Bevacizumab (directed against VEGF), and cetuximab (against EGFR) are the mAbs which have the largest amount of available data for study. However to date, only bevacizumab has been licensed (in combination with chemotherapy) for first-line treatment of advanced NSCLC. Many questions remain concerning the benefits of these new agents in terms of maintaining a balance between advantages and toxicity and the associated health economic burden. Notwithstanding, many unsolved questions still exist regarding patient selection, the length of benefit, and molecular and clinical predictors. In this review we will address some of these issues.
Bevacizumab
Bevacizumab is an anti-VEGF recombinant humanized mAb. Thus far, two randomized phase III trials have compared the combination of bevacizumab with chemotherapy versus chemotherapy alone in the treatment of advanced non-squamous NSCLC.[4-6] In both trials, enrollment was limited to non-squamous histology patients because of the elevated risk of bleeding for squamous lung cancer shown in a previous phase II randomized study. Also those patients with brain metastases were excluded due to the potential risk of bleeding.[7]
In the Eastern Cooperative Oncology Group (ECOG - E4599) study, 878 patients were randomized to either receive paclitaxel and carboplatin plus bevacizumab (15 mg/kg), or the same chemotherapy regimen plus placebo. Patients receiving bevacizumab reported a statistically significant advantage in overall survival (OS of 12.3 versus 10.3 months; P = .003), progression-free survival (PFS of 6.2 versus 4.5 months; P < .001) and objective response rate (ORR of 35% versus 15%; P < .001). Rates of clinically significant bleeding were 4.4% and 0.7% (P < .001), respectively. There were 15 treatment-related deaths in the bevacizumab group, including five from pulmonary hemorrhage.[4] In the AVAiL (AVAstin in Lung) trial, the chemotherapy regimen included cisplatin plus gemcitabine, recycled every three weeks.[5,6] In this trial, chemotherapy plus placebo was compared with chemotherapy plus two different doses of bevacizumab; 7.5 and 15 mg/kg. A total of 1,043 patients with non-squamous NSCLC were randomized to the three arms. Median PFS, the main endpoint of the trial, was significantly prolonged with the bevacizumab administration, the hazard ratios (HRs) were 0.75 (6.7 versus 6.1 months for placebo; P = .003) in the low-dose group and 0.82 (6.5 versus 6.1 months for placebo; P = .03) in the high-dose group compared with placebo. ORRs were 20.1%, 34.1%, and 30.4% for placebo, low-dose bevacizumab, and high-dose bevacizumab plus chemotherapy, with a response duration of 4.7, 6.1, and 6.1 months, respectively. Median OS was 13.1 months for chemotherapy alone, 13.6 months for bevacizumab at 7.5 mg/kg plus chemotherapy (HR versus placebo 0.93, 95% CI 0.78–1.11) and 13.4 months for bevacizumab at 15 mg/kg plus chemotherapy (HR versus placebo 1.03, 95% CI 0.86–1.23). Incidence of grade > 3 adverse events was similar across arms. Grade > 3 pulmonary hemorrhage rates were < 1.5% for all arms despite the fact that 9% of patients received therapeutic anticoagulation.
Both studies reached their primary endpoint (Table 1), however only the E4599 study showed a clinically relevant influence on PFS and OS. Based on these data, several questions were raised:
Should squamous histology and brain metastases really be excluded from bevacizumab therapy?
TABLE 1
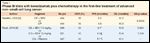
Phase III trials with bevacizumab plus chemotherapy in the first-line treatment of advanced non–small-cell lung cancer
Due to safety concerns, bevacizumab use is restricted to a selected category of patients which may limit its indication to < 30% of all NSCLC patients.[4-7]. Thus, there is interest in determining if patients with brain metastases and with squamous histology can be, at least partially, re-candidated to this effective targeted therapy. The risks related to these two conditions, although not negligible, are not completely known. It is currently unclear whether histology alone or the central localization of the tumor are the risk factors for bleeding. A retrospective evaluation of the clinical and radiographic risk factors associated with severe pulmonary hemorrhage in first-line advanced NSCLC patients treated with carboplatin plus paclitaxel plus bevacizumab reported only the baseline tumor cavitations as a potential risk factor, and not the influence of squamous histology and tumor central localization.[8] In a prospective phase II study, 44 patients with squamous cell histology were treated with two cycles of carboplatin plus paclitaxel regimen and then received carboplatin plus paclitaxel and bevacizumab for an additional four cycles. A total of 27 patients received at least one dose of bevacizumab with an acceptable observed rate of severe pulmonary hemorrhage (1 in 27 patients, or 3.7%).[9] Furthermore, a phase II study in patients with squamous histology completed the accrual; results are pending.
With regard to brain metastases, several data strongly suggest the safety of bevacizumab in advanced NSCLC patients with treated metastases to the brain.[10] Moreover, further safety data showed that the risk of bleeding in patients with untreated brain metastases is similar for patients who receive bevacizumab and for those who do not, across various tumor types. As a consequence, the European Medicines Agency (EMEA) has removed the contraindication concerning the use of bevacizumab in untreated central nervous system (CNS) metastases.[11] Finally, the Food and Drug Administration (FDA) has indicated bevacizumab, in combination with carboplatin and paclitaxel, in advanced non-squamous NSCLC regardless of the presence of brain metastases.[12] However, the last updated American Society of Clinical Oncology (ASCO) guidelines continue to advise against the use of bevacizumab in patients with brain metastases.[13]
To conclude, bevacizumab can be administered in the presence of brain metastases, however further prospective data is needed before we can truly assess its use in non-squamous histology. Next we will turn our attention to tumor cavitations, regardless of histology.
Which bevacizumab dose do we have to use?
As we discussed earlier, the doses of bevacizumab used within the two phase III randomized trials were 7.5 and 15 mg/kg. However, a clinically relevant impact on PFS and OS was shown only in the E4599 study, which used the higher dose of bevacizumab. Nevertheless, when these doses were investigated within a larger phase III randomized trial (the AVAiL study) no differences were reported between the three arms but the lower bevacizumab dose proved to be more powerful across all efficacy endpoints, when combined with cisplatin and gemcitabine.[6] A single-arm, multicenter, international trial evaluated the safety and efficacy of first-line bevacizumab in combination with a range of chemotherapy regimens in over 2,000 patients. Both bevacizumab doses (7.5 and 15 mg/kg) were used. This trial confirmed, in a real-life population, that bevacizumab-based therapy has a well-established and manageable safety profile, reporting efficacy results that were consistent with those seen in the pivotal randomized phase III trials.[14] A preclinical study showed that some chemotherapy drugs, e.g., paclitaxel, can rapidly induce proangiogenic bone marrow-derived circulating endothelial progenitor (CEP) mobilization and subsequent tumor homing, whereas others, e.g. gemcitabine, do not. In other words, paclitaxel exhibited enhanced antitumor effects, while gemcitabine did not. These data indicated that bevacizumab works synergistically with paclitaxel, but not with gemcitabine,[15] and may also explain the absence of improved OS by the addition of bevacizumab in the AVAiL trial. Furthermore, based on these considerations, the last updated ASCO guidelines recommended bevacizumab only at the dose of 15 mg/kg and only in combination with carboplatin and paclitaxel for first-line treatment of selected, advanced, non-squamous NSCLC patients.[13] A recent meta-analysis, including four randomized trials which together totaled 2,101 patients, reported that low-dose bevacizumab may significantly improve PFS in patients with unresectable NSCLC, whereas high-dose bevacizumab may increase two-year overall survival rates, prolong PFS, and improve ORR but at the cost of higher treatment-related death.[16]
Overall, to date, no specific chemotherapy or bevacizumab dose is agreed upon globally. An ongoing prospective randomized phase II biomarker trial is currently evaluating the optimal dose of bevacizumab for use in combination with carboplatin/paclitaxel or cisplatin/gemcitabine.
How long should patients be treated with bevacizumab?
No data are available concerning the optimal duration of the administration of Bevacizumab. At the end of the standard six cycles of chemotherapy plus the targeted agents, non-progressing patients currently continue to receive only the biologic agents until disease progression occurs or there is unacceptable toxicity. This means that several patients entered a sort of ‘maintenance phase’ during these trials. Unfortunately, none of the studies were designed to evaluate the impact of this maintenance phase on outcomes and, in the trials that showed positive results, it is not possible to determine if the benefit was also derived from the maintenance therapy period.
Overall, we believe that in advanced-stage NSCLC patients, bevacizumab should be administered until the disease progresses or until unacceptable toxicity occurs.
Is bevacizumab suitable for elderly patients?
Retrospective analyses evaluating the role of bevacizumab in the elderly population have been performed. In the E4599 trial, 224 (26%) of 850 eligible patients were > 70 years of age (1.6% were > 80 years). For elderly patients, there was a trend towards superior ORR (29% versus 17%; P = .067) and median PFS (5.9 versus 4.9 months; P = .063) with chemotherapy plus bevacizumab when compared to chemotherapy alone, although there was no difference in OS (chemotherapy plus bevacizumab = 11.3 months; chemotherapy = 12.1 months; P = 0.4). Grade 3-5 toxicities were reported in 87% of elderly patients treated with chemotherapy plus bevacizumab, compared to 61% with chemotherapy (P < .001); treatment-related death rates were 6.3% versus 1.8%, respectively. When compared to younger patients, the elderly experienced a higher incidence of toxicities with chemotherapy plus bevacizumab. It is probable that increased toxicity with the addition of bevacizumab in patients > 70 years may have contributed to the absence of survival benefit data for chemotherapy plus bevacizumab versus chemotherapy alone.[17] A retrospective analysis in the subpopulation of elderly patients (≥ 65 years) was also performed in the AVAiL study. The efficacy and safety of bevacizumab plus chemotherapy were compared between young and elderly patient populations. 304 out of a total of 1,043 patients were aged > 65 years. Bevacizumab-treated patients ≥ 65 years derived an improvement in PFS compared to placebo (bevacizumab at the dose of 7.5 mg/kg: HR 0.71, P = .023; at the dose of 15 mg/kg: HR 0.84, P = .25). This PFS benefit was similar to that observed in the overall patient population. ORRs were 40%, 29%, and 30% for elderly patients in the arms at doses of 7.5 mg/kg, 15 mg/kg, and placebo. OS was similar in all treatment arms regardless of age, (low-dose bevacizumab, HR 0.84; high-dose, HR 0.88). There were no safety signals of concern in older patients. Grade ≥ 3 toxicities occurred in 84%, 80%, and 80% of older patients treated with low-dose bevacizumab, high-dose and placebo. The incidences of hypertension and febrile neutropenia were similar in young and elderly patients.[18] Moreover, preliminary data from an international, open-label, single-arm, phase IV safety study of bevacizumab indicate that it has a similar safety profile in older and younger patients, and that elderly patients are no more likely to experience common bevacizumab-related toxicities.[19] However, in these last two analyses, the cut-off age was 65 years, which once again raises the question: What is the limit for defining an elderly patient?
TABLE 2

Phase III trials with cetuximab plus chemotherapy in the first-line treatment of advanced non–small-cell lung cancer
Overall, only retrospective data are available for the use of bevacizumab in elderly patients with advanced NSCLC, thus we recommend that in clinical practice, this treatment should be used in carefully selected elderly patients. Furthermore, ongoing prospective evaluation of bevacizumab-based therapy in elderly patients is clearly warranted, as the need for better and more tolerable therapies in this patient group becomes increasingly urgent.
Are there reliable clinical or biological predictive markers for bevacizumab therapy?
Several retrospective analyses of the E4599 trial that evaluated clinical and biological markers have been performed. Of particular interest are the data concerning the histology subgroups, adenocarcinoma patients (n = 602), with a median OS of 14.2 months for the bevacizumab arm versus 10.3 months for the control arm (HR = 0.69; 95% CI 0.58–0.83). For large cell carcinoma (n = 48), median OS was 10 months for bevacizumab and 8.7 months for placebo, while for NSCLC non-other specified (NOS; N = 165), OS was 9.5 and 10 months, respectively.[20] A subset analysis of survival by gender reported that women on the chemotherapy plus bevacizumab arm versus the chemotherapy alone arm appeared not to have an OS advantage (13.3 versus 13.1 months, respectively; P = .87); the advantage was confined exclusively to men (11.7 versus 8.7 months). Furthermore, the addition of bevacizumab resulted in significant improvements in PFS for men (6.3 versus 4.3 months, respectively) but less for women (6.2 versus 5.3 months). The reasons for this disparity remain unclear, but possible explanations include: the use of second- and third-line treatments (EGFR-TKIs, chemotherapy); imbalance in unmeasured baseline prognostic factors (demographic, molecular); statistical chance alone.[21] In the AVAiL trial, no significant differences attributed to gender were observed; this minimized the gender debate raised by the E4599 trial.[5] Nonetheless, this is an important issue that should be clinically addressed.
Administration of bevacizumab is postulated to decrease nitric oxide synthesis and lead to hypertension, which may be a physiological sign that the VEGF pathway is being blocked. Hypertensive patients were compared with non-hypertensive ones with respect to OS and PFS, using blood pressure data and adverse event data separately. Comparing patients with hypertension in the bevacizumab arm with those with hypertension in the placebo group gave an OS HR of 0.60 (95% CI, 0.43-0.81; P = .001) and a PFS HR of 0.54 (95% CI, 0.41-0.73;
P < .0001); comparing those in the arm without hypertension with those without hypertension in placebo group, the OS HR was 0.86 (95% CI, 0.74-1.00; P = .05) and the PFS HR was 0.72 (95% CI, 0.62-0.84; P < .0001). In conclusions, the onset of hypertension during treatment with bevacizumab plus chemotherapy may be associated with improved outcomes.[22]
With regard to biomarkers, VEGF, basic fibroblast growth factor (bFGF), soluble intercellular adhesion molecule-1 (ICAM), and E-selectin were all evaluated prospectively in the plasma of pretreatment patients. In this study, baseline ICAM levels were prognostic for survival and predicted response to chemotherapy with or without bevacizumab. VEGF levels were predictive of response to bevacizumab but not survival.[23]
Overall, to date, no clinical or biological markers predictive of bevacizumab activity in advanced NSCLC are reliable candidates for implementation in clinical practice. However, ongoing trials are now evaluating the above-mentioned markers.
Cetuximab
EGFR is overexpressed in up to 90% of cases of NSCLC, a fact which is the foundation for the basic rational behind the development of cetuximab. Cetuximab is a chimeric (human-murine) mAb directed against the extracellular domain of the EGFR that blocks ligand (TGF-α, EGF) access to the receptor.[24].
In a large phase III trial named FLEX (First-Line ErbituX in lung cancer), 1,125 patients with EGFR-detectable (by immunohistochemistry - IHC), advanced NSCLC were randomized to cisplatin plus vinorelbine, every three weeks with or without cetuximab (400 mg/m² initial dose, then 250 mg/m²/week) as first-line treatment. The median PFS was 4.8 months in both groups (HR 0.943, 95% CI 0.825–1.077; P = .39). The median OS was the main endpoint; the OS was improved in the cetuximab arm (11.3 versus 10.1 months. HR = 0.871; 95% CI 0.762–0.996; P = .044). The main cetuximab-related adverse event was grade 3 acne-like rash in 57 (10%) patients. A survival benefit was seen in all histological subgroups of NSCLC, with median OS of 12 months (9.6–14.8) versus 10.3 months (8.3–12.1), respectively, for patients with adenocarcinomas (n = 413), 10.2 months (8.2–12.0) versus 8.9 months (7.8–9.8), respectively, for those with squamous cell carcinomas (n = 347), and 9 months (6.5–11.5) versus 8.2 months (6.9–10.2), respectively, for patients with other histological subtypes (n = 185; large-cell, adeno-squamous carcinoma and NSCLC NOS) in the chemotherapy plus cetuximab group versus chemotherapy alone group.[25] The FLEX study is the first to demonstrate a survival benefit from the use of a targeted agent in combination with platinum-based chemotherapy across all histological subtypes in first-line treatment of advanced NSCLC.
A multicenter, open-label, phase III study named BMS099, enrolled 676 chemotherapy-nave patients with advanced NSCLC, without restrictions based on histology or EGFR expression. Patients were randomly assigned to cetuximab (400 mg/m² initial dose, then 250 mg/m²/week) plus carboplatin/paclitaxel or carboplatin/paclitaxel alone. The primary endpoint was PFS, assessed by independent radiologic review committee (IRRC). Secondary endpoints included ORR, OS, quality of life (QoL), and safety. Median PFS-IRRC was 4.4 months with cetuximab plus chemotherapy versus 4.24 months with chemotherapy alone (HR = 0.902; 95% CI, 0.761-1.069; P = .236). Median OS was 9.69 versus 8.38 months, respectively (HR = 0.890; 95% CI, 0.754-1.051; P = 0.169). ORR-IRRC was 25.7% with cetuximab plus chemotherapy versus 17.2% with chemotherapy (P = .007). The safety profile of this combination was manageable and consistent with its individual components: QoL did not differ across treatment arms. This trial did not reach the main endpoint-of PFS-IRCC improvement by cetuximab addition to chemotherapy. However, there was significant improvement in ORR-IRRC and the difference in OS favored cetuximab but did not reach statistical significance.[26] Both trials (Table 2), despite being statistically different, reported results that were quite similar: comparable PFS and an absolute survival benefit of about 1.2 months for the cetuximab arm. Several hypotheses formed to explain their different results: that there was an insufficient number of patients enrolled in the BMS099 trial which made it impossible to detect a difference between the two arms; the type of chemotherapy used; and the possible influence of any molecular selection.
Does cetuximab prove efficacy?
To better understand the real impact of cetuximab-based treatment in advanced NSCLC, a meta-analysis of four randomized phase II/III studies involving 2,018 patients (1,003 patients treated with chemotherapy plus cetuximab and 1,015 patients treated with chemotherapy alone) was performed. This meta-analysis demonstrated a significant benefit across all investigated efficacy endpoints for the cetuximab combination over chemotherapy alone, irrespective of which platinum doublet was used and in all histological subtypes of NSCLC: OS (HR = 0.878, 95% CI 0.795–0.969; P = .010), PFS (HR = 0.899, 95% CI 0.814–0.993, P = .036), and ORR (odds ratio = 1.463, 95% CI 1.201–1.783, P< .001).[27] Despite these positive results both the FDA and the EMEA rejected the licensing of cetuximab in combination with chemotherapy for first-line therapy of advanced NSCLC.[28,29] This decision was most likely based on the consideration that the addition of cetuximab to chemotherapy provides a small OS benefit, which should be weighed against its side effects, the fact that it must be administered weekly, and costs. Ongoing randomized trials have the goal of producing further data to reinforce the actual benefit reported by the addition of cetuximab to first-line therapy.
TABLE 3

Randomized phase II trials with cetuximab in the first-line treatment of special patients population affected by advanced non–small-cell lung cancer
Is cetuximab suitable for the “special patients population”?
The “special patients population” includes the elderly and patients with performance status (PS) 2; both of which are generally considered unsuitable for combination chemotherapy. The FLEX trial is the first study that investigates new biologic agents with PS 2 patients enrolled. The subgroup analysis performed in PS 2 patients (92 randomized in the cetuximab arm and 104 in the placebo group) confirmed the benefits in survival reported in the general population (HR 0.74, 95% CI, 0.55-1.01).[25] This topic has also been addressed by prospective studies. In two parallel randomized phase II studies (CALC-1:Cetuximab in Advanced Lung Cancer), 58 advanced NSCLC elderly (age > 70 years), and 42 PS 2 patients were randomized to receive the combination of cetuximab and gemcitabine or gemcitabine followed by cetuximab either as maintenance treatment after six cycles of gemcitabine or as second-line treatment after disease progression during the gemcitabine treatment. No patients were selected for EGFR-expression. The primary endpoint was one-year survival which was, in the elderly, 41.4% and 31% for the combination and sequential treatments, respectively with a PFS of 3 and 4 months and an OS of 6 and 9 months, respectively. ORRs were 10.3% in both arms, with similarly mild toxicity profiles. In PS 2 patients, the one-year survival was 27.3% in the combination arm and 35% in the sequential arm, PFS was 5.7 and 2.2 months and OS was 10.2 and 6.5 months, respectively. ORRs were 9.1% in the combination arm and 10% in the sequential arm. Overall toxicity was similar in the two arms. Although the percentage of patients alive after one year was higher in the combination arm for elderly patients and higher in the sequential arm in PS 2 patients, no striking differences in efficacy were observed in either study. However, using the sequential strategy, 34% of elderly patients and 60% of PS 2 patients were unable to start cetuximab as maintenance or second-line treatment. Our results suggest that combining gemcitabine and cetuximab, from the beginning of treatment, is the optimal way to give all patients the chance to receive cetuximab.[30] A phase II randomized trial, addressed to PS 2 advanced NSCLC patients, tested docetaxel in combination with either cetuximab or bortezomib, a proteasome inhibitor. A total of 64 patients were randomized, reporting an ORR of 13.3% for docetaxel plus cetuximab and 10.3% for docetaxel plus bortezomib; median PFS was 3.4 and 1.9 months, and OS was 5 and 3.9 months, respectively. There was one treatment-related death in each arm. These disappointing results confirm the poor prognosis associated with PS 2 patients. Neither combination produced data to justify further research in this subset of patients.[31] Table 3 summarizes the results of phase II randomized trials employing cetuximab and chemotherapy as first-line treatment for special patients population affected by advanced NSCLC. However, to date, there is still little data available about cetuximab administration in the special patients population, and further prospective studies should evaluate its role in this subset of patients.
Are there reliable clinical or biological markers predictive for subgroups of patients who may benefit from cetuximab therapy, and for whom it could be licensed for clinical practice?
Several molecular and clinical factors have been identified as potential predictors of outcome for treatment with cetuximab. Skin rash, the main side effect related to cetuximab, appears to be a sterile, suppurative form of folliculitis, and usually appears on the face and upper torso; it is generally dose-dependent. The possible relationship between rash and clinical benefit remains unclear, and additional studies are needed to determine the clinical relevance of this observation.[32] In the FLEX trial, 290 patients who had been randomized to chemotherapy plus cetuximab arm and who developed an acne-like rash of any grade within the first three weeks (and were still alive after the first cycle) had a longer OS than the 228 patients without an acne-like rash (14.3 versus 8.1 months).[33] An exploratory post hoc analysis from BMS099 trial was performed to evaluate the correlation between the presence of early rash and OS. Median OS for patients with early acneiform rash (n = 185) was 10.4 months (95% CI, 7.7-12.0 months), compared with 8.9 months (95% CI, 6.8-10.9 months) for the 130 patients without early rash (HR = 0.76; 95% CI, 0.59-0.98).[26] In the CALC-1 trial, patients receiving cetuximab and suffering skin toxicity also seem to have a better survival outcome.[30] Among the nine elderly patients who did not suffer from skin rash, OS was 2.5 months, while in the 20 patients with any grade skin toxicity OS was 13.5 months. Among eight PS 2 patients who had no skin rash, the OS was 6.7 months, while it was 10.7 months in the 14 patients who reported any grade of skin toxicity. Another clinical factor which should be evaluated is the Asian population, which in the FLEX trial reported a worse survival in the cetuximab arm when compared with the chemotherapy arm (OS of 17.6 versus 20.4 months, respectively). These data should be further evaluated considering that there were only 121 Asian patients randomized in the FLEX trial, the rate of EGFR mutations in this population is > 50% and the percentage of patients receiving, as salvage treatment, small molecule inhibiting EGFR was 73% in the chemotherapy-only arm and 50% in the chemotherapy plus cetuximab arm.[25] However, this difference underscores the need to understand population pharmacogenomics.
The roles of EGFR-IHC and EGFR gene copy number (evaluated by fluorescence in situ hybridization - FISH)in selecting patients who may much benefit from cetuximab therapy are not yet totally clear. However, most of these data comes from retrospective analyses of small phase II trials with limited specimens. A retrospective analysis from the FLEX trial evaluated the impact of EGFR mutations on the outcomes of patients treated with cetuximab. Of 293 patients for whom EGFR mutation status could be determined, 49 (17%) were found to have tumors with EGFR kinase domain mutations. OS was longer in patients with EGFR mutated tumors compared with wild type tumors in both treatment groups. These results indicate that benefit from cetuximab in NSCLC is regardless of EGFR mutation status.[34] In the FLEX trial, the K-ras status was evaluated in 395 patients (35% of the entire population) with adequate tumor tissue available. Mutations of K-ras were found in 75 patients (19%). No differences in terms of ORR, PFS and OS were reported between the cetuximab group and the placebo arm. These data showed benefit from cetuximab regardless of K-ras mutation status.[35]
Overall, careful patient selection is crucial to optimize the benefit from cetuximab. To date, rash developed during cetuximab therapy represents the most reliable predictor of its benefit. However, using the rash to select patients to treat with cetuximab presents various difficulties. The predictive value of biological markers, such as EGFR and K-ras status, is still highly controversial.
Conclusions
Despite the fact that bevacizumab and cetuximab are both in an advanced stage of clinical development for use in treatment for unresectable NSCLC (with bevacizumab already licensed for the use in clinical practice), several unanswered questions regarding these drugs remain. A number of ongoing trials have been specifically addressed to answer them, however, the first priority should be to personalize treatment, through clinical or biological markers, in order to better select patients who could benefit from targeted therapy with decreased toxicity.
Financial Disclosure:The author has no significant financial interests or other relationships with the manufacturers of any products or providers of any service mentioned in this article.
References:
References
1. Socinski MA, Crowell R, Hensing TE, et al. Treatment of non–small-cell lung cancer, stage IV – ACCP evidence-based clinical practice guidelines (2nd Edition). Chest. 2007;132:277S-289S.
2. Azzoli CG, Baker S Jr, Temin S, et al. American Society of Clinical Oncology Clinical Practice Guideline update on chemotherapy for stage IV non–small-cell lung cancer. J Clin Oncol. 2009; 27:6251-6266.
3. D’Addario G, Fruh M, Reck M, et al. Metastatic non–small-cell lung cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2010; 21 (suppl. 5):v116-v119.
4. Sandler A, Gray R, Perry MC, et al. Paclitaxel-carboplatin alone or with bevacizumab for non–small-cell lung cancer. N Engl J Med. 2006; 355:2542-2550.
5. Reck M, von Pawel J, Zatloukal P, et al. Phase III trial of cisplatin plus gemcitabine with either placebo or bevacizumab as first-line therapy for nonsquamous non–small-cell lung cancer: AVAil. J Clin Oncol. 2009; 27:1227-1234.
6. Reck M, von Pawel J, Zatloukal P, et al. Overall survival with cisplatin-gemcitabine and bevacizumab or placebo as first-line therapy for nonsquamous non–small-cell lung cancer: results from a randomised phase III trial (AVAiL). Ann Oncol. 2010; 21:1804-1809.
7. Johnson DH, Fehrenbacher L, Novotny WF, et al. Randomized phase II trial comparing bevacizumab plus carboplatin and paclitaxel with carboplatin and paclitaxel alone in previously untreated locally advanced or metastatic non–small-cell lung cancer. J Clin Oncol. 2004; 22:2184-2191.
8. Sandler AB, Schiller JH, Gray R, et al. Retrospective evaluation of the clinical and radiographic risk factors associated with severe pulmonary hemorrhage in first-line advanced, unresectable non–small-cell lung cancer treated with carboplatin and paclitaxel plus bevacizumab. J Clin Oncol. 2009;27:1405-1412.
9. Hainsworth J, Compton P, Strickland D, et al. BRIDGE: An open-label phase II trial evaluating the safety of bevacizumab (BV) + paclitaxel/carboplatin (PC) as 1st-line treatment for patients (pts) with advanced, previously untreated, squamous non–small-cell lung cancer (NSCLC) (Abstract 128). J Thorac Oncol, 2008;3(Suppl.):S281.
10. Socinski MA, Langer CJ, Huang JE, et al. Safety of bevacizumab in patients with non–small-cell lung cancer and brain metastases. J Clin Oncol. 2009;27:5255-5261.
11. Post-authorisation summary of positive opinion for avastin. Available at:
http://www.emea.europa.eu/pdfs/human/opinion/Avastin_12112009en.pdf (accessed on October 23, 2010).
12. Label approved on 07/31/2009 for avastin, BLA no. 125085. Available at:
http://www.accessdata.fda.gov/drugsatfda_docs
label/2009/125085s0168lbl.pdf (accessed on October 23, 2010).
13. Azzoli CG, Baker S Jr, Temin S, et al. American Society of Clinical Oncology clinical practice guideline update on chemotherapy for stage IV non–small-cell lung cancer. J Clin Oncol. 2009;27:6251-6266.
14. Crinò L, Dansin E, Garrido P, et al. Safety and efficacy of first-line bevacizumab-based therapy in advanced non-squamous non–small-cell lung cancer (SAiL, MO19390): a phase 4 study. Lancet Oncol. 2010; 11:733-740.
15. Shaked Y, Henke E, Roodhart JM, et al. Rapid chemotherapy-induced acute endothelial progenitor cell mobilization: implications for antiangiogenic drugs as chemosensitizing agents. Cancer Cell. 2008;14:263-273.
16. Yang K, Wang YJ, Chen XR, et al. Effectiveness and safety of bevacizumab for unresectable non–small-cell lung cancer. A meta-analysis. Clin Drug Investig. 2010; 30:229-241.
17. Ramalingam SS, Dahlberg SE, Langer CJ, et al. Outcomes for elderly, advanced-stage non–small-cell lung cancer patients treated with bevacizumab in combination with carboplatin and paclitaxel: analysis of Eastern Cooperative Oncology Group Trial 4599. J Clin Oncol.2008; 26:60-65.
18. Leighl NB, Zatloukal P, Mezger J, et al. Efficacy and safety of bevacizumab-based therapy in elderly patients with advanced or recurrent nonsquamous non–small-cell lung cancer in the phase III BO17704 study (AVAiL). J Thorac Oncol, 2010; Oct 25 [Epub ahead of print].
19. Griesinger F, Pavlakis N, Garrido P, et al. MO19390 (SAiL): safety and efficacy of first-line bevacizumab plus chemotherapy in elderly patients with advanced or recurrent non-squamous non–small-cell lung cancer (NSCLC) (Abstract C2.6). J Thorac Oncol. 2009; 4 (Suppl 1):S359-S360.
20. Sandler A, Yi J, Dahlberg S, et al. Treatment outcomes by tumor histology in Eastern Cooperative Group Study E4599 of bevacizumab with paclitaxel/carboplatin for advanced non–small-cell lung cancer. J Thorac Oncol. 2010; 5:1416-1423.
21. Brahmer JR, Gray R, Schiller JH, et al. ECOG 4599 phase III trial of carboplatin and paclitaxel + bevacizumab: Subset analysis of survival by gender (Abstract 7036). J Clin Oncol,2006; 24(18S):373s.
22. Dahlberg SE, Sandler AB, Brahmer JR, et al. Clinical course of advanced non–small-cell lung cancer patients experiencing hypertension during treatment with bevacizumab in combination with carboplatin and paclitaxel on ECOG 4599. J Clin Oncol. 2010;28:949-954.
23. Dowlati A, Gray R, Sandler AB, et al. Cell adhesion molecules, vascular endothelial growth factor, and basic fibroblast growth factor in patients with non–small-cell lung cancer treated with chemotherapy with or without bevacizumab - an Eastern Cooperative Oncology Group Study. Clin Cancer Res. 2008; 14:1407-1412.
24. Humblet Y: Cetuximab: an IgG(1) monoclonal antibody for the treatment of epidermal growth factor receptor-expressing tumours. Expert Opin Pharmacother. 2004; 5:1621-1633.
25. Pirker R, Pereira JR, Szczesna A, et al. Cetuximab plus chemotherapy in patients with advanced non–small-cell lung cancer (FLEX): an open-label randomised phase III trial. Lancet 2009; 373:1525-1531.
26. Lynch TJ, Patel T, Dreisbach L, et al. Cetuximab and first-line taxane/carboplatin chemotherapy in advanced non–small-cell lung cancer: results of the randomized multicenter phase III trial BMS099. J Clin Oncol. 2010; 28:911-917.
27. Thatcher N, Lynch TJ, Butts C, et al. Cetuximab plus platinum-based chemotherapy as 1stline treatment in patients with non–small-cell lung cancer (NSCLC): a meta-analysis of randomized phase II/III trials (Abstract A3.7). J Thorac Oncol. 2009; 4 (suppl 1):S297.
28. Label approved on 07/22/2009 for erbitux, BLA no. 125084. Available at: http://www.accessdata.fda.gov/drugsatfda_docs/label/2009/125084s167lbl.pdf (accessed on October 23, 2010).
29. Assessment report for erbitux, procedure no. EMEA/H/C/558/II/0029. Available at: http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Assessment_Report_-_Variation/human/000558/WC500075683.pdf (accessed on October 23, 2010).
30. Gridelli C, Morabito A, Gebbia V, et al. Cetuximab and gemcitabine in elderly or adult PS2 patients with advanced non–small-cell lung cancer: The cetuximab in advanced lung cancer (CALC1-E and CALC1-PS2) randomized phase II trials. Lung Cancer. 2010; 67:86-92.
31. Lilenbaum R, Wang X, Gu L, et al. Randomized phase II trial of docetaxel plus cetuximab or docetaxel plus bortezomib in patients with advanced non–small-cell lung cancer and a performance status of 2: CALGB 30402. J Clin Oncol. 2009; 27:4487-4491.
32. Rossi A, Bria E, Maione P, et al. The role of cetuximab and other epidermal growth factor receptor monoclonal antibodies in the treatment of advanced non–small-cell lung cancer. Rev Recent Clin Trials 2008; 3:217-227.
33. Gatzemeier U, von Pawel J, Vynnchenko I, et al. FLEX: Cetuximab in combination with platinum-based chemotherapy (CT) improves survival versus CT alone in the 1st-line treatment of patients (pts) with advanced non–small-cell lung cancer (NSCLC) (Abstract 8). J Thorac Oncol. 2008; 3 (suppl 4):S265-S266.
34. Gatzemeier U, Paz-Ares L, Rodrigues Pereira J, et al. Molecular and clinical biomarkers of cetuximab efficacy: data from the phase III FLEX study in non–small-cell lung cancer (NSCLC) (Abstract B2.3). J Thorac Oncol. 2009; 4 (suppl. 1):S324.
35. O’Byrne KJ, Bondarenko I, Barrios C, et al. Molecular and clinical predictors of outcome for cetuximab in non–small-cell lung cancer (NSCLC): data from the FLEX study (Abstract 8007). J Clin Oncol. 2009; 27(15S):408s.