Recap: AE Management and QOL Improvement Options in RCC
Chung-Han Lee, MD, PhD, and colleagues discuss the case of a patient with renal cell carcinoma, touching on optimal treatments, toxicities, and other factors.

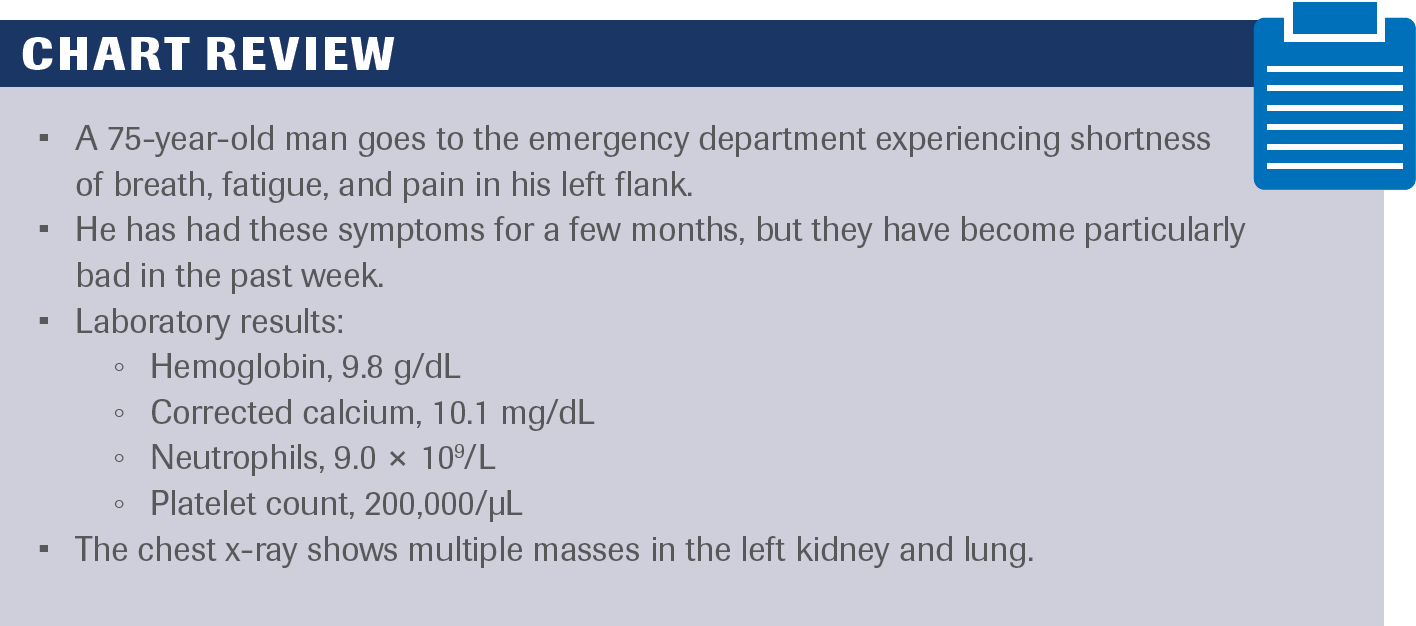
Chart Review.
FOLLOW Chung-Han Lee, MD, PhD, assistant attending physician at Memorial Sloan Kettering Cancer Center, as he conducts Morning Rounds with the treating team of Christine Anderson, FNP-BC, RN, and Patricia Fischer, MSN, RN, OCN.
The discussion begins by reviewing a patient case of a 75-year-old man with a diagnosis of renal cell carcinoma (RCC), for whom Lee navigated adverse effect (AE) management and adjusted dosing to improve his quality of life. Additionally, the team reviews what they are looking forward to treatment-wise in the future.
LEE: How do you typically see RCC presented?
ANDERSON: Just as in this [chart review], pain is the biggest factor. Sometimes this pain has been going on for a while, but then it gets so acute that it brings them to the emergency [department]. Imaging at that time reveals kidney cancer. For the most part, when we see them in the clinic, they also tend to complain of fatigue that has been lingering for a while, or even some weight loss that has been unintentional too. Those tend to be common symptoms.
LEE: What type of imaging would this patient need?
ANDERSON: In this setting, certainly a CT, a CAT scan of the chest, the abdomen, and of the pelvis would be helpful just to get the overall extent of his disease.
LEE: The patient is given lenvatinib [Lenvima] plus pembrolizumab [Keytruda]. About 3 weeks after the patient started treatment, he ends up developing a little bit of hypertension, about grade 1 so far, and then grade 2 diarrhea. These are not uncommon AEs with these types of medications. Then the patient comes into the clinic and says, “I have a family reunion in a few weeks,” and he wants to get a better sense of how he wants to handle some of these AEs. What would you recommend for this patient?
ANDERSON: The diarrhea can [have the most impact] on patients and their quality of life and doing [activities]. Certainly, there are times if maybe there is a specific event coming up we can hold it for a couple of days just to give them a little relief and enjoy their time with family. We could see how the diarrhea improves even while they’re holding the medication. Then at that point, if things get better [and] he’s done with the reunion, we could talk about restarting [therapy] possibly at a lower dose just to see if he tolerates that a little bit better.
LEE: Whenever we talk about these dose holds or modifications, this is always distressing [to] the patients. Trying to educate them in advance about these dose modifications is incredibly important. Whenever we talk about these medications that do have potential AEs, [patients will] know in advance that dose modifications are common.
ANDERSON: Educating them right at the beginning of treatment with the mind-set that this is where we’re starting, the highest dose, but we are able to go down—and everybody tolerates things differently—and just reassuring them is important.
LEE: For these patients, if we’re considering starting a tyrosine kinase inhibitor/immunotherapy (TKI/IO) regimen like lenvatinib plus pembrolizumab, how often will you see them?
ANDERSON: These patients are receiving active treatment, they’re receiving IO about every 3 weeks, so we would certainly see them for their visits before we proceed with any more infusions, to assess their AEs and tolerability. We certainly want to get updated labs before each infusion, while they’re [receiving] the TKIs too, to make sure everything is within range to continue their therapy or in case we need to modify any dosing or anything like that. It certainly is about every 3 weeks, at least a month, [that] we’re seeing them in the clinic to evaluate them.
LEE: If the patient comes to you with some symptoms, what’s your threshold for saying that we should probably think about escalating some of the questions?
ANDERSON: It depends on what it is. We’ve talked about things like diarrhea and blood pressure. Certainly, if blood pressure is a hypertensive crisis, they need to go to an emergency [department]. There are other things that patients with cancer are at risk for. Sometimes whether it’s new onset, shortness of breath, or things like that, we have to rule them out for blood clots or whatnot. We have a symptomatic care clinic that we use or an emergency [department]. Sometimes if [they experience] new pain or [symptoms] like that, it just may prompt us to get imaging a little bit sooner rather than later, but those are the big things.
LEE: What are you excited about in the future of RCC?
ANDERSON: When I started as a newer [nurse practitioner], these multiple combination regimens of the TKIs and the IOs were not so much available. The fact that these combination approaches are now happening on a routine basis and we’re seeing people live longer with this disease is very hopeful for the future of kidney cancer.
LEE: How do you associate specific AEs when deciding on treatment options, because they are key when debating therapies?
FISCHER: When thinking about IO drugs, the goal is to boost the immune system to fight cancer. At the same time, it will boost other systems within the body. That can have AEs of diarrhea, perhaps, elevated liver function test values, sometimes itchy skin with or without a rash, as well as other organs that can be affected throughout the body. Maybe those are some of the more common ones. Including the TKIs, their AE profiles are typically elevating blood pressure. We’d have to be sure to educate [patients] about how to take their blood pressure when using a battery-operated cuff for the arm. I like it when they bring it into the clinic so we can compare it with a reading that we get just to make sure it’s similar and the machine is OK for them to use at home. We’d also have to talk to them about diarrhea and some of the precautions to help maintain regular bowel movements without diarrhea, when to call us, and how to reach us after hours as well as during hours if there’s a concern or a question.
LEE: What are ways that you’ve thought about [for] trying to be proactive and preempting some of these issues that they may experience?
FISCHER: I like to use the fact cards that are available. Some institutions have their own. If not, the Kidney Cancer Association has a website that’s great and is a wealth of information for patients and caregivers. [I recommend starting] with the fact cards so they can have handwritten material. Even though I’m going to go over it in the room with them, it’s important to have something to bring home, and they can use that to take notes on. I also want to give them a calendar to record [dosing schedules], especially if they’re taking a drug by mouth every day or twice a day. I’d like to see them record that on a daily basis. I’m also going to ask them to take their blood pressure at least once a day in the morning, and record on the calendar or the diary that they’ve taken their medication as well as their blood pressure. Parameters [should be discussed] as to when they should call us if they see the blood pressure above a certain number, what that number is, and when to call us and how to call us. Then we’ll see them in the clinic to review these things, but I want them to know that they can call us as well.
LEE: Blood pressure control is a huge issue, especially for this population [in which] the medications are expected to raise people’s blood pressure, and many of our patients are on multiple blood pressure medications already. What advice can you offer to patients here?
FISCHER: Knowing what blood pressure medications they’re currently on with the correct dose and keeping that up to date in their chart [is important]. Also, have a discussion with them about what we might add if there’s a problem. We give them specific numbers [about which] to call us if there’s a concern. If they see this number [for blood pressure, they should] give us a phone call.
LEE: We also want to emphasize to them if they’re symptomatic from their blood pressure, that’s going to be incredibly important that they seek medical attention.
FISCHER: They might think that the headache they’re having is just an ordinary headache or a headache from treatment, but it could be a sign of elevated blood pressure.
LEE: As a nurse who is at the forefront of clinical trials, what have you seen in terms of how the treatments have impacted patients’ lives?
FISCHER: People are living longer with these therapies and finding the right dose for them is so important, as you were just talking about. When we start them, it’s 1 dose for everyone whether you’re 6 ft 4 in or 5 ft 2 in. Everybody tolerates therapies differently, and we want to keep that in mind and support them through their first 2 cycles as best we can to then find the best dose for them to hopefully be able to take the medication continuously without too many interruptions or AEs, because they are on it for months or years.
LEE: How do patients tolerate treatments once you find a dose that is tolerable?
FISCHER: From the beginning, I tell patients we want them to keep doing all the things that they want to do. If that means working full time and taking vacations, then we will support you to do that and that’s part of helping them tolerate the therapy so that they’re not stuck at home with diarrhea or extra visits to the doctor because their blood pressure is too high. And most people are able to keep doing those things.
LEE: Are there any therapies that you’re excited about?
FISCHER: It’s all exciting right now. It’s come a long way. It’s great to have all these therapies to choose from. I think genetics is important, which is sometimes done right at certain centers, [using] genetic profiling [correctly] to better define what therapy each person should get.
