Study Finds Different Treatment Responses Between BRCA2- and BRCA1-Mutated Ovarian Cancers
Women with high-grade serous ovarian cancer who also harbor a BRCA2, but not a BRCA1 mutation tend to have a better chemotherapy response and overall survival compared with those patients who are BRCA wild type.
Women with high-grade serous ovarian cancer who harbor a BRCA2, but not a BRCA1 mutation tend to have a better chemotherapy response and overall survival compared with patients who are BRCA wild-type. The 5-year survival rate of BRCA2-mutation carriers was significantly greater than that of wild-type BRCA2 patients (61% compared with 25%, P = .003). BRCA1 mutation carriers had a 44% 5-year survival rate, not statistically different from survival rates of wild-type BRCA individuals when adjusted for age.
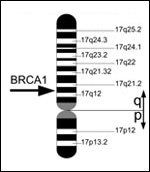
BRCA1
gene located on chromosome 17, Courtesy of Armin Kbelbeck, Wikimedia Commons
In terms of chemotherapy responses, BRCA2 mutant carriers had a significantly higher response to primary chemotherapy as well as a longer platinum-free duration than either BRCA1 or BRCA wild-type individuals.
No differences were found among individuals who had an inactivation of BRCA1 via a genetic mutation in the BRCA1 gene or inactivation of BRCA1 via an epigenetic mechanism. This data is the result of an observational genomics and clinical data analysis of 316 women with high-grade serous ovarian cancer published today in JAMA.[1] All participants were part of the public Cancer Genome Atlas (TCGA) project.
It is not yet clear whether women with ovarian cancer who have a mutation in either of the BRCA genes are more susceptible to treatment with platinum-based chemotherapy and may therefore have a better response and overall survival.
This data conflicts with different studies reporting both favorable and negative outcomes in BRCA1/2 carriers, which have looked at different nationalities including Israeli and Japanese, as well as at both broad and narrow classifications of ovarian cancer. The confounding results may be due to the different types of treatments used around the world and the timing of treatment and detection. Additionally, research is now showing that ovarian cancer may not be one disease but many different subtypes that originated from distinct tissue types. To further confound results, most studies looking at the clinical outcome of BRCA1/2 patients did not have detailed information on the patients’ chemotherapy treatments.
The goal of surveillance of BRCA germline mutations is to detect ovarian cancer early. This is especially important because, currently, very little other detection methods exist for ovarian cancer. Women with a germline mutation in BRCA1 have a 39% to 54% cumulative lifetime risk of developing ovarian cancer, and those with BRCA2 have an 11% to 23% cumulative risk.
The BRCA genes function in homologous recombination and DNA repair, and cells deficient in either BRCA gene have compromised homologous recombination function and accumulation of DNA damage. Because DNA repair is also essential for cancer cells to survive, the rationale is that treating tumor cells with DNA-damaging agents such as chemotherapy will cripple the already genomically-unstable repair-deficient tumor cells. Therefore, patients with the BRCA mutations may have a higher response to and overall survival from platinum-based chemotherapy.
The results
The 316 women with ovarian cancer, who were in the TCGA database that contains detailed clinical and genetic information, were analyzed for overall survival (OS) and progression-free survival (PFS) rates, chemotherapy response (both primary response and platinum-free duration after treatment), and mutation status. 35 women had a BRCA1 mutation (10 somatic, 15 germline), 27 had a BRCA2 mutation (9 somatic, 18 germline), and 219 were wild-type for both. Patients with a BRCA1 mutation were younger at diagnosis, with a mean age of 55.9 years, compared with 61.8 years for wild-type patients (P = .006), or 60.9 years for patients with a BRCA2 mutation (P = .03). The study did not say whether the mutations were missense or nonsense mutations.
Because there were no differences in the OS or the PFS duration between germline carriers and somatic mutant patients, these mutation types were pulled for analysis. In addition to better OS rates, BRCA2 mutation carriers had more 5-year PFS durations than their wild-type BRCA counterparts (39% of the former remained progression free compared with 10% of the latter, P = .004). There was also a significant difference between BRCA2 and BRCA1 individuals; 13% of the latter had a 5-year PFS duration.
100% of BRCA2 mutant carriers were sensitive to an initial adjuvant chemotherapy regimen, compared with 85% of wild-type BRCA individuals. 80% of BRCA1 carriers were adjuvant chemotherapy–sensitive. BRCA2 carriers had a median 18.0-month platinum-free duration compared with 12.5 months in BRCA1-mutant individuals and 11.7 months in wild-type BRCA patients.
Of the 316 ovarian cancer patients, 33 had inactivation of the BRCA1 gene via promoter hypermethylation, while no cases of promoter hypermethylation in the BRCA2 gene were found. BRCA1-hypermethylated individuals were also statistically significantly younger than the wild-type BRCA counterparts, with a mean age of 57.3 at diagnosis. No significant differences between BRCA1 hypermethylated cases and wild-type cases were observed for OS or PFS. These patients did have a statistically significantly shorter PFS duration compared with BRCA2 individuals, suggesting that neither genomic nor epigenetic inactivation is associated with a better prognosis.
The surgical specimens of all of the ovarian cancer patients were sequenced prior to any systemic therapies and sequenced to look for disparities in mutation accumulation. The genomes of ovarian cells from BRCA2 individuals were found to be hypermutated compared with either BRCA1 or BRCA wild-type tumors. The authors found 61 genes that were differentially mutated in BRCA2 tumors compared with wild-type tumors. There were no differentially mutated genes in the genomes of BRCA1 carrier specimens compared with wild-type samples.
In the discussion of their results, the authors point out that there are differences between BRCA1 and BRCA2 carriers. While BRCA1 germline mutations are associated with breast and ovarian cancers, families with BRCA2 germline mutations also have higher frequencies of pancreatic cancer in both males and females, of male breast cancer, and of prostate cancer.
In terms of function, while both BRCAgenes function in DNA repair, they have distinct functions in different pathways. BRCA2 appears to regulate the RAD51 in the homologous recombination pathway of double-stranded break repair. The authors believe that this function may be why a "mutator" phenotype is seen in BRCA2 deficient ovarian tumor cells and why chemotherapy appears to elicit a response for this tumor type. BRCA1 has a broader role in the different pathways that influence DNA repair, including the DNA damage response, mitotic spindle assembly, and cell cycle checkpoint. This broader function of BRCA1 may be why cells deficient in BRCA1 may be predisposed to tumorigenesis but may not necessarily result in the BRCA1 mutated tumors being more susceptible to chemotherapy cross-linking agents.
The results shown in this paper need to be substantiated with a larger patient study cohort and prospective clinical trials. Functional studies are also needed to further delineate the roles of the BRCAgenes in DNA damage repair and cell cycle checkpoint control.
As the authors of the accompanying editorial, Victor R. Grann, MD, and Ramon E. Parsons, MD, PhD, point out, "The discrepancy between the response and survival among BRCA1 and BRCA2 mutation carriers should encourage attention to the differences in treatment between the two groups."
References:
Reference:
1. Yang D et al. JAMA. 2011;306:1557-65.