Study teases out physician intent and preferences for CRC regimen selection
Fluorouracil, oxaliplatin (Eloxatin), and bevacizumab (Avastin) for first-line therapy is preferred in metastatic colon cancer.
Fluorouracil, oxaliplatin (Eloxatin), and bevacizumab (Avastin) for first-line therapy is preferred in metastatic colon cancer. But chemotherapy use can vary depending on patient age and the therapy’s toxicity profile, said researchers from Duke University Medical Center in Durham, N.C. What remains a bit of a mystery is how oncologists settle on one treatment plan over another.
As patients with colon cancer continue to live longer, they are exposed to more lines of chemotherapy with different agents. Yet no published study has examined community-based treatment patterns for metastatic colorectal cancer patients in the U.S., wrote S. Yousuf Zafar, MD, and colleagues from the division of medical oncology and the department of medicine as well as the department of biostatistics and bioinformatics.

Dr. Zafar's group conducted a two-part retrospective review of patients whose colon cancer was diagnosed between 2003 and 2006. Data were abstracted using patient sociodemographics, disease stage, medication dosage, clinicians’ reasons for choosing or discontinuing a therapy, and adverse events. They also looked at the chemotherapeutic regimens chosen: either FOLFOX or FOLFIRI. Patients were excluded if they had been part of a research protocol during first-line or second-line treatment (J Oncol Pract 5:228-233, 2009).
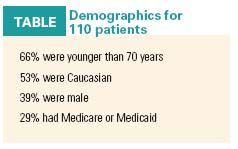
After examining 738 patient records, 400 patients were eligible for inclusion in the study and, of those, 110 made up the population of phase II of this review (see Table). The mean age of the patients was 57.9 years, and the majority of patients receiving any chemotherapy were younger than 70, the authors reported.
For most patients (64%), first-line therapy consisted of FOLFOX plus bevacizumab. FOLFIRI plus bevacizumab was the most common second-line regimen (13% of patients). The most often used third-line regimen was irinotecan (Camptosar) plus cetuximab (Erbitux) (21% of patients).
“As treatment progressed from first to third line, the use of bevacizumab, 5-FU, and oxaliplatin decreased, whereas the use of irinotecan increased,” the author stated.
Treatment decisions
The authors noted regimens were often used in first-line treatment even when phase III data hadn’t been published, indicating that oncologists are comfortable making therapeutic choices based on preliminary or phase II data. However, Dr. Zafar’s group also found that the reason why a physician chose a particular regimen was not well documented and, in fact, was missing from the majority (65%) of the medical records reviewed for this study. In those rare instances when treatment options were noted, 12% of the oncologists said they made a decision on the basis of perceived patient tolerability, while 10% cited treatment guidelines.
In an interview with Oncology News International, Dr. Zafar offered some thoughts on why the information was not documented. “The lack of documentation is more likely due to the complexity of the decision-making process and the time involved in appropriately documenting the process,” he said. “For example, the FOLFIRI regimen might be chosen over the FOLFOX regimen because the patient is an auto mechanic and his work would suffer from the inevitable neuropathy associated with FOLFOX.”
Another consideration may be whether a patient is a candidate for surgery in the future. Also, oncologists and patients may talk about treatment options, but there is no formal procedure for going on-the-record with the discussion. “The oncologist might simply document that FOLFIRI will be administered instead of FOLFOX. I am not surprised that the details of the decision-making process were not documented, but I do believe that more thorough documentation would be beneficial to both patients and care providers,” said Dr. Zafar, who is a medical instructor in the Duke division of medical oncology.
On the other hand, the reasons for ending therapy were documented and they included disease progression (29%) and tolerability or toxicity (18%). For instance, when choosing between an irinotecan-based regimen and an oxaliplatin-based regimen, oncologists may be more comfortable with the perceived toxicity profile of the latter, the authors wrote.
Finally, patient age played an important part in the delivery of chemotherapy. The authors pointed out that previously published research supports an age bias for older patients, even though these patients generally do as well as their younger counterparts. Dr. Zafar said that he believes this bias will diminish with the general graying of the population.
“As oncologists become more accustomed to treating older patients, and as older patients are enrolled in clinical trials, I think the age bias will lessen. The key to shrinking the age bias lies in greater enrollment and eligibility of older patients in clinical trials such that the data produced by trials are more representative of the general cancer population,” he said.
Dr. Zafar and colleagues are currently enrolling patients in a study to understand treatment-related decision making from the patient’s perspective. Also, Dr. Zafar is an investigator with the Cancer Care Outcomes Research & Surveillance Consortium (CanCORS), a National Cancer Institute-funded, prospective, multi-health system study designed to measure the quality of cancer care and associated health outcomes in the U.S.
“Data from this [CanCORS] study will hopefully shed more light on factors which influence treatment-related decision making for lung and colorectal cancers,” he said.
Q&A with Dr. Zafar
Q: Given the current emphasis on cost reduction in healthcare, how much influence do you think reimbursement rates had on oncologists and their treatment decisions in your study?
Dr. Zafar: Differences in reimbursement probably did not play a significant role in why one regimen was chosen over another because the differences are probably small. As far as drug costs are concerned, both regimens have similar overall costs. However, the issue of cost of care remains important, particularly in terms of out-of-pocket expenses that are borne by patients and not third-party payers. I am designing a study that aims to identify the extent of out-of-pocket expenses related to cancer care and how those expenses impact quality of care delivered.
Vantage Point
A challenging area with few data available
The analysis by Dr. Zafar's group confirms the tendency of physicians to make treatment decisions based on their familiarity with a particular therapy, wrote Dr. Eng and Dr. Kopetz in an accompanying JOP editorial. Dr. Eng, an associate professor, and Dr Kopetz, an assistant professor, are based at Houston’s M.D. Anderson Cancer Center (J Oncol Pract 5:233-235, 2009).
On the basis of these study results, there was a preference for FOLFOX even though European phase II trials have shown that FOLFOX and FOLFIRI are equivalent as first-line therapy, they said. In addition, FOLFOX was combined with bevacizumab, although the latter was approved by the FDA based on a phase III trial in combination with irinotecan rather than oxaliplatin (J Clin Oncol 23:4866-4875, 2005; J Clin Oncol 22:229-237, 2004).
“Familiarity with the drug of interest appears to have precedence in practice patterns over recent evidenced-based literature,” Drs. Eng and Kopetz wrote.
With regard to age, the commentators said that the study did not state the median age and the percentage of patients older than 70 years. They recommended that stratifying patients on the basis of biologic age (comorbidities, functional status) would be necessary for defining optimal chemotherapy utilization. Dr. Eng and Dr. Kopetz pointed out that the nine community practices analyzed in this study were all affiliated with Duke University, which may have influenced their practice patterns.
However, the study “emphasizes the importance and value of observational analyses...in improving quality measures for any practicing physician,” they wrote. This is “a challenging subject on which, to our knowledge, few data have been published.”