Survival Advantage for Docetaxel Combination in NSCLC
LISBON, Portugal-In patients with advanced or metastatic non-small-cell lung cancer (NSCLC), first-line docetaxel (Taxotere) plus cisplatin (Platinol) has been shown to offer a survival advantage relative to a standard regimen of vinorelbine
LISBON, PortugalIn patients with advanced or metastatic non-small-cell lung cancer (NSCLC), first-line docetaxel (Taxotere) plus cisplatin (Platinol) has been shown to offer a survival advantage relative to a standard regimen of vinorelbine (Navelbine) and cisplatin.
Frank V. Fossella, MD, medical director of the Thoracic Oncology Multidisciplinary Care Center at M.D. Anderson Cancer Center, reported results of the study (TAX 326) at the 11th European Cancer Conference (ECCO abstract 562).
With more than 1,200 patients from 29 countries enrolled, TAX 326 is one of the largest phase III trials ever conducted in NSCLC. Patients were randomized to receive docetaxel 75 mg/m² plus cisplatin 75 mg/m² every 3 weeks; docetaxel 75 mg/m² plus carboplatin (Paraplatin) AUC 6 every 3 weeks; or a control regimen of vinorelbine 25 mg/m²/wk plus cisplatin 100 mg/m² every 4 weeks.
"Overall survival in the docetaxel-cisplatin arm was greater than that in the control group, with a significant P value of .044," Dr. Fossella reported. "The curves separated at about 4 months and remained nonoverlapping throughout the follow-up period."
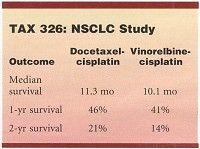
The docetaxel-cisplatin regimen yielded a median survival of 11.3 months, 1-year survival of 46%, and 2-year survival of 21%, in contrast to corresponding values of 10.1 months, 41%, and 14% for the control regimen (see Table). "The objective response rate was also in favor of docetaxel-cisplatin32% vs 25%, with a P value of .029," Dr. Fossella said.
The response rate, median survival, 1-year survival, and 2-year survival were equivalent in the docetaxel-carboplatin and vinorelbine-cisplatin arms.
All three treatment arms were generally well tolerated, Dr. Fossella said. The vinorelbine-cisplatin combination was responsible for the highest incidence of grade 3-4 toxicity, including anemia, nausea, and vomiting, whereas diarrhea was more common in patients treated with docetaxel-cisplatin.
The control regimen was associated with deteriorations in global quality of life and global health status, more weight loss, and less improvement in pain score, compared with both docetaxel-platinum arms.
"The impressive impact on survival and quality of life demonstrated with the docetaxel-cisplatin combination could profoundly change the treatment standard of patients with NSCLC," Dr. Fossella concluded.