The Evolving Landscape of Prostate Cancer Management
Maha Hussain, MD, FACP, FASCO, spoke about BRCA testing and ctDNA as diagnostic tools and PSMA-imaging and -targeted approaches in prostate cancer.
Maha Hussain, MD, FACP, FASCO
Prostate cancer remains the most common tumor type in males and the second leading cause of cancer deaths overall in the United States.1 With an estimated 299,010 new cases expected in 2024, the average lifetime risk of diagnosis is about 17%, while the risk of dying from the disease is approximately 3%.
The landscape of prostate cancer management has been dramatically reshaped by precision medicine. This approach has evolved from focusing on individual risk assessment to guiding diagnostic procedures, treatment decisions, and management of advanced disease.2
Precision medicine now incorporates:
- Risk assessment: Utilizing genetic and molecular
markers to identify high-risk populations - Diagnostic accuracy: Employing advanced imaging
techniques and biomarker analysis to enhance
prostate biopsy procedures - Tailored treatments: Optimizing therapy based on the
genetic profile of the tumor, balancing efficacy with
minimized adverse effects - Advanced care strategies: Personalizing treatment
for advanced prostate cancer using targeted therapies,
immunotherapies, and hormone-based treatments
aligned with the molecular characteristics of the tumor
Q / Which patient subpopulation would you test for BRCA1/2 mutations?
HUSSAIN /Anytime we have patients who have metastatic disease, testing them for BRCA or BRCA-like genes is going to be important, potentially for therapeutic purposes and particularly in metastatic castration-resistant disease. Other than that, testing for germline mutations is important.
Q / How do you foresee the role of circulating tumor DNA (ctDNA) as a diagnostic and prognostic tool in prostate cancer?
HUSSAIN /Potentially, ctDNA will play different roles. In situations in which we are looking for insight into the genomics of the tumor, ctDNA is going to be helpful in that regard. When it comes to the actual diagnosis of prostate cancer or the staging of disease, ctDNA is not a mature biomarker at this point. For diagnostic purposes, we need the tissue either via biopsy from the prostate or, if a patient has metastatic disease, then biopsy from tissues affected by metastasis. As it relates to monitoring disease activity, prostate- specific antigen (PSA) continues to be the most useful biomarker. Any additional biomarkers, such as ctDNA, will have to be validated as they relate to early detection of metastatic disease or micrometastatic disease and potential response to therapy.
How have PSMA diagnostics changed the way that prostate cancer is managed?
Q / How have PSMA diagnostics changed the way that prostate cancer is managed?
HUSSAIN /From a therapeutic standpoint, it provides an option that we did not have for patients before. Since 2004, when the first drug that prolonged life in castration-resistant disease—docetaxel—was approved, we now have infinitely more agents available for our patients. I’m hopeful that at some point we’re going to have potential cures for patients with metastatic disease.
Use of PSMA therapeutics, specifically, is an FDA-approved option based on impactful benefit with regard to progression-free survival and overall survival in the setting of end-stage mCRPC.
The imaging is very important. Ultimately, the goal is to detect cancer at a very early stage with the hope that we can target it, treat it appropriately, and potentially cure it. I do think that theranostics with regard to the imaging component is very helpful. However, it is clear that more research to define its impact on our treatment decisions is needed. Until now, when it comes to metastatic disease, all of the current data from key clinical trials that led to FDA approvals and guiding our therapy decisions were based on conventional imaging and not PSMA imaging.
I tell patients and my mentees: in reality, a tumor 1 to 3 cm in size is comprised of a billion cancer cells. Clearly, even if the PSMA imaging is negative and the PSA level is up, that does not mean that there is no micrometastatic disease. One cannot just 100% believe the negative imaging. There is cancer activity that has to be managed based on evidence-based standards of care and clinical judgment.
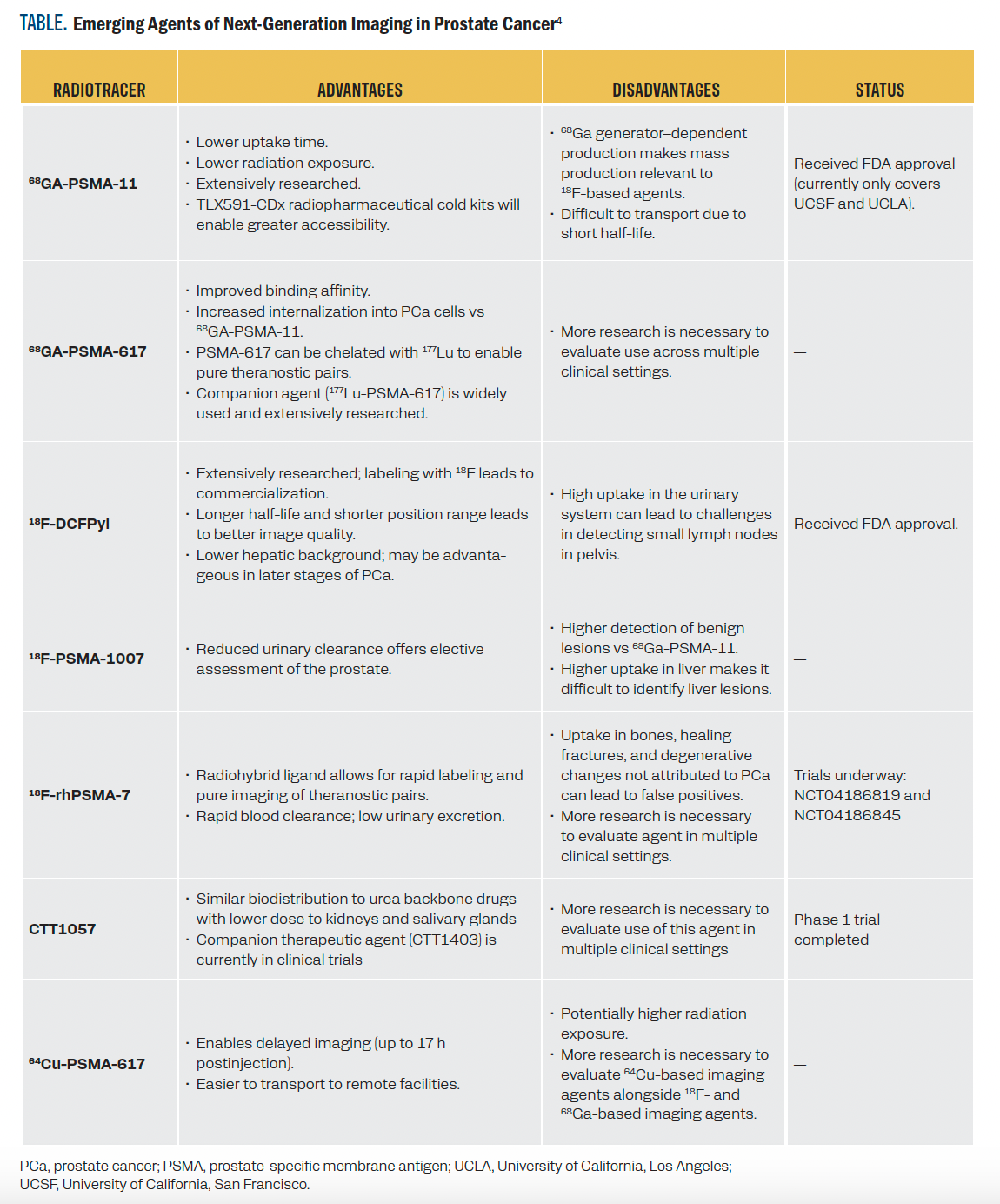
TABLE. Emerging Agents of Next-Generation Imaging in Prostate Cancer4
Q / Where do you see the field of prostate cancer going in the next 5 years?
HUSSAIN /Basically, the field is moving in a wonderful way with significant investment at all levels regarding research, science, clinical trials, and enrollment in different parts of the world, not just in Western countries. I think we are moving toward converting prostate cancer, when it comes to metastatic disease, from an imminently deadly disease to more of a chronic disease.
When I entered the field 3 decades ago, the median survival for men with metastatic hormone-sensitive disease was roughly 2.5 to 3 years. Now, it has doubled to nearly 6 years with a significant number of men living beyond 10 years. In fact, my practice includes several patients who have surpassed the 10-year mark since their initial diagnosis of metastatic hormone-sensitive disease.
We’ve seen similar progress in castration-resistant disease. The median survival was about 9 months when I started my clinical practice, but that has extended considerably. We’ve made substantial strides, and I’m optimistic that we’re moving closer to managing this as a chronic disease with the ultimate goal of finding a cure.
Where do you see the field headed in the next 5 years?
References
- Siegel RL, Giaquinto AN, Jemal A. Cancer statistics, 2024. CA Cancer J Clin. 2024;74(1):12-49. doi:10.3322/caac.21820
- Gillette CM, Yette GA, Cramer SD, Graham LS. Management of advanced prostate cancer in the precision oncology era. Cancers (Basel). 2023;15(9):2552. doi:10.3390/cancers15092552
- Haberkorn U, Eder M, Kopka K, Babich JW, Eisenhut M. New strategies in prostate cancer: Prostate-specific membrane antigen (PSMA) ligands for diagnosis and therapy. Clin Cancer Res. 2016;22(1):9-15. doi:10.1158/1078-0432.CCR-15-0820
- Murthy V, Aggarwal R, Koo PJ. The emerging role of next-generation imaging in prostate cancer. Curr Oncol Rep. 2022;24(1):33-42. doi:10.1007/s11912-021-01156-1
- Kase AM, Tan W, Copland JA 3rd, Cai H, Parent EE, Madan RA. The continuum of metastatic prostate cancer: interpreting PSMA PET findings in recurrent prostate cancer. Cancers (Basel). 2022;14(6):1361. doi:10.3390/cancers14061361
LEARNING OBJECTIVES
Upon successful completion of this activity, you should be better prepared to:
- Analyze the evolution of prostate cancer management from acute to chronic, identifying key challenges in treating advanced stages.
- Evaluate the role of emerging biomarkers and targets, especially PSMA, in improving detection and treatment of metastatic castration-resistant prostate cancer.
- Assess how precision medicine has transformed prostate cancer care across the disease spectrum, from risk assessment to advanced disease management.
RELEASE DATE: October 1, 2024 EXPIRATION DATE: October 1, 2025
INSTRUCTIONS FOR PARTICIPATION and HOW TO RECEIVE CREDIT
1. Read this activity in its entirety.
2. Go to https://gotoper.com/nygu24psma-postref to access and complete the posttest
3. Answer the evaluation questions.
4. Request credit using the drop down menu.
YOU MAY IMMEDIATELY DOWNLOAD YOUR CERTIFICATE.
Faculty, Staff, and Planners’ Disclosures
In accordance with ACCME Guidelines, PER® has identified and resolved all COI for faculty, staff, and planners prior to the start of this activity by using a multistep process.
Disclosures (Dr Hussain): Grant/Research Support (paid to institution): Arvinas, AstraZeneca, Bayer; Advisory Board: AstraZeneca, Bayer, Convergent, Novartis, Tango; Honoraria: AstraZeneca; Travel: Bayer.
The staff of PER® have no relevant financial relationships with commercial interests to disclose.
Off-label Disclosure and Disclaimer
This activity may or may not discuss investigational, unapproved, or off-label use of drugs. Learners are advised to consult prescribing information for any products discussed. The information provided in this activity is for accredited continuing education purposes only and is not meant to substitute for the independent clinical judgment of a health care professional relative to diagnostic, treatment, or management options for a specific patient’s medical condition. The opinions expressed in the content are solely those of the individual faculty members, and do not reflect those of PER® or any company that provided commercial support for this activity.
Accreditation/Credit Designation
Physicians’ Education Resource®, LLC, is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide continuing medical education for physicians. Physicians’ Education Resource®, LLC, designates this enduring material for a maximum of 0.5 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Prolaris in Practice: Guiding ADT Benefits, Clinical Application, and Expert Insights From ACRO 2025
April 15th 2025Steven E. Finkelstein, MD, DABR, FACRO discuses how Prolaris distinguishes itself from other genomic biomarker platforms by providing uniquely actionable clinical information that quantifies the absolute benefit of androgen deprivation therapy when added to radiation therapy, offering clinicians a more precise tool for personalizing prostate cancer treatment strategies.