The Negative Impact of the COVID-19 Pandemic on Oncology Care at an Academic Cancer Referral Center
COVID-19 created unexpected delays in oncologic treatment. This study sought to assess the volume of missed cancer-related services due to the pandemic.
Nakayama is affiliated with the Division of Gynecologic Oncology, Department of Obstetrics and Gynecology of the University Hospitals/Cleveland Medical Center in Cleveland, OH.

Wang is affiliated with the Research and Education Division, University Hospitals of Cleveland.

Cioffi is affiliated with the Department of Population and Quantitative Health Sciences, Case Western Reserve University School of Medicine; the Research and Education Division of the University Hospitals/Cleveland Medical Center; and the Cleveland Center for Health Outcomes Research.

Waite is affiliated with the Department of Population and Quantitative Health Sciences, Case Western Reserve University School of Medicine; the Research and Education Division of the University Hospitals/Cleveland Medical Center; and the Cleveland Center for Health Outcomes Research.

Patil is affiliated with Case Comprehensive Cancer Center of Cleveland.

Kyasaram is affiliated with the Department of Cancer Informatics of the Seidman Cancer Center in Cleveland.

Shanahan is affiliated with the Department of Cancer Informatics of the Seidman Cancer Center in Cleveland.

Caimi is affiliated with the Division of Hematology, Department of Medicine at the University Hospitals/Seidman Cancer Center.
Barnholtz-Sloan is affiliated with the Department of Population and Quantitative Health Sciences, Case Western Reserve University School of Medicine; the Research and Education Division of the University Hospitals/ Cleveland Medical Center; the Research and Education Division, University Hospitals of Cleveland; and the Cleveland Center for Health Outcomes Research.

ABSTRACT
Objectives: COVID-19 created unexpected delays in oncologic treatment. This study sought to assess the volume of missed cancer-related services due to the pandemic.
Methods: This case-controlled trial evaluated more than 345,000 oncologic clinic, lab, and radiation appointments from January 1, 2019, through December 31, 2020, and surgery appointments from January 1, 2019, through October 31, 2020. All patients at the Seidman Cancer Center with a cancer diagnosis based on a comprehensive list of 2178 International Classification of Diseases, Ninth Edition (ICD-9) and ICD-10 codes were included in the analysis. Subgroup analyses based on age, race, and sex were also performed.
Results: Clinic, lab, and surgical visit cancellations increased by 4.20% (P <.001), 4.84% (P <.001), and 5.22% (P <.001), respectively. In the first 10 months of 2020, there were 703 (9.2%) fewer surgeries compared with the same time period in 2019. The following cancellation rates peaked in March 2020: clinic visits (26.53%), labs (43.66%), surgery (34.00%). Radiation oncology (12.53%) cancellations peaked in April 2020. Prior to the emergence of COVID-19, the group aged 0 to 39 years had the highest clinic cancellation rate (17.85%) compared with patients aged 40 to 64 years (15.95%) and 65 years and older (14.52%; P <.001). Men cancelled (15.63%) significantly more often than women (14.93%; P <.001) in 2019. This reversed during the pandemic: Women (19.56%) cancelled more frequently than men (19.20%; P <.036).
Conclusions: There was a large increase in cancelled oncologic care in 2020, which has implications for delayed diagnosis and treatment. This was especially true for patients older than 65 years and for women. These delays could result in patients presenting with more advanced disease, complicating morbidities, and ultimately worse long-term outcomes.
Oncology (Williston Park). 2021;35(8):462-470.
DOI: 10.46883/ONC.2021.3508.0462
Introduction
The COVID-19 pandemic created an unprecedented situation pitting the urgent need to appropriately treat patients with cancer against the unknown level of risk of subjecting patients to immunosuppressive therapies during a pandemic. Attempts to strike a balance of these risks led to delays in care.1-3 Statistical modeling of delayed care of the most common cancers in the United Kingdom estimated up to several thousand additional deaths.4,5 While it will be years before we will have an accurate determination on patient morbidity and mortality, we can gain insight on the potential impact by examining the number of delayed medical visits, tests, and procedures. Multiple small reports have indicated a drop in procedures.6-8 One large study examining a sample of Medicare data showed a significant drop in cancer screening procedures and office visits, but it is unclear if these were cancer-related visits.9
Here, we assess the volume of missed cancer-related services due to the COVID-19 pandemic, as well as the populations impacted. We hypothesized that there would be significantly more delays in cancer-related care, delays that would be influenced by age, sex, and race.
Methods
Patient Cohort
Under a protocol approved by the University Hospitals Seidman Cancer Center Institutional Review Board, a search of all appointment data from patients with cancer in the in the Seidman Cancer Center was performed. Only patients with a cancer diagnosis (>345,000 patient visits annually) based on a comprehensive list of 2178 International Classification of Diseases, Ninth Revision (ICD-9) and ICD-10 codes were eligible (eAppendix A). Clinic, lab, and radiation appointments from January 1, 2019, through December 31, 2020, and surgery appointments from January 1, 2019, through October 31, 2020, were obtained. For each of the 4 groups of appointment types, rates of cancellation (cancellation count divided by appointment count) were stratified by age group (0-39 years, 40-64 years, 65 years or older),10 sex (male or female), and race (White, Black, or other) on a monthly basis.
Statistical Analysis
Clinic, lab, and radiation appointments for all of 2019 and 2020 were evaluated. Given data availability, the first 10 months of surgeries for 2020 were analyzed. Descriptive statistics were used to assess any association of cancellation rate between 2019 and 2020 for both overall data, and stratified by age group, sex, and race for each appointment type respectively, where the χ2 test of independence was used for comparison. The trend comparison of appointment rates was also examined by trend plot both for overall data and stratified by age group, sex, and race for each appointment type respectively. A series of plots describe the cancellation trends of years 2019 and 2020. A statistical test for the difference in trend is not provided in this analysis due to the limited number of observations.
TABLE 1. Oncologic Visit Cancellation Changes Related to COVID-19 Pandemic (2019 and 2020)
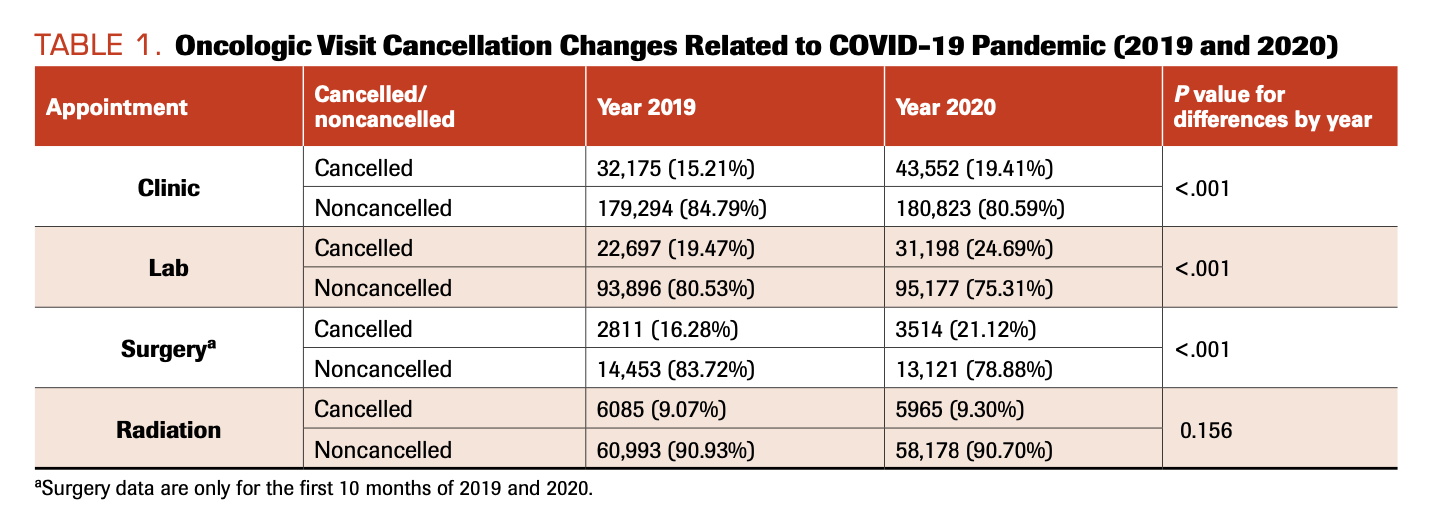
TABLE 2. Oncologic Appointment Cancellations by Year and Stratified by Age, Sex, and Race: 2019-2020
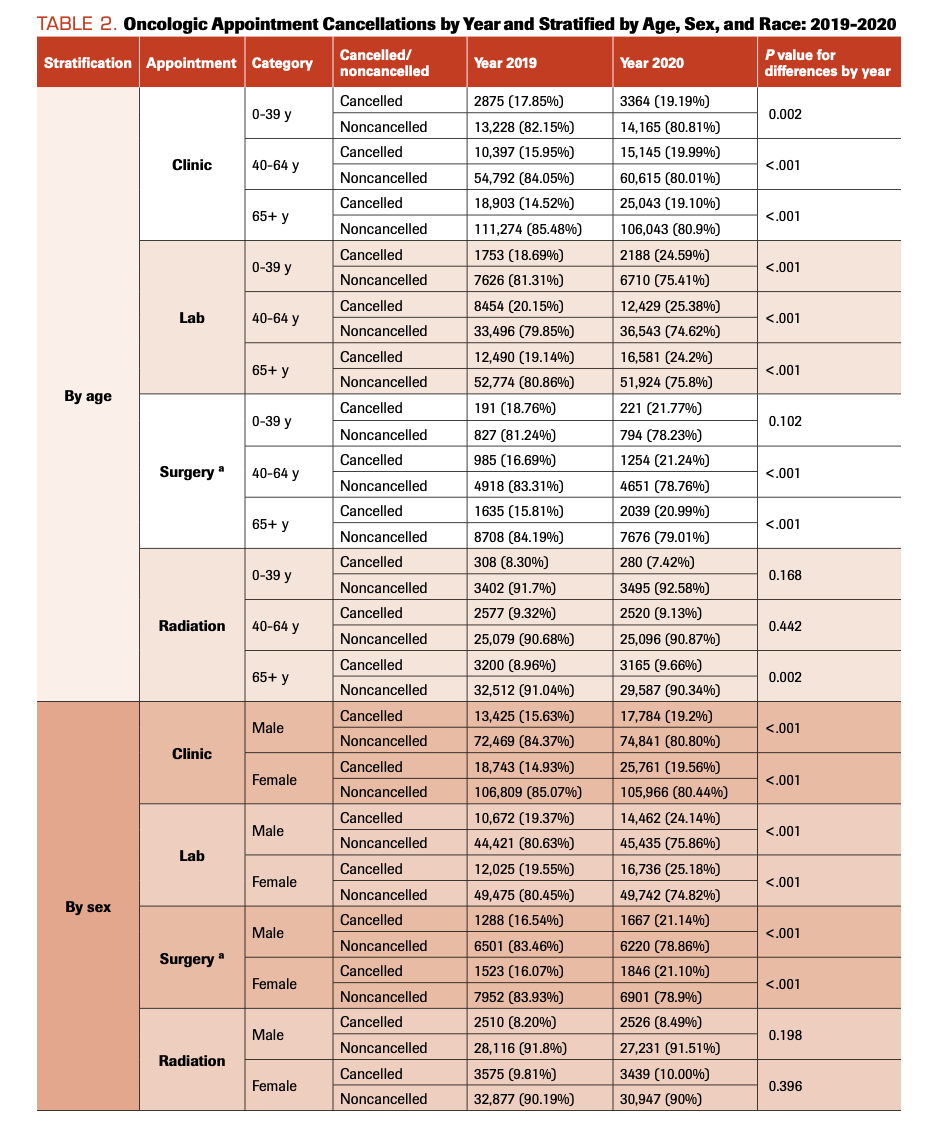
TABLE 2. Oncologic Appointment Cancellations CONTINUED
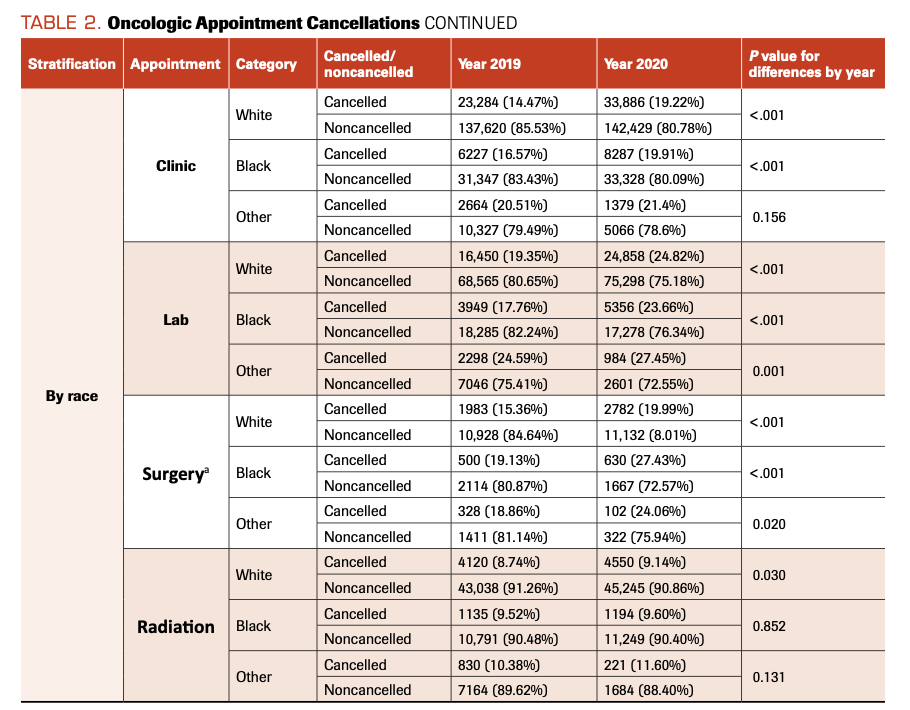
FIGURE 1. Trends in Oncologic Appointment Cancellation Rates by Year (2019-2020) and by Appointment Type: (A) Clinic, (B) Lab, (C) Surgical, and (D) Radiation Therapy
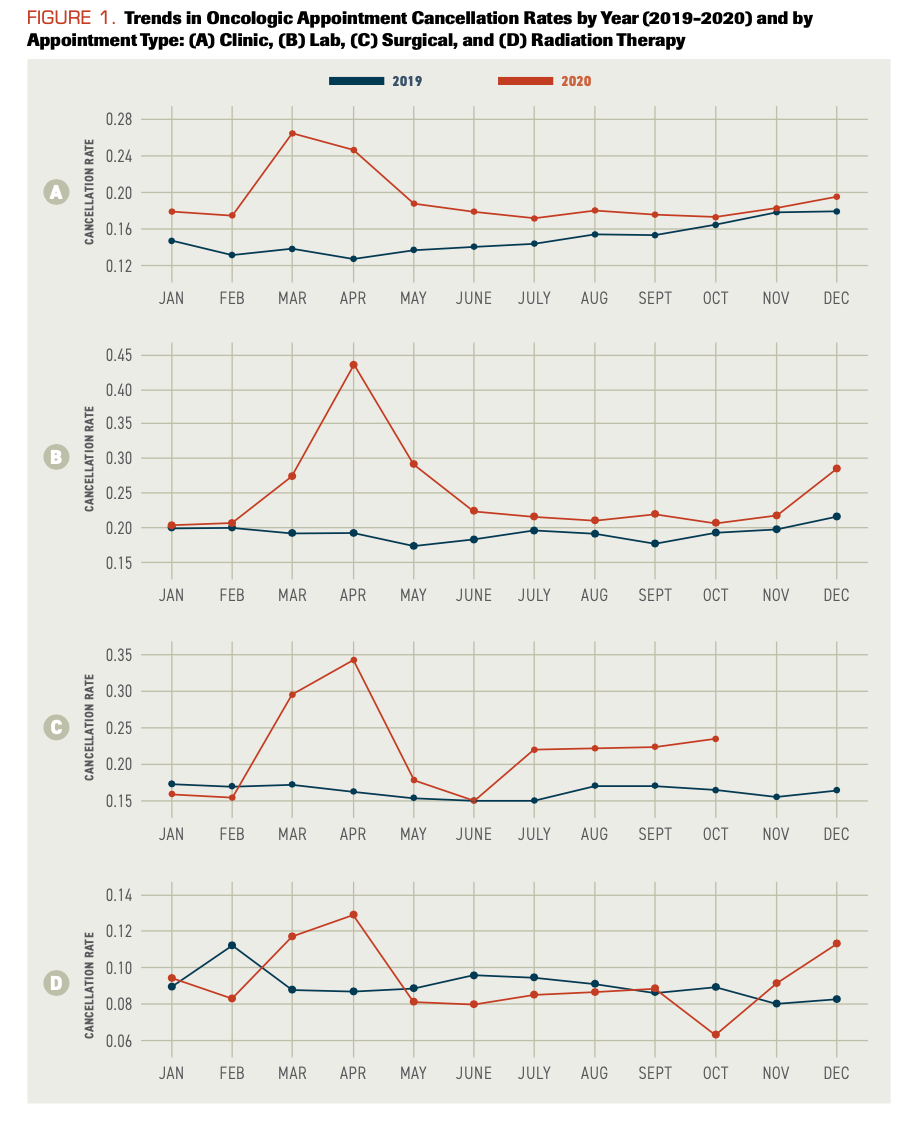
TABLE 3. Clinic Appointment Cancellations by Year Stratified by Age, Sex, and Race: 2019-2020
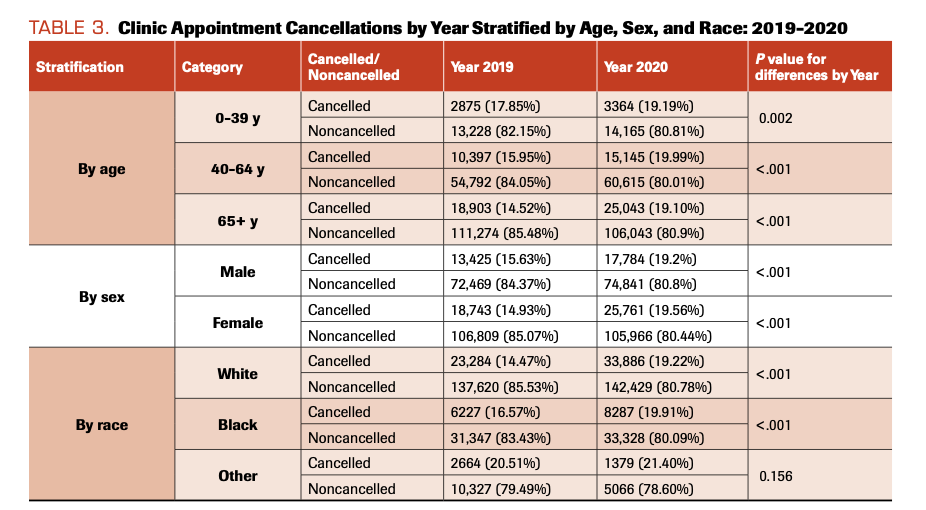
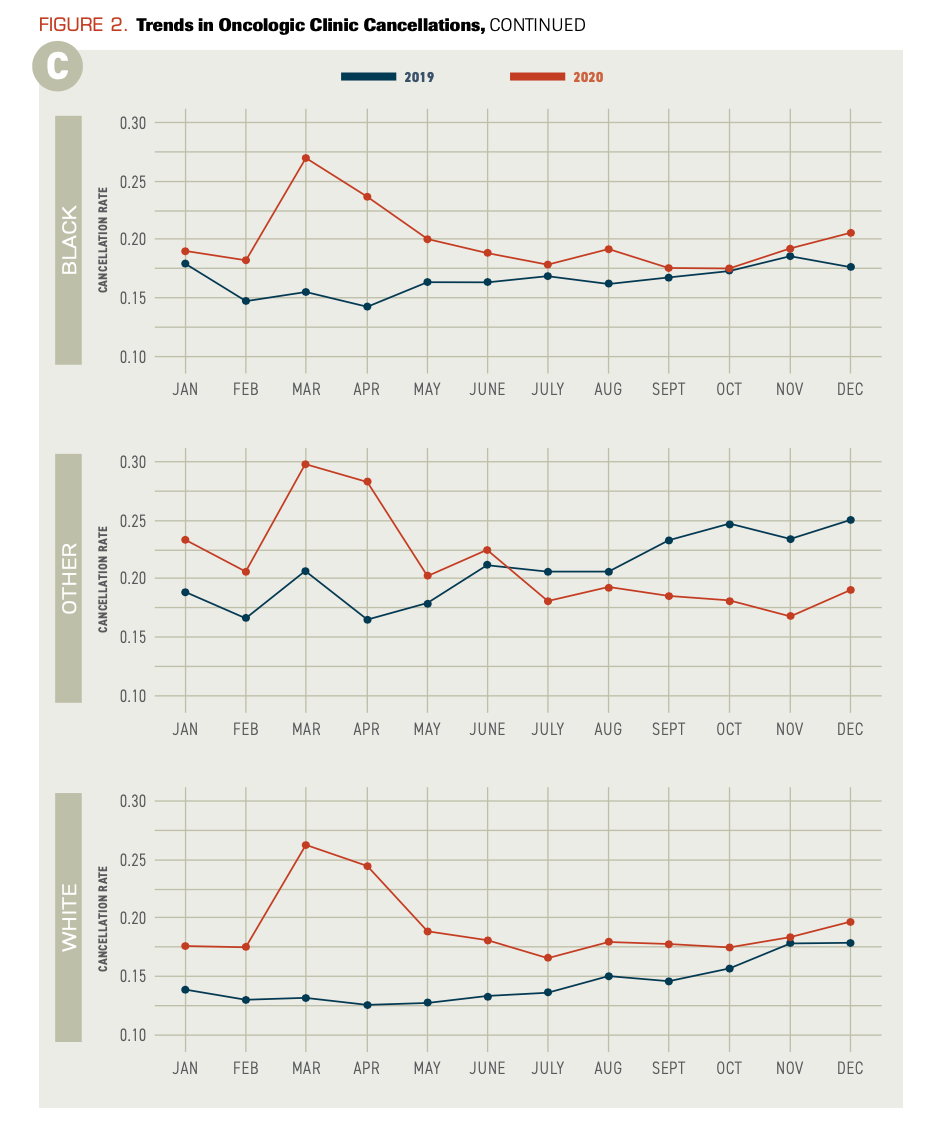
FIGURE 2. Trends in Oncologic Clinic Cancellations, Stratified by (A) Age, (B) Sex, and (C) Race
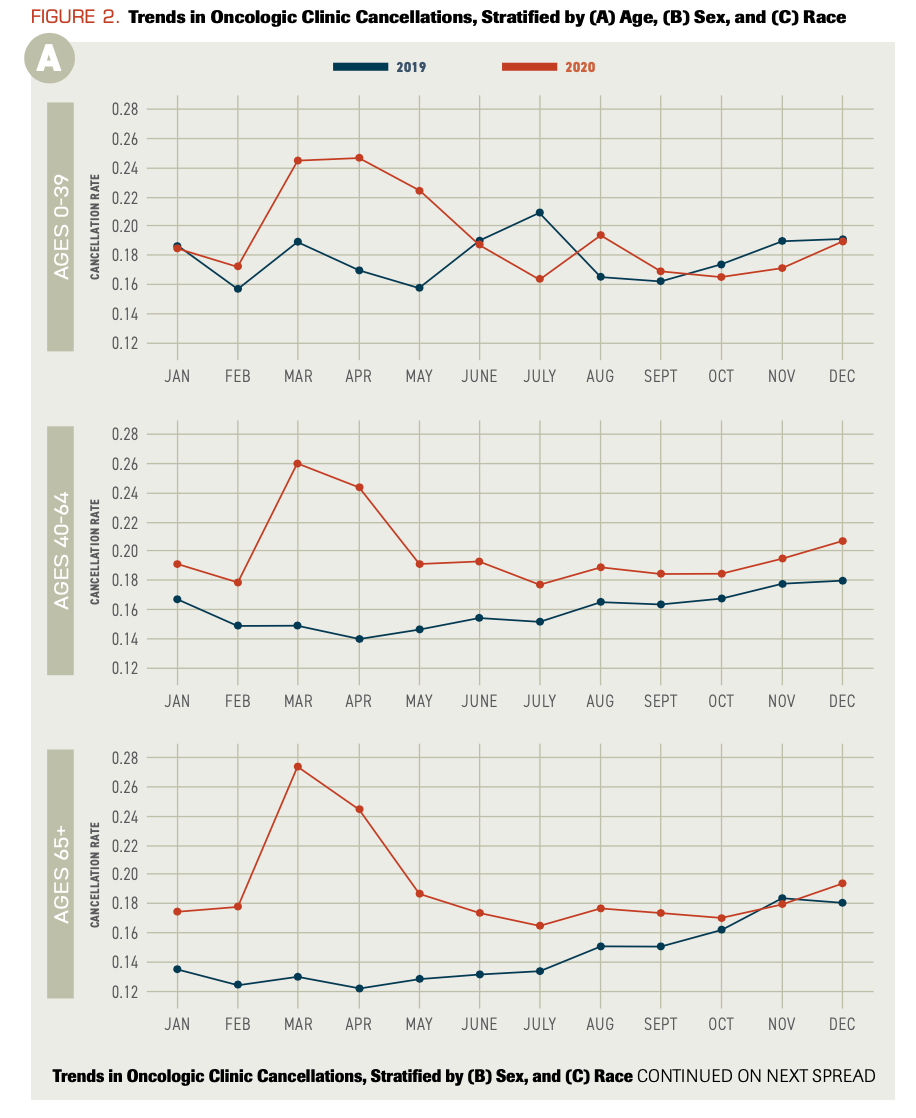
FIGURE 2. Trends in Oncologic Clinic Cancellations, CONTINUED

FIGURE 2. Trends in Oncologic Clinic Cancellations, CONTINUED
Results
There was a significant increase in the number of cancellations for oncologic care from 2019 to 2020. Clinic, lab, and surgical visit cancellations increased by 4.20% (P <.001), 4.84% (P <.001), and 5.22% (P <.001), respectively (Table 1). This translates into an increase of 11,377 clinical outpatient oncology appointment cancellations and 8502 lab visit cancellations in 2020. Compared with the same time period in 2019, there were 703 (9.2%) fewer surgeries in the first 10 months of 2020. The rate of radiation oncology cancellations was about 9% in both years (P = .156). The pattern of greater clinic, lab, and surgery cancellations with unchanged radiation visits stayed fairly consistent when patients were stratified by age, sex, and race (Table 2). Exceptions included the group aged 0 to 39 years (P = .102) and patients listed as “other” for racial group (P = .156), which had unchanged surgery and clinic cancellation rates, respectively. Unlike other groups, the White (P = .002) and 65 years or older (P = .030) groups had a significant increases in their radiation oncology cancellations. Cancellation rates for clinic, lab, surgery, and radiation therapy are shown in Figure 1. The following cancellations peaked in March 2020: clinic visits (26.53%), labs (43.66%), surgery (34.00%). Radiation oncology (12.53%) cancellations peaked in April 2020. Cancellation rates began to rise again in October/November 2020 in all areas.
Due to hospital mandates restricting appointments to only time-sensitive care during the initial months of the COVID-19 pandemic, clinic visits were evaluated in greater detail (Table 3). In 2019, prior to the widespread awareness of COVID-19, the group aged 0 to 39 years had the highest clinic cancellation rate (17.85%) compared with those aged 40 to 64 years (15.95%) and 65 years and older (14.52%; P <.001). As age in years increases, the gap between 2019 and 2020 cancellation rates widens, especially in the first half of 2020 when COVID-19 restrictions were first put in place (Figure 2A). Men cancelled (15.63%) significantly more often than women (14.93%; P <.001) in 2019 (Figure 2B). This reversed in 2020, during the pandemic, to women (19.56%) cancelling more frequently than men (19.20%; P <.036). Racial groups also had distinct trends. The patients listed as “other” for racial group had the highest clinic cancellation rate in both 2019 (20.51%) and 2020 (21.4%). White patients had the lowest cancellation rate in 2019 (14.47%) and 2020 (19.22%). All racial groups showed an increase in cancellation rates at the end of 2019 (Figure 2C). The first 3 months of 2019 compared with the last 3 months of 2019 showed a significant increase in the mean cancellation rate for Black patients (1.90%; P = .002), White patients (3.80%; P = .002), and those of other racial groups (5.61%; P = .002).
Discussion
There are clear trends in the cancellation rates that coincide with the course of the COVID-19 pandemic. Cancellations spiked in March and April 2020 as infection rates began to rise and states implemented restrictions. At the end of 2020, there is a suggestion of another rise in cancellations corresponding with the peak of new COVID-19 infections that December.11 This resulted in 9.2% fewer surgeries despite a stable volume of completed clinic visits. It is unclear if surgery cancellations were patient-driven or the result of pandemic restrictions on elective surgeries. A combination of both is likely responsible. Interestingly, radiation oncology cancellations were unchanged. This likely reflects the urgency of most radiation referrals and the importance of limiting delays in radiation once therapy has begun.
When the groups were stratified by age, sex, and race, several interesting patterns emerged. The surgical cancellation rate among the youngest group, aged 0 to 39 years, was unchanged by COVID-19 restrictions. This could be the result of lower morbidity from COVID-19 infections in young patients as well as of surgeries being time-sensitive in this population. When the clinic cancellation rate was evaluated, all age groups showed an increase from 2019 to 2020. However, Figure 2A illustrates that the youngest group’s cancellation rate changed the least and that of the oldest group changed the most. Given the increased risk of COVID-19 infection in older patients, these results are expected. One surprising finding, however, was the shift from a greater male cancellation rate to female. While further research is needed, we hypothesize that the burden of health care needs typically falls on women, and the rate of female cancellations rose as women met the needs of other family members.
Limitations
Limitations of this study include pote tial selection bias and the study population being drawn from a large academic medical center. This is partially mitigated by including all cancer patients in the system, which includes outlying clinic centers.
Conclusions
This study illustrates the large number of delayed oncologic visits due to the COVID-19 pandemic at an academic cancer referral center. These patients will reenter care either emergently or when the risk of infection abates, and the health care system will need to have resources in place to manage the situation. This will be especially true in older patients and in women, both representing groups who disproportionately delayed care. Overall, there was a large decrease in oncologic care in 2020, which has implications for delayed diagnosis and treatment. This could result in patients presenting in the future with more advanced disease, more complicating morbidities, and ultimately worse long-term outcomes. Oncologists and hospital systems should prepare accordingly for increased demand as the threat of COVID-19 infection diminishes and patients present for care. ν
Financial Disclosure: The authors have no significant interest or other relationship with the manufacturer of any product or provider of any service mentioned in this article.
Conflicts of Interest: NM speaks for a Merck and Eisai and consults for AstraZeneca, Clovis Oncology, and Xodus Medical.
References
1. Gultekin M, Ak S, Ayhan A, et al. Perspectives, fears and expectations of patients with gynaecological cancers during the COVID‐19 pandemic: a pan‐European study of the European Network of Gynaecological Cancer Advocacy Groups (ENGAGe). Cancer Med. 2021;10(1):208-209. doi:10.1002/cam4.3605
2. Al‐Shamsi HO, Alhazzani W, Alhuraiji A, et al. A practical approach to the management of cancer patients during the novel coronavirus disease 2019 (COVID‐19) pandemic: an international collaborative group. Oncologist. 2020;25(6):e936-e945. doi:10.1634/theoncologist.2020-0213
3. Curigliano G, Banerjee S, Cervantes A, et al; panel members. Managing cancer patients during the COVID-19 pandemic: an ESMO multidisciplinary expert consensus. Ann Oncol. 2020;31(10):1320-1335. doi:10.1016/j.annonc.2020.07.010
4. Sud A, Torr B, Jones ME, et al. Effect of delays in the 2-week-wait cancer referral pathway during the COVID-19 pandemic on cancer survival in the UK: a modelling study. Lancet Oncol. 2020;21(8):1035-1044. doi:10.1016/S1470-2045(20)30392-2
5. Maringe C, Spicer J, Morris M, et al. The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study. Lancet Oncol. 2020;21(8):1023-1034. doi:10.1016/S1470-2045(20)30388-0
6. Tzeng C-WD, Teshome M, Katz MHG, et al. Cancer surgery scheduling during and after the COVID-19 first wave: the MD Anderson Cancer Center experience. Ann Surg. 2020;272(2):e106-e111. doi:10.1097/SLA.0000000000004092
7. Brugel M, Carlier C, Essner C, et al. Dramatic changes in oncology care pathways during the COVID-19 pandemic: The French ONCOCARE-COV study. Oncologist. 2021;26(2):e338-e341. doi:10.1002/onco.13578
8. Riemann S, Speck I, Gerstacker K, Becker C, Knopf A. Collateral damage of the COVID-19 pandemic: an alarming decline in critical procedures in otorhinolaryngology in a German university hospital. Eur Arch Otorhinolaryngol. Published online December 15, 2020. doi:10.1007/s00405-020-06519-1
9. Patt D, Gordan L, Diaz M, et al. Impact of COVID-19 on cancer care: how the pandemic is delaying cancer diagnosis and treatment for American seniors. JCO Clin Cancer Inform. 2020;4:1059-1071. doi:10.1200/cci.20.00134
10. Risk for COVID-19 infection, hospitalization, and death by age group. CDC. Updated July 19, 2021. Accessed March 31, 2021. https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-age.html
11. United States [COVID-19] Overview. Johns Hopkins University of Medicine Coronavirus Resource Center. Updated July 24, 2021. Accessed July 17, 2021. https://coronavirus.jhu.edu/region/united-states