Use of Immunotherapy in Patients With Cancer During the COVID-19 Pandemic
This article discusses the potential implications of using checkpoint inhibitors during the COVID-19 pandemic.
Soares is a medical oncologist at Centro Paulista de Oncologia and Hospital Israelita Albert Einstein.

Schutz is a medical oncologist at Beneficência Portuguesa de São Paulo.

Bastos is a genitourinary oncologist at Hospital Sírio-Libanês and Instituto do Cancer do Estado de São Paulo (Sao Paulo Cancer Institute), Brazil. He is currently the chair of the genitourinary branch of the Latin American Cooperative Oncology Group.

Jardim is a medical oncologist at Hospital Sírio- Libanês in São Paulo, Brazil. He is currently the head of clinical research at Sírio-Libanês and coordinator of oncology at the Hospital Unit in Itaim.

Monteiro is a medical oncologist at Hospital Santa Lucia and Hospital de Universitario de Brasilia.

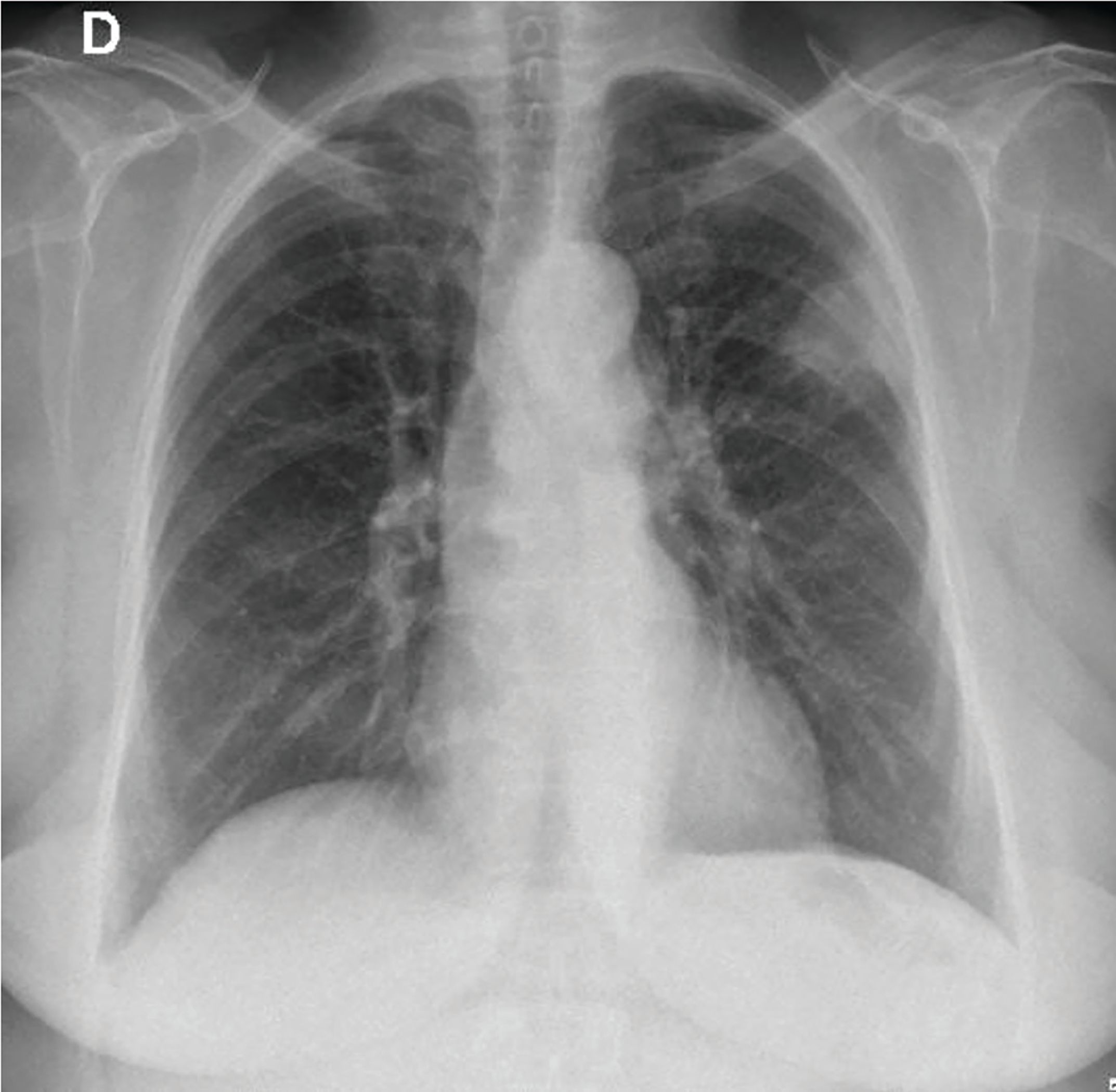
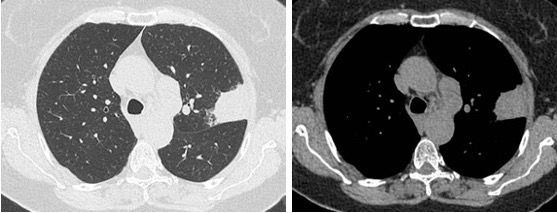
In an asymptomatic 77-year-old woman, former 55 pack-years smoker, a routine X-ray showed a 45-mm superior left lobe lesion (Figure 1). A chest CT scan confirmed a 36-mm superior left lobe lesion and an aortic-pulmonary lymph node enlargement measuring 42 mm, suspicious for neoplasia (Figure 2). A PET-CT scan showed an elevated uptake in the primary lesion, in the aortic-pulmonary lymph node, and in the left hilar lymph node with a standardized uptake value – 40 and 4.3, respectively (Figure 3).
CT-guided lung biopsy showed a lung squamous cell carcinoma. An endobronchial ultrasound-guided transbronchial needle aspiration for lymph-node staging was negative for lymph node spread. Brain MRI was negative. Final staging was determined to be a IIIA (T2bN2) squamous cell carcinoma of the lung.
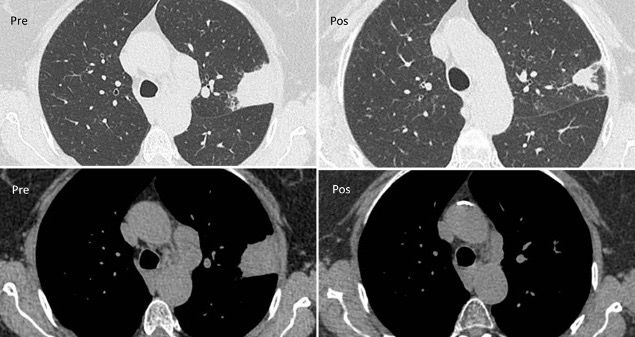
After multidisciplinary team consultation, the patient received radiotherapy (Figure 4) with concurrent weekly paclitaxel and carboplatin. The treatment was well tolerated, and the patient had no toxicity. A CT scan after therapy showed a good response (Figure 5). After chemo-radiotherapy treatment, the patient started durvalumab as consolidation therapy.
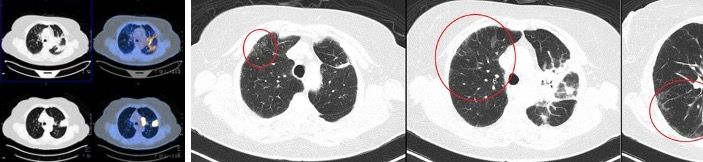
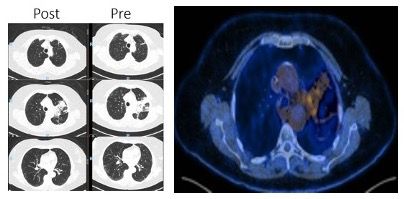
Three months after starting durvalumab, the patient developed a dry cough with no other symptoms. Physical examination was normal and oxygen saturation was 96%. The patient denied contact with coronavirus disease 2019 (COVID-19) positive patients and was practicing all measures of COVID-19 protection. A new PET-CT showed an excellent tumor response, with appearance of some ground-glass opacity in the lungs (Figure 6). A polymerase chain reaction (PCR) naso- and oropharyngeal test to detect severe acute respiratory syndrome (SARS) coronavirus 2 (SARS-CoV-2) was negative, as was the full respiratory viral panel. A subsequent durvalumab dose was put on hold to better define the diagnosis. After 48 hours, the patient repeated the SARS-CoV-2 test; the results were again negative. Due to the COVID-19 pandemic and her very good clinical status, the patient did not receive corticosteroids at this time and was instead monitored every 48 hours with telemedicine. The cough disappeared after 1 week and a new COVID-19 test was negative. Durvalumab was reinitiated 2 weeks later and the patient is still receiving the medication with no new symptoms, with a very good tolerance. After 3 months a new PET-CT (Figure 7) showed an almost complete resolution of the ground-glass opacity, and the patient maintains an excellent response.
Introduction
SARS-CoV-2 is the virus responsible for the biggest pandemic in recent years, COVID-19. SARS-Cov-2 is a positive sense single-strand RNA virus in the coronaviridae family with a potential to infect humans, including transmission between them. After the first case was reported in Wuhan, China, at the end of 2019, COVID-19 reached global proportions, leading the World Health Organization to declare it a pandemic on March 11, 2020. Globally, COVID-19 infection rates are still rising and as of August 31, 2020, 25,402,968 people were infected in 188 countries, with 849,303 deaths.1,2
SARS-CoV-2 causes an asymptomatic or mild infection in approximately 80% of cases. However, it presents in the other 20% as a symptomatic and potentially serious infection. The most severe problems caused by SARS-CoV-2 are respiratory failure, due to pneumonitis, and/or multiple organ failure. The evolution of this serious disease is attributed to an exacerbated inflammatory response.2 After contamination and contact with the host, SARS-CoV-2 uses angiotensin-converting-enzyme 2 (ACE2) as receptor to cell invasion. During this process, type II transmembrane serine protease (TMPRSS2) expression seems to be important as a coadjuvant protein to assist SARS-CoV-2 in cell invasion.3,4 Patients who progress to the severe form of the disease have an inflammatory response that leads to a reduction of the expression of cytotoxic CD8+ and CD4+ T lymphocytes. Also, important inflammatory cytokines such as interleukin-6 (IL-6), tumor necrosis factor–α, and interferon-ɣ (IFN-ɣ), as well as others, increase.2,4,5 In this context, as with other viral infections, increased expression of regulatory molecules of inflammatory response, like PD-1 and PD-L1, occurs.2, 4-6
COVID-19 and Cancer
The morbidity and mortality of COVID-19 is higher in elderly and male patients, as well as in those with comorbidities. The most relevant comorbidities associated with serious outcomes are hypertension, diabetes, cardiovascular disease, obesity, dementia, chronic respiratory disease, kidney disease, liver disease, autoimmune disease, immunosuppressive disease, and cancer.
Specifically in cancer patients, those who are elderly and/or who have lung cancer, hematologic malignancy, advanced-stage disease, active solid tumor, or a diagnosis of solid tumor in the past 5 years, or who had oncological surgery performed in the last 30 days, are at highest risk of an unfavorable outcome.
With regard to systemic oncological treatments, correlation of the use of immunotherapy with checkpoint inhibitors (anti–PD-1, anti–PD-L1, and anti–CTLA-4) with the risk of more severe COVID-19 infection is uncertain. So far, published data are conflicting; some data show serious outcomes in patients receiving immunotherapy, while others do not.6-12
Figure 1. X-ray and the left superior lesion.
Considering the magnitude of the pandemic, several expert-opinion guidelines have emerged, aiming to minimize both the risk of infection and complications related to COVID-19. Many focused on recommended measures, such as social distancing, and assess the risks and benefits of delaying systemic oncological treatments. Additionally, in clinical practice, many patients have chosen to postpone their oncological treatments. However, evidence shows that cancer-related mortality increases due to delays in cancer diagnosis and treatment, even if such delays might seem warranted due to the COVID-19 threat.13,14
Figure 2. CT scan with pulmonary lesion and mediastinal lymph node.
COVID-19 Risk in Cancer Patients Receiving Immunotherapy
In patients with COVID-19, pneumonitis is the main cause of hospitalization and death. However, pneumonitis is also an adverse event (AE) caused by immunotherapy (IMT); it occurs in between 2% and 5% of patients receiving IMT monotherapy and in about 10% of patients receiving IMT combination therapy (anti–PD-1/PD-L1 + anti–CTLA-4). Notably, although pneumonitis is not a common AE in patients receiving IMT, it is associated with a high mortality rate (about 35%).6,11,15
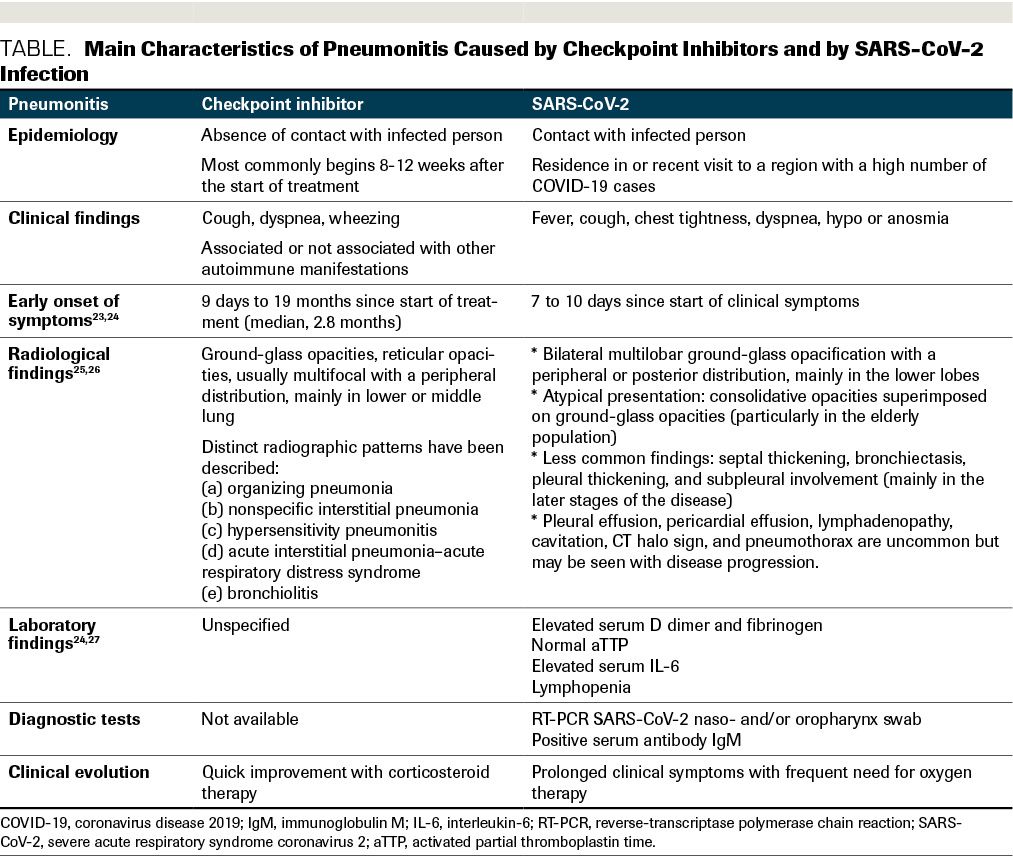
Clinically, the pneumonitis caused by SARS-CoV-2 and that induced by IMT can be confused, because symptoms such as fever, dry cough, dyspnea, and fatigue are common in both presentations. The reverse-transcriptase PCR (RT-PCR) test to diagnose COVID-19 can register a false negative during the first days of symptoms7,11 (Table), and in many localities, results of the test can take more than a few days to be processed. These factors can increase the confusion surrounding the diagnosis and can delay the decision of whether or not to begin treatment for IMT-induced pneumonitis.
Another challenge is that imaging findings from both causes of pneumonitis can be indistinguishable. The most common presentation in COVID-19 patients is the pattern of ground-glass opacities seen on a CT scan of the chest, which is a possible characteristic of IMT-related pneumonitis.6,11,16 Therefore, statement A is correct.
Figure 3. PET-CT with pulmonary and lymph node involvement.
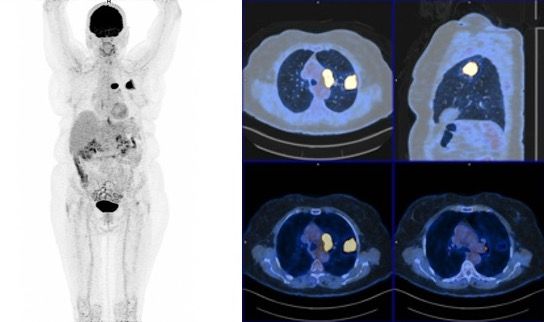
TABLE. Main Characteristics of Pneumonitis Caused by Checkpoint Inhibitors and by SARS-CoV-2 Infection
During this pandemic, treating patients with cancer using IMT can be challenging, and oncologists face several quandaries. The first is whether IMT could potentially have a protective effect, reducing the risk of SARS-CoV-2 infection because the therapy may enhance patient immunity. However, only observational studies have raised the possibility of the protective effect of IMT, and further data are required to confirm this hypothesis and use it to guide the management of patients with cancer.
Conversely, it is possible that patients receiving IMT may be more susceptible to SARS-CoV-2 infection because of higher expression of ACE2 and TMPRSS2 in the case of naturally or IMT-stimulated inflamed tumors.3-5,12 However, previous data do not demonstrate that the use of IMT increases the risk of other viral pneumonias, such as influenza.17 Therefore, statement B is also correct. Yet it is known that in severe cases of pneumonitis, the host experiences exacerbated inflammation, and in these cases, the use of IMT could enhance the inflammatory response. Rarely, the IMT itself can cause cytokine release syndrome, characterized by the release of cytokines including IL-6 and IFN-ɣ. In the case of SARS-CoV-2 infection in patients receiving IMT, the risk of cytokine release syndrome is high. Thus, the second quandary oncologists face is the challenge to correctly diagnosis SARS-CoV-2 infection or IMT-induced pneumonitis.4,6,11
Figure 4. Radiotherapy plan.
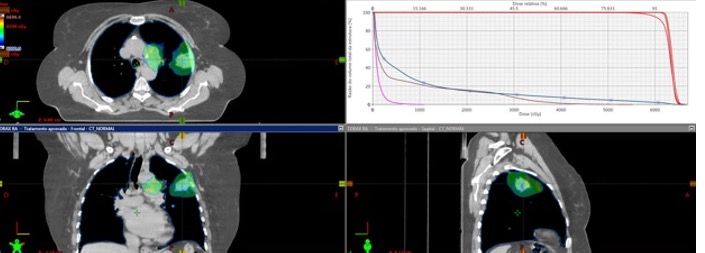
Figure 5. CT scan prior to radiochemotherapy and post radiochemotherapy.
Another important consideration is controlling immune-related AEs in patients who need long-term immunosuppression therapy. These patients must be rigorously followed because of their higher risk of infection.18 To help distinguish between COVID-19 and IMT-related pneumonitis when clinical and radiological findings are not sufficient, epidemiological data may be useful. In such cases, only a COVID-19 diagnostic test – the gold standard being the RT-PCR nasopharynx and/or oropharynx swab for SARS-CoV-2019 – will provide a definitive diagnosis of COVID-19. Considering that the humoral immune response with immunoglobulin G (IgG) antibody production happens, on average, 14 days after symptom onset, and that these antibodies can be detected up to 36 months after the infection, another reasonable option to consider when investigating the cause of pneumonitis is the quantitative analysis of serum IgG antibodies in the blood sample. In a clinical setting when a patient presents with respiratory symptoms, the presence of IgG antibodies could be evidence that the patient has already had contact with SARS-CoV-2 and that pneumonitis is probably secondary to IMT.20,21 Therefore, statement C is a correct answer.
In such a case, immediately postpone IMT and begin clinical support. IMT can be restarted as soon as the pneumonitis resolves. The early diagnosis of lung injury is fundamental to define the most appropriate treatment. For moderate IMT-induced pneumonitis, corticosteroid treatment must be started immediately, but for pneumonitis secondary to SARS-CoV-2 infection, corticosteroid treatment has shown benefit only in patients receiving concurrent oxygen therapy; it may actually be harmful in mild cases.11,22 In cases of severe pneumonitis, when the patient requires hospital admission and oxygen therapy, it is reasonable to consider starting corticosteroid treatment early; corticosteroids are indicated in severe presentation of pneumonitis regardless of the cause and, in cases of IMT-related pneumonitis, corticosteroids improve symptoms very quickly.
Figure 6. PET-CT with an excellent tumor response and appearance of ground-glass opacity.
For patients with SARS-CoV-2–related pneumonitis who are receiving IMT, the recommendation is to restart IMT treatment at least 14 days after symptom onset and only after the patient has been asymptomatic for at least 72 hours. In addition, the patient ideally should have 2 negative RT-PCR test results, 24 hours apart. However, in some localities RT-PCR kits are scarce, and in this scenario, a single negative RT-PCR test result together with clinical improvement may be enough. When it is impossible to repeat the exam, all cases must be discussed with patients, caregivers, and the medical oncologist; local recommendations should also be followed as closely as possible.11,19 Therefore, statement D is also a correct answer.
Figure 7. PET-CT with a tumor good response and resolution of almost all ground-glass opacity.
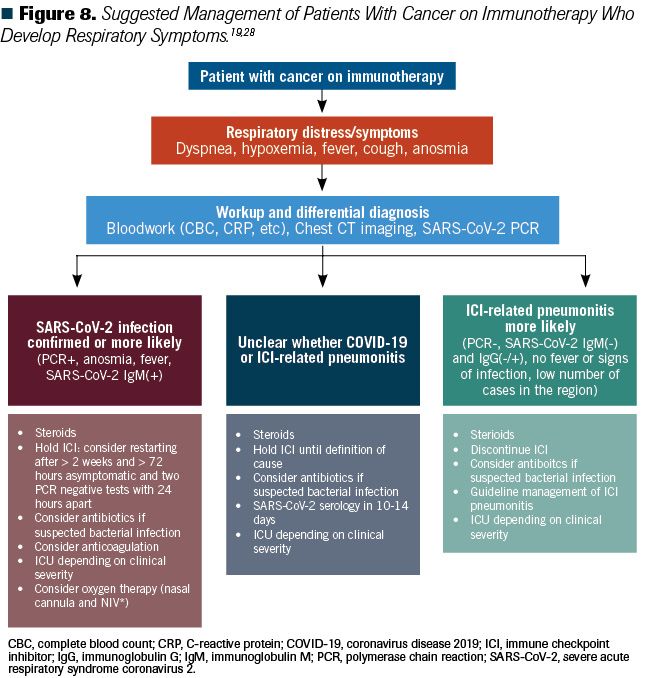
The medical oncology community had previously developed measures to minimize IMT-related pneumonitis. The American Society of Clinical Oncology19 has made new recommendations to mitigate the risk to patients with SARS-CoV-2 infection who receive oncological treatments; these include performing an RT-PCR test on all patients 48 to 72 hours before the first cycle of systemic therapy; clinical and epidemiological screening for all patients via questionnaire, 48 to 72 hours before each cycle of systemic therapy; and clinical and epidemiological evaluation when the patients arrive at the clinic and/or hospital. In symptomatic patients who are screened before arrival to the oncology unit, the current recommendation is that the patient be tested for SARS-CoV-2 outside the oncology unit. If a patient arrives at the oncology unit with COVID-19 symptoms, they must be isolated, evaluated, and tested for SARS-CoV-2. Facial masking and social distancing should be required of all patients11,19 (Figure 8).
Figure 8. Suggested Management of Patients With Cancer on Immunotherapy Who Develop Respiratory Symptoms.
Conclusions
The COVID-19 pandemic may take a long time to be controlled. Until it is, it is vital that we do not fail to recommend and maintain the appropriate treatment for patients with cancer. Educating patients, caregivers, and the health care team, and adapting oncology clinics and hospital oncology units to this new situation, is essential. Early reporting of symptoms by patients or caregivers and actively screening for symptoms by the health care team are fundamental to diagnosis and to taking the most appropriate treatment approaches.
Conflicts of interests:
Andrey Soares
Honoraria: Janssen, Pfizer, Bayer, Novartis, AstraZeneca, Astellas Pharma, Pierre Fabre, Merck Serono, Sanofi, Roche, MSD
Consulting or Advisory Role: Astellas Pharma, Janssen, Roche, Bayer, Lilly, AstraZeneca, Novartis, MSD, Bristol Myers Squibb
Research Funding: Bristol Myers Squibb (Inst)
Travel, Accommodations, Expenses: AstraZeneca, Pfizer, AstellasPharma, Bristol Myers Squibb, Bayer, Roche, Janssen, Merck Serono, Sanofi, Ipsen
Fabio A. Schutz
Honoraria: Janssen, Bayer, AstraZeneca, Astellas, Roche, MSD, Bristol-Myers Squibb, Ipsen
Consulting or Advisory Role: Astellas, Janssen, Roche, Bayer, AstraZeneca, MSD, Bristol Myers Squibb, Ipsen
Travel, Accommodations, Expenses: Bristol Myers Squibb, MSD, Janssen, Astellas Pharma
Diogo Basto
Honoraria: Janssen, Pfizer, Bayer, AstraZeneca, Astellas, Merck Serono, Roche, MSD, BMS
Consulting or Advisory Role: Astellas, Janssen, Roche, Bayer, AstraZeneca, MSD, Bristol-Myers Squibb Research Funding: Janssen, Astellas, Bayer.
Travel, Accommodations, Expenses: AstraZeneca, MSD, Bayer, Janssen
Denis Jardim
Honoraria: Janssen, Pfizer, Bayer, Novartis, AstraZeneca, Astellas Pharma, Merck Serono, Roche, MSD, Bristol Myers Squibb, Libbs
Consulting or Advi.sory Role: Janssen, Roche, AstraZeneca, MSD, Bristol Myers Squibb
Research Funding: Janssen, Bristol Myers Squibb, Roche (Inst)
Travel, Accommodations, Expenses: Bristol Myers Squibb, MSD, Janssen
Fernando Sabino M Monteiro
Honoraria: Janssen, Bayer, Bristol-Myers Squibb, Astellas Pharma, ACHE, Roche, MSD
Consulting or Advi.sory Role: Jan.ssen, Roche, MSD, Bristol-Myers Squibb
Research Funding: Janssen
Travel, Accommodations, Expenses: Bristol Myers Squibb, Roche, Janssen, MSD
About the SERIES EDITORS:
Maria T. Bourlon, MD is Associate Professor, Head Urologic Oncology Clinic, National Researcher. Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán. Mexico City, Mexico.
E. David Crawford, MD, is Chairman, Prostate Conditions Education Council; Editor in Chief, Grand Rounds in Urology; and Professor of Urology, University of California San Diego, La Jolla, California.
REFERENCES
1.COVID-19 dashboard by the Center For Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). Johns Hopkins University & Medicine Coronavirus Resource Center. Accessed August 31, 2020. https://coronavirus.jhu.edu/map.html
2.Di Cosimo S, Malfettone A, Pérez-García JM, et al. Immune checkpoint inhibitors: a physiology-driven approach to the treatment of coronavirus disease 2019. Eur J Cancer. 2020;135:62-65. doi:10.1016/j.ejca.2020.05.026
3.Bao R, Hernandez K, Huang L, Luke JJ. ACE2 and TMPRSS2 expression by clinical, HLA, immune, and microbial correlates across 34 human cancers and matched normal tissues: implications for SARS-CoV-2 COVID-19. J Immunother Cancer. 2020;8(2):e001020. doi:10.1136/jitc-2020-001020
4.Vabret N, Britton GJ, Gruber C, et al; Sinai Immunology Review Project. Immunology of COVID-19: current state of the science. Immunity. 2020;52(6):910-941. doi:10.1016/j.immuni.2020.05.002
5.Vardhana SA, Wolchok JD. The many faces of the anti-COVID immune response. J Exp Med. 2020;217(6):e20200678. doi:10.1084/jem.20200678
6.Bersanelli M. Controversies about COVID-19 and anticancer treatment with immune checkpoint inhibitors. Immunotherapy. 2020;12(5):269-273. doi:10.2217/imt-2020-0067
7.Tian J, Yuan X, Xiao J, et al. Clinical characteristics and risk factors associated with COVID-19 disease severity in patients with cancer in Wuhan, China: a multicentre, retrospective, cohort study. Lancet Oncol. 2020;21(7):893-903. doi:10.1016/ S1470-2045(20)30309-0
8.Trapani D, Marra A, Curigliano G. The experience on coronavirus disease 2019 and cancer from an oncology hub institution in Milan, Lombardy region. Eur J Cancer. 2020;132:199-206. doi:10.1016/j.ejca.2020.04.017
9.Williamson EJ, Walker AJ, Bhaskaran K, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584(7821):430-436. doi:10.1038/s41586-020-2521-4
10.Lee LY, Cazier J-B, Angelis V, et al; UK Coronavirus Monitoring Project Team. COVID-19 mortality in patients with cancer on chemotherapy or other anticancer treatments: a prospective cohort study. Lancet. 2020;395(10241):1919-1926. doi:10.1016/S0140-6736(20)31173-9. Published correction appears in Lancet. 2020;396(10250):534.
11.Naidoo J, Reuss JE, Suresh K, et al. Immune-related (IR)-pneumonitis during the COVID-19 pandemic: multidisciplinary recommendations for diagnosis and management. J Immunother Cancer. 2020;8(1):e000984. doi:10.1136/jitc-2020-000984
12.Luo J, Rizvi H, Egger JV, et al. Impact of PD-1 blockade on severity of COVID-19 in patients with lung cancers. Cancer Discov. 2020;10(8):1121-1128. doi:10.1158/2159-8290.CD-20-0596
13.Sud A, Jones ME, Broggio J, et al. Collateral damage: the impact on outcomes from cancer surgery of the COVID-19 pandemic. Ann Oncol. 2020;31(8):1065-1074. doi:10.1016/j.annonc.2020.05.009
14.Maringe C, Spicer J, Morris M, et al. The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study. Lancet Oncol. 2020;21(8):1023-1034. doi:10.1016/S1470-2045(20)30388-0
15.Kennedy LB, Salama AKS. A review of cancer immunotherapy toxicity. CA Cancer J Clin. 2020;70(2):86-104. doi:10.3322/caac.21596
16.Guerini AE, Borghetti P, Filippi AR, et al. Differential diagnosis and clinical management of a case of COVID-19 in a patient with stage III lung cancer treated with radio-chemotherapy and durvalumab. Clin Lung Cancer. Published online June 2, 2020. doi:10.1016/j.cllc.2020.05.027
17.Su Q, Zhu EC, Wu JB, et al. Risk of pneumonitis and pneumonia associated with immune checkpoint inhibitors for solid tumors: a systematic review and meta-analysis. Front Immunol. 2019;10:108. doi:10.3389/fimmu.2019.00108
18.Kattan J, Kattan C, Assi T. Do checkpoint inhibitors compromise the cancer patients’ immunity and increase the vulnerability to COVID-19 infection? Immunotherapy. 2020;12(6):351-354. doi:10.2217/imt-2020-0077
19.ASCO special report: a guide to cancer care delivery during the COVID-19 pandemic. American Society of Clinical Oncology. May 19, 2020. Accessed x x, 2020. https://www.asco.org/sites/new-www.asco.org/files/content-files/2020-ASCO-Guide-Cancer-COVID19.pdf
20.Cao W-C, Liu W, Zhang P-H, et al. Disappearance of antibodies to SARS-associated coronavirus after recovery. N Engl J Med. 2007;357(11):1162-1163. doi:10.1056/NEJMc070348
21.Siracusano G, Pastori C, Lopalco L. Humoral immune responses in COVID-19 patients: a window on the state of the art. Front Immunol. 2020;11:1049. doi:10.3389/fimmu.2020.01049
22.RECOVERY Collaborative Group; Horby P, Lim WS, Emberson JR, et al. Dexamethasone in hospitalized patients with Covid-19 – preliminary report. N Engl J Med. Published online July 17, 2020. doi:10.1056/NEJMoa2021436
23.Naidoo J, Wang X, Woo KM, et al. Pneumonitis in patients treated with anti-programmed death-1/programmed death ligand 1 therapy. J Clin Oncol. 2017;35(7):709-717. doi:10.1200/JCO.2016.68.2005. Published correction appears in J Clin Oncol. 2017;35(22):2590.
24.Cao W, Li T. COVID-19: towards understanding of pathogenesis. Cell Res. 2020;30(5):367-369. doi:10.1038/s41422-020-0327-4
25.Kalisz KR, Ramaiya NH, Laukamp KR, Gupta A. Immune checkpoint inhibitor therapy-related pneumonitis: patterns and management. Radiographics. 2019;39(7):1923-1937. doi:10.1148/rg.2019190036
26.Salehi S, Abedi A, Balakrishnan S, Gholamrezanezhad A. Coronavirus disease 2019 (COVID-19): a systematic review of imaging findings in 919 patients. AJR Am J Roentgenol. 2020;215(1):87-93. doi:10.2214/AJR.20.23034
27.Herold T, Jurinovic V, Arnreich C, et al. Elevated levels of IL-6 and CRP predict the need for mechanical ventilation in COVID-19. J Allergy Clin Immunol. 2020;146(1):128-136.e4. doi:10.1016/j.jaci.2020.05.008
28.Brahmer JR, Lacchetti C, Schneider BJ, et al; National Comprehensive Cancer Network. Management of immune-related adverse events in patients treated with immune checkpoint inhibitor therapy: American Society of Clinical Oncology clinical practice guideline. J Clin Oncol. 2018;36(17):1714-1768. doi:10.1200/JCO.2017.77.6385
Late Hepatic Recurrence From Granulosa Cell Tumor: A Case Report
Granulosa cell tumors exhibit late recurrence and rare hepatic metastasis, emphasizing the need for lifelong surveillance in affected patients.
