36 MONARCH 3: Final Overall Survival Results of Abemaciclib Plus a Nonsteroidal Aromatase Inhibitor as First-Line Therapy for HR+/HER2– Advanced Breast Cancer
Masakazu Toi
- Jens Huober, MD
- Joohyuk Sohn
- Oliver Trédan
- In Hae Park
- Mario Campone
- Shin-Cheh Chen
- Luis Manuel Manso
- Shani Paluch-Shimon
- Orit C. Freedman
- Joyce A. O’Shaughnessy
- Xavier Pivot
- Sara M. Tolaney, MD, MPH
- Sara A. Hurvitz, MD
- Antonio Llombart
- Valérie André
- Abhijoy Saha
- Gertjan van Hal
- Ashwin Shahir
- Hiroji Iwata
- Stephen R.D. Johnston
Background
Abemaciclib (abema) is approved both for high-risk early breast cancer as well as advanced breast cancer (ABC) in the first- and second-line setting. In MONARCH 3, the addition of abemaciclib to a nonsteroidal aromatase inhibitor (NSAI) significantly improved PFS (HR, 0.540; 95% CI, 0.418-0.698; P = .000002) as initial therapy in hormone receptor–positive, HER2-negative (HR+/HER2–) ABC. Here, we present the final overall survival (OS) analysis of MONARCH 3 (NCT02246621).
Methods
MONARCH 3 is a randomized, double-blind, phase 3 study of abemaciclib plus an NSAI (anastrozole or letrozole) vs placebo plus NSAI in women who are postmenopausal with HR+/HER2– ABC without prior systemic therapy in the advanced setting. OS was a gated secondary end point, and chemotherapy-free survival (CFS) was an exploratory end point. Final OS analysis was planned after about 315 OS events occurred in the intent-to-treat (ITT) population with a split α between the ITT population and the subgroup with visceral disease (sVD) according to a prespecified graphical testing scheme. Kaplan-Meier method and Cox proportional hazards models were used. Reported P values are 2-sided.
Results
OS in the ITT Population
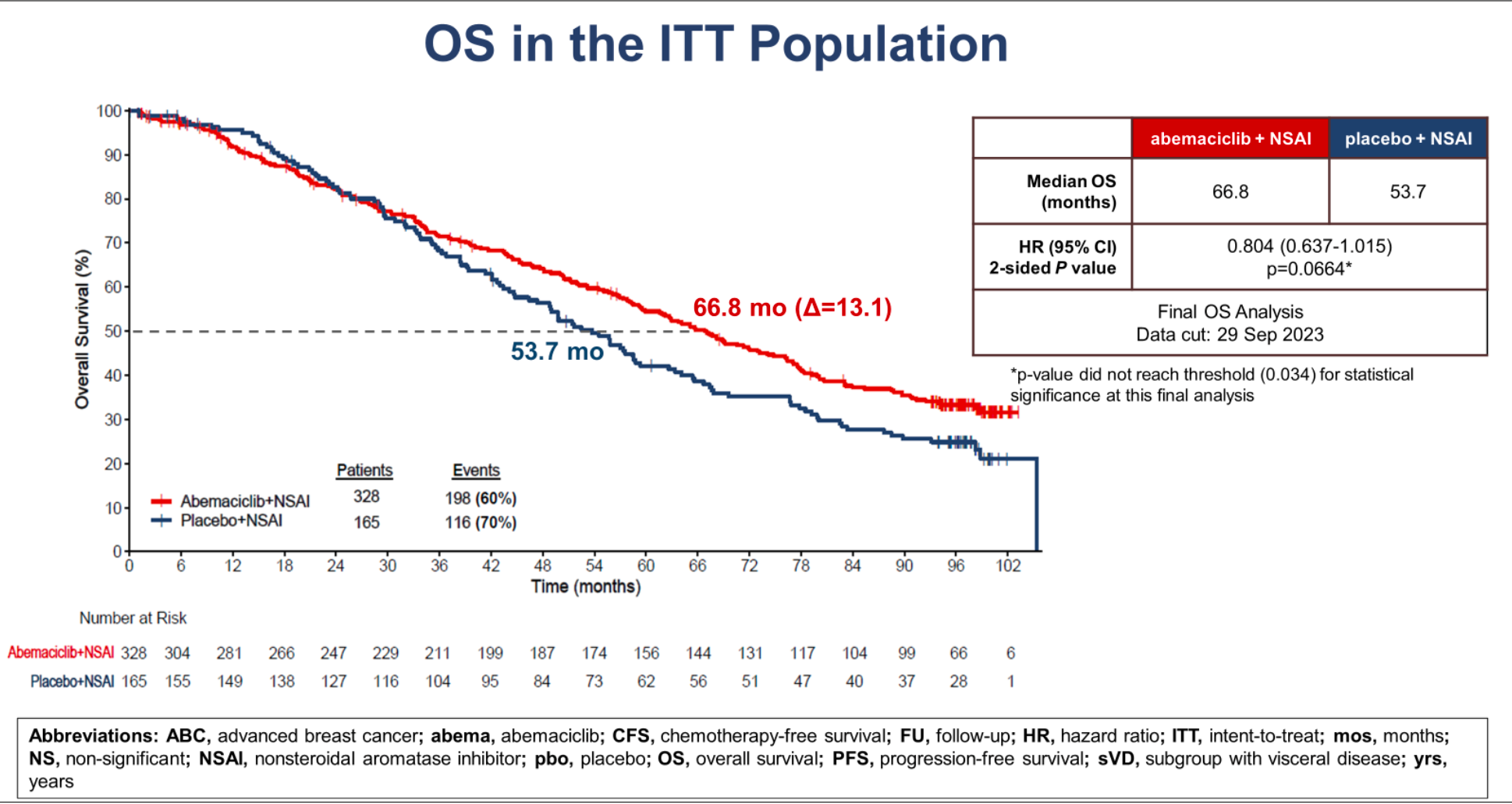
A total of 493 women were randomized 2:1 to receive abema plus an NSAI (n = 328) or placebo plus NSAI (n = 165). After a median follow-up of 8.1 years, 7% of patients were still receiving treatment in the abemaciclib arm vs 3% in the placebo arm. In the ITT population, 314 OS events were observed (198 deaths among 328 patients [60%] in the abemaciclib arm and 116 among 165 [70%] in the placebo arm) (HR, 0.804; 95% CI, 0.637-1.015; P = .0664 [not significant (NS)]). Median OS was 66.8 months in the abemaciclib arm and 53.7 months in the placebo arm (a numerical difference of 13.1 months) in the ITT population. Results were consistent in the sVD with abema vs placebo (median OS, 63.7 vs 48.8 months; HR, 0.758; 95% CI, 0.558-1.030; P = .0757 [NS]). Consistent OS differences were observed across prespecified subgroups. PFS benefit was sustained (median PFS, 29.0 vs 14.8 months; HR, 0.535; 95% CI, 0.429-0.668; nominal P <.0001). CFS was also improved with abemaciclib vs placebo (median CFS, 46.7 vs 30.6 months; HR, 0.693; 95% CI, 0.557-0.863; nominal P = .0010). No new safety signals were observed with longer-
term use.
Conclusions
In patients with HR+/HER2– ABC, abema plus NSAI resulted in numerically longer OS compared to an NSAI alone; however, statistical significance was not reached after a median follow-up of 8.1 years. The clinically meaningful improvement in median OS (> 13 months) combined with the sustained significant improvement in median PFS (> 14 months) and substantial extension in median CFS (> 16 months) continue to support the use of abema in combination with an NSAI as first-line therapy
in ABC.
