45 Neoadjuvant Chemotherapy Use in Elderly Patients
Sami Abujbarah, BA1; Heidi E. Kosiorek, MS2; Jacob B. Hammond, MD3; Patricia A. Cronin, MD4; Sarwat B. Ahmad, MD4; Brenda J. Ernst, MD5; Donald W. Northfelt, MD5; Karen S. Anderson, MD, PhD5; Barbara A. Pockaj, MD4
1Mayo Clinic Alix School of Medicine, Scottsdale, AZ.
2Department of Health Sciences Research, Mayo Clinic, Scottsdale, AZ.
3Department of Surgery, Mayo Clinic, Phoenix, AZ.
4Division of Surgical Oncology & Endocrine Surgery, Mayo Clinic, Phoenix, AZ.
5Division of Hematology/Oncology, Mayo Clinic, Phoenix, AZ.
Background
Neoadjuvant chemotherapy (NAC) is the standard of care for locally advanced breast cancer and has been shown to be most effective in the treatment of triple-negative breast cancer (TNBC) and HER2-positive breast cancer. This study characterizes the use of neoadjuvant chemotherapy in elderly patients 65 years (y) and older with early-stage breast cancer from 2005 to 2020.
Materials and Methods
Elderly patients (65 y and older) with TNBC or HER2-postive breast cancer from 2005 to 2020 at a single institution were reviewed. Univariate and multivariate analysis evaluated rates and predictive factors of neoadjuvant chemotherapy treatment use.
Results
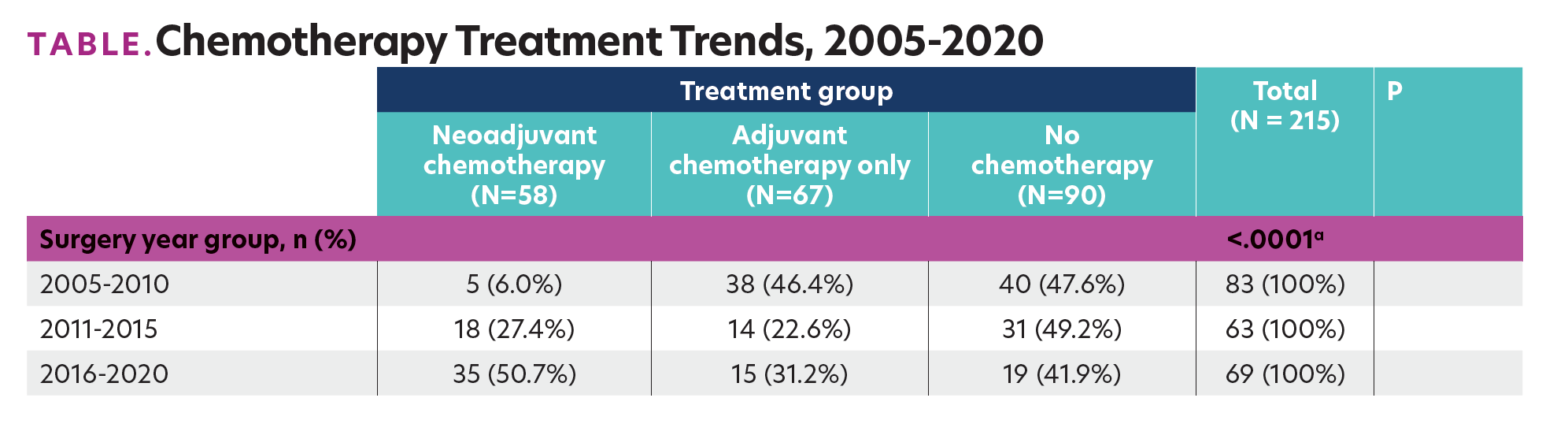
Among the 215 patients, approximately a quarter (58; 30.0%) received NAC. The mean age of those who received NAC was significantly lower (70.6 y) than of those who received only adjuvant chemotherapy (72.1 y) or no chemotherapy (76.7 y; P <.001). Those treated with NAC had a significantly larger tumor size (4.3 cm; P <.001) and a higher proportion of locally advanced and advanced stage disease (86.3%; P <.001) than those who received only adjuvant or no chemotherapy. From 2005 through 2020, the proportion of elderly patients receiving neoadjuvant chemotherapy significantly increased, from only 6% receiving NAC in 2005 through 2010, to 50.7% of patients in 2016 through 2020 (Table; P <.0001). This increase was independent of patient age and tumor stage (odds ratio [OR], 11.1; 95% CI. 3.1-39.4; P <.001 for 2011-2015 vs 2005-2010, and OR, 27.7; 95% CI, 8.1-95.3; P <.001 for 2016-2020 vs 2005-2010 reference group). Changes in the chemotherapeutic agents used also occurred over this period, with a significant decrease in the usage of anthracycline from 2005 through 2010 (18.6%) compared with 2016 through 2020 (0.0%; P <.0001). There was no significant difference in hospitalization or chemotherapy dose reduction rates in patients receiving NAC compared with those who received only adjuvant chemotherapy.
TABLE. Chemotherapy Treatment Trends, 2005-2020
Conclusions
NAC is becoming more widely used in elderly patients with HER2-postive and triple-negative tumors, independent of age and tumor stage, with no increased risk of chemotherapy complications.
Expert Commentary

