ALK-Targeted Therapy for Lung Cancer: Ready for Prime Time
Lung cancer remains the leading cause of cancer-related death in the United States. Ongoing research into the molecular basis of lung cancer has yielded insight into various critical pathways that are deregulated in lung tumorigenesis, and in particular key driver mutations integral to cancer cell survival and proliferation.
Lung cancer remains the leading cause of cancer-related death in the United States. Ongoing research into the molecular basis of lung cancer has yielded insight into various critical pathways that are deregulated in lung tumorigenesis, and in particular key driver mutations integral to cancer cell survival and proliferation. One of the most recent examples of this has been definition of translocations and functional dysregulation of the anaplastic lymphoma kinase (ALK) gene in a subset of patients with non–small-cell lung cancer. The pace of research progress in this area has been remarkable: chromosomal rearrangements involving this gene in lung cancer were first reported in 2007 by a team of investigators in Japan. Less than 3 years later, an early-phase clinical trial of a targeted ALK inhibitor has yielded impressive responses in patients with advanced lung cancer containing ALK rearrangements, and mechanisms of acquired resistance to ALK-targeted therapy are being reported. A definitive study randomizing patients with ALK-mutant lung cancer to crizotinib (also known as PF-02341066 or 1066) versus standard therapy has recently completed enrollment. Taken together, these data describe a trajectory of research progress from basic discovery science to real-world implementation that should serve as a model for future integration of preclinical and clinical therapeutic research.
FIGURE 1
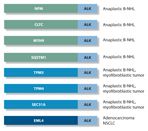
Chromosomal translocations resulting in ALK fusion genes
Anaplastic lymphoma kinase (ALK) is a member of the insulin receptor family of receptor tyrosine kinases, and is normally expressed in the central nervous system, small intestine, and testis.[1] Activating mutations or translocations of the ALK gene have been identified in several types of cancer, including anaplastic large-cell lymphoma, neuroblastoma, inflammatory myofibroblastic tumor, and, most recently, non–small-cell lung cancer (Figure 1).[2–4] The normal functions of ALK have not been fully defined. Aberrant activation of ALK in anaplastic B-cell non-Hodgkin’s lymphoma is due to chromosomal translocation of ALK to create a fusion gene with partners such as nucleoplasmin (NPM).[5,6] ALK cancer-associated fusion genes preserve the C-terminal kinase domain of ALK, and juxtapose this in frame with upstream components of the partner gene (Figure 1).[5] Less commonly, activating mutations of ALK in the absence of chromosomal translocation and gene fusion have been reported. A recent and seminal discovery extended these observations to include lung cancer. In a subset of lung adenocarcinomas, genetic translocation of two genes in the short arm of chromosome 2 leads to the expression of the fusion protein between the N-terminal portion of echinoderm microtubule-associated protein-like 4 (EML4) and the C-terminal kinase domain of ALK.[7] This leads to constitutive, ligand-independent activation of the ALK kinase, resulting in aberrant activation of downstream oncogenic signaling pathways including MAP kinase–, PI3 kinase–, and STAT3-dependent pathways that promote cell proliferation, stromal invasion, and apoptotic inhibition.[8]
Detection of ALK Translocation in Lung Cancer
ALK translocations in non–small-cell lung cancer (NSCLC) were first detected by transfection of a cDNA expression library from an NSCLC tumor into 3T3 fibroblasts, resulting in selective transformation.[7] In the initial report, 5 of 75 Japanese NSCLC tumor samples of unselected histologic subtype contained an EML4-ALK gene fusion.[9]The presence of EML4-ALK translocation in general appears to be mutually exclusive of mutations in other known driver mutations, including epidermal growth factor receptor (EGFR) and KRAS, although counterexamples have been recently reported.[10,11] Shaw et al studied the prevalence of tumor-specific ALK rearrangements and reported association with clinical characteristics including female sex, Asian ethnicity, light or never smoking history, and adenocarcinoma histology.[11] ALK translocations were identified in 19 of 141 tumors (13%) and, in this report, were mutually exclusive of activating EGFR mutation. In unselected populations of patients with NSCLC, the frequency of ALK translocation appears to be in the range of 2%–7%. ALK-mutated tumors are more likely to demonstrate a "signet ring cell" histologic morphology, are more prevalent in younger lung cancer patients, and are less strongly sex-associated than EGFR mutations, which are more common in women.[12] Several reproducible detection methods for ALK tyrosine kinase rearrangement have been developed and validated, including break-apart fluorescence in situ hybridization (FISH) to detect chromosomal translocation, multiplexed RT-PCR (reverse transcriptase polymerase chain reaction) to detect the fusion transcript, or immunohistochemistry using antibodies to detect aberrant ALK protein expression.[13]
Reported Activity of Crizotinib
Investigators promptly began to evaluate whether ALK inhibition may have a role in this selected population. Crizotinib (also known as PF-02341066 or 1066), initially launched as an inhibitor of the MET tyrosine kinase, also had anti-ALK activity.[14] The phase I trial of crizotinib had started in May 2006, before the demonstration of ALK gene rearrangements in NSCLC, and without molecular selection tested six different doses of drug in patients with various advanced malignancies.[14] In preclinical studies involving more than 600 cell lines derived from human cancers, crizotinib had specifically reduced the proliferation of cells carrying genetic alterations in ALK.[6] Crizotinib inhibits phosphorylation of activated ALK at nanomolar concentrations.[14] The maximum tolerated dose was identified to be 250-mg twice daily, as the 300-mg twice-daily dose was associated with two cases of grade 3 fatigue. Following observation of impressive activity of crizotinib in some patients with ALK-positive NSCLC, investigation of an expanded molecularly enriched cohort was conducted.[15]
FIGURE 2
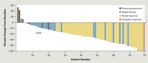
Waterfall plot showing response to crizotinib in patients with
EML4-ALK
NSCLC
After screening 1,500 patients with NSCLC for the presence of ALK rearrangements, the investigators identified 82 patients with ALK-rearranged advanced NSCLC who were eligible for study.[15] Key eligibility requirements included good performance status (most ECOG 0–1), ALK positivity on fluorescence in situ hybridization (FISH), and measurable disease. No limit was placed on the number of previous treatment regimens that a patient received. At a mean treatment duration of 6.4 months, the overall response rate to crizotinib was 57% (46 confirmed partial responses and 1 confirmed complete response) in this cohort of 82 patients; 27 patients (33%) had stable disease. A waterfall plot of tumor reduction provides a snapshot of the impressive activity of this drug in this select patient population (Figure 2). A total of 63 of 82 patients (77%) continued to receive crizotinib at the time of data cutoff, and the estimated probability of 6-month progression-free survival (PFS) was 72%. A median PFS was not reached at the time of study reporting. More than 90% of the patients in the phase I study received crizotinib as second-line therapy.[15] These exciting findings clearly compare favorably with historical data in NSCLC; a recent meta-analysis of clinical outcome following second-line therapy demonstrated a 6-month PFS rate of 27.2% in historical controls.[16]
Safety data from the 82 patients, treated primarily in the 250-mg twice-daily expansion cohort, suggested that crizotinib was well tolerated.[15] Grade 1 nausea and diarrhea were the most commonly reported side effects. Mild visual disturbances reported by 34 patients (41%) were most frequently described as trails of light following objects moving relative to the observer. Increases in levels of hepatic transaminases were observed and generally grade 1 or 2. Grade 3 elevations in alanine aminotransferase (ALT) and aspartate aminotransferase (AST) were observed in four patients (5%) and five patients (6%) respectively, usually with onset during cycle 2. These increases reversed on cessation of crizotinib, and four of five patients with elevated transaminase levels were able to resume treatment at a lower dose without recurrence of dose-imiting toxicities.
Not all patients with EML4-ALK translocated NSCLC had dramatic benefit from crizotinib. Of the 82 patients, 6 (7%) had disease progression at the time of their first staging scans. Two patients had an increase of more than 20% in disease burden after two cycles of therapy. Three patients had stable disease in target lesions but concurrently developed new lesions consistent with progressive disease. One patient had tumor regression of 25% on the basis of early CT scanning during cycle 1 but subsequently had an increase in tumor burden of more than 20% at the time of protocol-specified staging.[15] The mechanisms for primary resistance in this subset of patients have not been defined, but they are the subject of ongoing research in several groups.[17]
Because crizotinib also inhibits the MET receptor tyrosine kinase, tumors from 33 patients with available tissue were tested for MET amplification. No samples were MET amplified, arguing against inhibition of MET as a primary determinant of response in these patients. None of the patients with ALK rearrangement had a concurrent mutation in EGFR, even though these patients shared several key clinical and demographic features of patients with EGFR mutations.[15]
Ongoing Clinical Research and Future Directions
TABLE 1

Selected Small Moleculte Inhibitors of ALK
Based on these highly promising results, a randomized phase III trial was initiated, PROFILE 1007 (Clinical Trials.gov identifier: NCT00932893).[14] This study compares crizotinib against standard of care in 318 patients with advanced NSCLC and an alteration of the ALK gene who have failed to respond to one prior treatment with a platinum-based chemotherapy. The primary endpoint of this trial is PFS. Patients in the experimental arm receive crizotinib at a dosage of 250-mg twice daily on a continuous schedule, whereas patients assigned to the control arm receive either pemetrexed (Alimta) or docetaxel at standard doses and schedules. Given the promising activity of crizotinib reported in the expansion cohort of the initial phase I study, a second partner study was designed to allow crizotinib access to patients with ALK-translocated NSCLC who did not meet enrollment criteria for the phase III study. This companion study also allows enrollment of patients with progressive disease on the phase III study who were assigned to the control arm of standard chemotherapy (Clinical Trials.gov Identifier NCT00932451). A second phase III trial, testing the efficacy of crizotinib as first-line treatment for metastatic NSCLC demonstrating ALK translocation, has been recently launched. This study will randomize eligible patients to crizotinib versus pemetrexed/cisplatin or pemetrexed/carboplatin. Following rapidly on the heels of these studies, a number of preclinical or early-phase clinical investigations have reported activity of small-molecule TKIs against ALK (Table 1).[18]
REFERENCE GUIDE
Therapeutic Agents
Mentioned in This Article
Carboplatin
Cisplatin
Crizotinib (PF-02341066 or 1066)
Docetaxel
IPI-504
Pemetrexed (Alimta)
Brand names are listed in parentheses only if a drug is not available generically and is marketed as no more than two trademarked or registered products. More familiar alternative generic designations may also be included parenthetically.
In conjunction with a current focus on other targeted inhibitors of driver mutations in cancer, researchers are actively working to address the issue of primary and acquired resistance to crizotinib in ALK-mutant NSCLC. The pace of research in this domain has also been impressive. Most notably, Choi et al recently characterized two distinct secondary mutations in the kinase domain of the EML4-ALK fusion transgene in NSCLC tumor material derived from a patient demonstrating progressive disease on crizotinib. Both of these mutations were associated with resistance not only to crizotinib, but also to other targeted ALK inhibitors.[17] Interestingly, a recent phase I study of a heat shock protein 90 inhibitor (IPI-504) included a small number of patients with EML4-ALK translocated NSCLC, with responses following progression on crizotinib.[19] A phase II study of IPI-504 in this patient population is ongoing.
Understanding the tumor cell dependence on ALK signaling in ALK-mutant NSCLC, defining key downstream signaling pathways and mechanisms of both primary resistance and secondary acquired resistance, and identifying optimal combination therapies involving ALK inhibitors, all will be active areas of investigation with clear and relatively immediate clinical relevance. This is an area of clinical translation now operating at hyperspeed: fasten your seatbelts and stay tuned.
Financial Disclosure:The authors have no significant financial interest or other relationship with the manufacturers of any products or providers of any service mentioned in this article.
References:
References
1. Pulford K, Lamant L, Espinos E, et al. The emerging normal and disease-related roles of anaplastic lymphoma kinase. Cell Mol Life Sci. 2004;61:2939-53.
2. Kutok JL, Aster JC. Molecular biology of anaplastic lymphoma kinase-positive anaplastic large-cell lymphoma. J ClinOncol. 2002;20:3691 702.
3. George RE, Sanda T, Hanna M, et al. Activating mutations in ALK provide atherapeutic target in neuroblastoma. Nature. 2008;455:975-8.
4. Mossé YP, Laudenslager M, Longo L, et al. Identification of ALK as a major familial neuroblastoma predisposition gene. Nature. 2008;455:930-5.
5. Morris SW, Kirstein MN, Valentine MB, et al. Fusion of a kinase gene, ALK, to a nucleolar protein gene NPM, in non-Hodgkin’s lymphoma. Science. 1994; 263:1281-4.
6. Morris SW, Naeve C, Matthew P, et al. ALK, the chromosome 2 gene locus altered by the t(2;5) in non-Hodgkins lymphoma, encodes a novel neural receptor tyrosine kinase that is highly related to leukocyte tyrosine kinase (LTK). Oncogene. 1997;14:2175-88.
7. Soda M, Choi YL, Enomoto M, et al. Identification of the transforming EML4-ALK fusion gene in non-small cell lung cancer. Nature. 2007;448:561-6.
8. Amin HM, Lai R. Pathobiology of ALK+ anaplastic large cell lymphoma. Blood. 2007;110:2259-67.
9. Choi YL, Takeuchi K, Soda M, et al. Identification of novel isoforms of the EML4-ALK transforming gene in non-small cell lung cancer. Cancer Res. 2008;68:4971-6.
10. Tiseo M, Gelsomino F, Boggiani D, et al. EGFR and EML4-ALK mutations in NSCLC: a case report of erlotinib-resistant patient with both concomitant mutations. Lung Cancer. 2011;71:241-3.
11. Shaw AT, Yeap BY, Mino-Kenudson M, et al. Clinical features and outcome of patients with non-small cell lung cancer who harbor EML4-ALK. J Clin Oncol. 2009;27:4247-53.
12. Rodig SJ, Mino-Kenudson M, Dacic S, et al. Unique clinicopathologic features characterize ALK-rearranged lung adenocarcinoma in the Western populations. Clin Cancer Res. 2009;15:5216-23.
13. Mino-Kenudson M, Chirieac LR, Law K, et al. A novel highly sensitive antibody allows for the routine detection of ALK-rearranged lung adenocarcinomas by standard immunohistochemistry. Clin Cancer Res. 2010;16:1561-71.
14. Christensen JG, Zou HY, Arango ME, et al. Cytoreductive antitumor activity of PF-2341066, a novel inhibitor of anaplastic lymphoma kinase and c-Met, in experimental models of anaplastic large cell lymphoma. Mol Cancer Ther. 2007;3314-22.
15. Kwak EL, Bang Y-J, Camidge R, et al. Anaplastic lymphoma kinase inhibition in non-small cell lung cancer. N Engl J Med. 2010;363:1693-1703.
16. Di Maio M, Chiodini P, Georgoulias V, et al. Meta-analysis of single agent chemotherapy compared with combination chemotherapy as second line treatment for advanced non-small cell lung cancer. J Clin Oncol. 2009;27:1836-43.
17. Choi YL, Soda M, Tanio Y, et al. EML4-ALK mutations in lung cancer that confer resistance to ALK inhibitors. N Engl J Med. 2010;363:1734-9.
18. Lovly CM, Heuckmann JM, de Stanchina E, et al. Insights into ALK-driven cancers revealed through development of novel ALK tyrosine kinase inhibitors. Cancer Res. 2011; May 25 [Epub ahead of print]
19. Normant E, Paez G, West KA, et al. The HSP90 inhibitor IPI-504 rapidly lowers EML4-ALK levels and induces tumor regression in ALK-driven NSCLC models. Oncogene. 2011;Jan 24 [Epub ahead of print]