Proton Therapy for Prostate Cancer
This review discusses the rationale, history, and current status of proton therapy for prostate cancer-and controversies regarding it.
Proton therapy has been used in the treatment of cancer for over 50 years. Due to its unique dose distribution with its spread-out Bragg peak, proton therapy can deliver highly conformal radiation to cancers located adjacent to critical normal structures. One of the important applications of its use is in prostate cancer, since the prostate is located adjacent to the rectum and bladder. Over 30 years of data have been published on the use of proton therapy in prostate cancer; these data have demonstrated high rates of local and biochemical control as well as low rates of urinary and rectal toxicity. Although before 2000 proton therapy was available at only a couple of centers in the United States, several new proton centers have been built in the last decade. With the increased availability of proton therapy, research on its use for prostate cancer has accelerated rapidly. Current research includes explorations of dose escalation, hypofractionation, and patient-reported quality-of-life outcomes. Early results from these studies are promising and will likely help make proton therapy for the treatment of prostate cancer more cost-effective.
Introduction
Proton therapy (PT) has been used in the management of cancer for over 50 years. The unique pattern of radiation dose deposition associated with protons-the characteristic spread-out Bragg peak (SOBP)-was recognized as early as the 1950s as a tool that radiation oncologists could use to deliver highly conformal radiotherapy to cancers located adjacent to critical organs. Until 1991, PT was only available at physics research centers; these facilities typically offered relatively low-energy protons delivered through a fixed beam, so clinical applications were limited. The prostate, with its close proximity to the rectum, bowel, and bladder, was recognized early on as an ideal site for the application of PT. At the Massachusetts General Hospital in Boston, PT was used as a “boost” to conventional radiation therapy in prostate cancer as early as the late 1970s.[1] The first clinically dedicated facility opened at Loma Linda University in Loma Linda, California in 1991, complete with sufficiently high-energy protons to penetrate to central tumors, with a gantry system to deliver PT from any angle, and offering treatment of prostate cancer solely with PT. Early results of PT from these two institutions have been promising, leading to a burgeoning interest in PT for prostate cancer at other institutions that have acquired PT. While there is much theoretical and early clinical promise, many questions remain regarding the degree of potential benefit and the cost-effectiveness of PT in prostate cancer. This review discusses the rationale, history, and current status of PT for prostate cancer-and controversies regarding it.
Rationale: The Physics of Proton Therapy and X-Ray Therapy
The patterns of radiation dose deposition in tissue associated with PT and X-ray therapy (XRT) differ significantly. With XRT, most X-rays pass through the patient, depositing radiation energy along the beam path and leaving a track of radiation damage, much like that left by a bullet, from the skin surface through which the beam enters to the skin surface through which it exits. Because the X-rays in these interactions are absorbed, the dose deposited along the beam path is reduced gradually as the X-ray beam passes through the patient. Since radiation damage is proportional to dose and not specific to cancer cells, this pattern of dose deposition with X-rays delivers more dose to nontargeted normal tissue. This unnecessary dose to the nontargeted normal tissue contributes considerably to the “integral dose” (dose deposited in the entire patient body).
Historically, there have been two basic strategies for dealing with the problem of integral dose with X-rays: 1) the use of higher-energy X-rays, which reduces the dose to normal tissues within the first few centimeters of the entrance path, and 2) the use of additional X-ray beams whose paths overlap only over the targeted tumor, which increases the dose to the cancer relative to the dose to any particular section of normal nontargeted tissue, at the expense of exposing more normal tissue to low doses of radiation. This second strategy is the basis for three-dimensional conformal radiation therapy (3DCRT), stereotactic radiosurgery and stereotactic body radiation therapy (SBRT), Cyberknife, intensity-modulated radiation therapy (IMRT), image-guided IMRT, and volumetric modulated arc therapy.
Most XRT for prostate cancer is delivered with an IMRT technique. IMRT is a sophisticated XRT technique that employs multiple radiation beams aimed at the target from different directions, with the beams varying in size and shape during treatment delivery to create a highly conformal radiation dose distribution in which the volume of tissue receiving a “high” dose of radiation conforms precisely to the three-dimensional (3D) volume of the target. This technique is a significant improvement over simpler, conventional radiation therapy techniques used historically, which deliver a high radiation dose to a volume of tissue that is much larger and less conformal-and that thus includes substantially more normal tissue. However, because of the increased number of X-ray beams used with IMRT, a much larger volume of non-targeted tissue receives low radiation doses than is the case with the simpler conventional radiation therapy techniques. With IMRT, as in other XRT techniques based on overlapping beams, integral dose is redistributed over a larger volume of nontargeted tissue compared with simpler historical techniques, but it is not reduced.
In contrast to X-rays, protons have mass and thus do not travel an infinite distance; rather, they stop in tissue at a distance proportional to their acceleration. In addition, protons are 1,800 times as heavy as electrons, the primary subatomic particles with which they collide. Unlike X-rays, which are absorbed in these interactions, protons lose relatively little energy along the beam path until the end of their range, at which point they lose the majority of their energy, producing a characteristic sharp peak in radiation energy deposition known as the Bragg peak. Thus, a typical proton beam disperses a low constant dose of radiation along the entrance path of the beam, a high uniform dose throughout the range of the SOBP, and no exit dose, eliminating much of the integral dose inherent in X-ray therapy. In contrast to XRT, the majority of radiation energy from a proton beam is actually deposited in the targeted cancer. Because the width of the Bragg peak is only 4 to 7 mm, in actual clinical practice, an SOBP is produced by adding a series of proton beams with appropriate energies to cover the full thickness of a particular target with a uniform dose.
FIGURE 1

A Comparison of Typical Radiation Dose Distributions Achieved With PT and IMRT for a Patient With Low-Risk Prostate CancerFIGURE 2
Dose-Volume Comparison of Intensity-Modulated Radiotherapy (IMRT) and Proton Therapy in Patients with Prostate Cancer
Figure 1 is a comparison of typical radiation dose distributions achieved with PT and IMRT for a patient with low-risk prostate cancer. The relative radiation dose levels are indicated by the color wash, with red representing the highest radiation doses and blue indicating the lowest doses. As is apparent, there is a higher integral dose with IMRT compared with PT; with PT, a much larger proportion of the rectum receives either no radiation dose or only a very small dose. Figure 2 shows a comparison of dose-volume histograms for the rectum and bladder with the PT and IMRT treatment plans. The x-axis charts radiation dose and the y-axis charts the percentage of organ receiving the corresponding dose. Due to the proximity of the anterior wall of the rectum and the base of the bladder to the prostate, the volumes of these organs receiving high radiation doses are similar for the IMRT and PT plans. However, there are significant differences in the volumes of bladder and rectum receiving medium- and low-dose radiation in the PT plan compared with the IMRT plan.[2] It should be noted that proton therapy for prostate treatments is typically delivered using two lateral or slightly lateral oblique beams, taking full advantage of the ability of protons to stop before the contralateral femoral heads. Proton beams at such large depths do not necessasrily possess an advantage of reduced beam penumbra compared with IMRT treatments, as pointed out by Goitein.[3] However, the ability of proton prostate therapy to avoid beam entrance and exit through bladder and rectum allows maximum sparing of these critical organs, such that large percentages of these volumes receive essentially no dose. At the same time, the robustness of such beam arrangements has been shown to be adequate for intra-fraction prostate movements up to 5 mm.[4] Given the growing body of literature demonstrating an association between gastrointestinal (GI) and genitourinary (GU) complications with dose-volume histograms of the rectum and bladder, including the volumes receiving low and moderates doses, the reduction in integral dose to these structures with PT will likely translate into fewer GU and GI toxicities.[5,6]
Along with the lower dose to the rectum and bladder, the lower integral radiation dose with PT compared with XRT may result in other benefits to patients with prostate cancer. The relationship between the volume of tissue exposed to low radiation doses and secondary malignancies has been established in pediatric cancers.[7,8] Fontenot et al[9] of the MD Anderson Cancer Center in Houston have evaluated the risk of secondary malignancies with IMRT compared with PT in patients with early-stage prostate cancer and have shown that PT should reduce the risk of secondary malignancies by 26% to 39% compared with IMRT. Due to concerns regarding urinary incontinence and erectile dysfunction with surgery, the use of radiotherapy in younger men with prostate cancer has increased. Particularly in these younger patients with prostate cancer, PT may result in a measurably lower rate of secondary malignancy than is seen with IMRT.
Integral dose may affect other organs located close to the treatment field. Some investigators have suggested that the low-dose scatter radiation to the testes from 3DCRT, IMRT, and SBRT may reduce testosterone levels.[10-12] However, in a study from the University of Florida Proton Therapy Institute in Jacksonville, PT had no significant effect on testosterone levels in patients during the first 2 years of follow-up.[13] It is possible that preserving testosterone levels may result in preservation of libido and prevention of fatigue following treatment. Doses to the penile bulb may be less with PT than with IMRT, which may also help preserve erectile function after radiation therapy. Not all structures, however, receive less integral dose with PT than with XRT. In a study from Massachusetts General Hospital,[14] Trofimov demonstrated higher doses to the femoral neck with PT. This has led to some concern regarding the possibility of an increased risk of femoral neck fractures in patients treated with PT.[15] In an analysis from the University of Florida Proton Therapy Institute with a median follow-up of 2 years, no increased risk in hip fracture was observed among 400 consecutive men treated with PT compared with the number of fractures expected in this population, based on patient comorbidities and as determined by the World Health Organization FRAX tool for assessing hip fracture risk.[16]
The History of Proton Therapy in Prostate Cancer
Proton therapy as a conformal boost after conventional radiation therapy
Prior to 3D imaging and 3DCRT, radiation doses for prostate cancer were limited to 70 Gy or less because of the morbidity associated with high integral doses to large volumes of the bladder and rectum.[17-19] During this era, surgery was the preferred treatment for prostate cancer because of relatively high probabilities of tumor recurrence with radiation as well as high morbidity rates.[18,20] PT was available only in physics research centers, which provided a beam of protons emanating from a fixed beam line, generally of limited energies insufficient for penetration to deep-seated tumors. The initial studies of PT in prostate cancer came from Massachusetts General Hospital and used a 160-MeV proton beam from the Harvard cyclotron. In their first published study, Shipley et al reported on 17 patients treated with conventional megavoltage X-rays to between 48 and 50 Gy followed by a proton boost applied through a perineal field to a final dose of 70 to 76.5 Gy/CGE.[1] Although one patient relapsed 18 months after therapy, the remaining patients did well. A follow-up study by the Massachusetts General Hospital group[21] compared two cohorts of patients: one treated with megavoltage X-rays alone to 67 Gy and the other treated with 50 Gy of XRT followed by a proton boost of 20 to 26.5 CGE. Despite higher doses in the PT cohort, no significant difference was found regarding GU or GI toxicity between the two groups. Following the phase I/II study, Massachusetts General Hospital conducted the first phase III PT study randomly assigning patients with stage T3-4 prostate cancer to treatment with either high-dose radiation with 75.6 CGE (via 50.4 Gy X-rays and 25.2-CGE proton boost; n = 103) or with 67.2 Gy X-rays (n = 99).[22] After a median follow-up of 5 years, no significant differences were found in overall survival or disease-specific survival. However, patients with poorly differentiated prostate cancer (Gleason score ≥ 7) had better local control (LC) with high-dose radiotherapy (5-year LC, 94% vs 64%; P = .0014). Also, there was a trend toward improved LC with high-dose radiation for the cohort as a whole (5-year LC, 92% vs 80%; P = .089), and GU and GI toxicity were not significantly different.
FIGURE 3
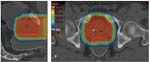
Sagittal (A) and Transverse (B) colorwash of a typical perineal proton boost
Proton therapy as sole treatment for prostate cancer
In 1991, Loma Linda University Medical Center opened the first clinically dedicated PT facility with higher-energy (250-MeV) protons and a gantry system similar to those available for conventional XRT, thereby permitting PT delivery to deep-seated tumors and from any angle. Loma Linda University conducted a phase I/II study using a higher-energy proton beam that allowed the delivery of PT via lateral fields through the hip, instead of the perineal approach used at Massachusetts General Hospital (Figure 3). The study included 104 patients treated with 45 Gy of X-rays and a 30-CGE boost with PT.[23] With a median follow-up of 20 months, no grade 3 or 4 morbidity was observed and only 12% of patients had a grade 1 or 2 late morbidity (8% rectal and 4% urinary). Two-year local disease control rates were encouraging, with only 2.8% developing progression. In a follow-up report on 319 patients (median follow-up, 43 months) who were treated with PT to 74 to 75 CGE either as a boost following conventional radiation therapy (n = 93) or as sole treatment (n = 226), the 5-year biochemical failure–free survival (BFFS) in the entire cohort was 88%, with no Radiation Therapy Oncology Group (RTOG) grade 3 or 4 GU or GI toxicities.[24] Importantly, this was the first study to report long-term outcomes of patients who were treated solely with PT. In the most recent update of the Loma Linda University experience, Slater et al[25] reported on 1,255 patients (median follow-up, 63 months) who were treated either with protons alone (n = 524) or with a proton boost (n = 731) to total doses of 74 to 75 CGE; 5-year BFFS was 75%, and the rate of late grade 3+ GU or GI toxicities was < 1%.
Proton therapy as a means for dose escalation: Proton Radiation Oncology Group trial 95-09
Considering the promising data emerging from Massachusetts General Hospital and Loma Linda University, a collaboration called Proton Radiation Oncology Group (PROG) developed between the two institutions, supported by the American College of Radiology (ACR). The first trial, PROG 95-05, conducted from 1996 to 1999, randomly assigned 393 men with T1b-2b prostate cancer and a prostate-specific antigen (PSA) level < 15 ng/mL to receive treatment with either low-dose (70.2 Gy/CGE) or high-dose (79.2 Gy/CGE) radiation. The radiation was comprised of a proton “boost” with either 19.8 CGE or 28.8 CGE via opposed lateral 250-mV proton beams at Loma Linda University or via a single en-face 160-mV proton beam through the perineum at Massachusetts General Hospital, followed by 50.4 Gy with 3DCRT. The goal of the study was not to compare protons with X-rays, but to determine whether dose escalation with PT would improve outcomes. In the first outcome report, which had a median follow-up of 5.5 years, Zietman et al[26] reported a statistically significant improvement in 5-year BFFS in the high-dose arm of 80.4% compared with 61.4% in the low-dose arm. Although the study appeared to be positive, demonstrating the feasibility of dose escalation with PT and improved disease control with dose escalation, critics of the study pointed out that both treatment arms did rather poorly compared with other contemporary studies of radiation therapy in prostate cancer. On re-evaluation of the data, Zietman et al[27] identified a considerable statistical error in the initial report. The updated outcomes demonstrated a 5-year BFFS of 91.3% with high-dose therapy compared with 78.8% for low-dose therapy (P < .001), which translated to a 59% reduction in the risk of failure. These BFFS rates were much higher than in the initial evaluation, and similar to those in other published studies. In the most recent update,[28] the group reported 10-year BFFS rates of 83.3% and 67.6% for high-dose and low-dose radiotherapy, respectively. The BFFS in patients with low-risk disease was 93% at 10 years. Importantly, the study demonstrated extremely low rates of grade > 3 GU (2%) and GI (1%) toxicity, even in the high-dose arm.
Contemporary Proton Therapy for Prostate Cancer
Over the last decade, more proton centers have been built in the United States and abroad. PT for prostate cancer has been investigated at these newer centers using treatment guidelines similar to those used at Loma Linda University, with PT for the entire course of treatment to maximize the dosimetric benefit of PT over X-ray radiation.
TABLE

Review of the Literature on Proton Therapy for Prostate Cancer
The University of Florida Proton Therapy Institute recently reported the early outcomes of 211 patients enrolled in one of three treatment protocols, including a low-risk protocol delivering 78 CGE at 2 CGE per fraction, an intermediate-risk protocol of dose escalation from 78 CGE to 82 CGE at 2 CGE per fraction, and a high-risk protocol of 78 CGE at 2 CGE per fraction with concomitant docetaxel (Taxotere) followed by androgen deprivation therapy.[6] With a minimum follow-up of 2 years, the grade > 3 GU toxicity rate was 1.9% and the grade > 3 GI toxicity rate was < 0.5%. Two studies out of Japan have also published early outcomes for PT for prostate cancer. Mayahara et al[29] reported on 287 patients treated to 74 CGE with 190- to 230-MeV protons using opposed lateral fields; the rate of grade > 3 GU toxicity in this study was 1%, and the rate of grade > 3 GI toxicity was 0%. Nihei et al[30] reported on a multi-institutional phase II study from Japan in which 74 CGE was delivered in 37 fractions in 151 patients. With a median follow-up of 43 months, only 1% of patients developed grade > 3 GU toxicity, and 0% developed late grade > 3 GI toxicity. These studies, which are reported in the Table, confirm the safety of PT for prostate cancer over the first 4 years following treatment; however, longer follow-up is needed to confirm the low rate of late toxicity and long-term efficacy of the treatment (and the high rate of BFFS). Interestingly, Massachusetts General Hospital and Loma Linda University have reported a smaller series of patients treated with PT alone to 82 CGE, with a slightly higher rate of toxicity than observed in the University of Florida Proton Therapy Institute series with the same dose and dose per fraction.[31]
Cost-Effectiveness of Proton Therapy
Although the benefits to patients of reduced radiation-dose exposure with PT are quite obvious, concerns still exist regarding whether these dosimetric benefits are cost-effective. In a study by Konski et al,[32] the cost-effectiveness of PT was compared to that of IMRT with the assumption that PT could deliver a 10-Gy higher dose than IMRT, resulting in a 10% improvement in 5-year BFFS compared with IMRT. However, despite the improvement in BFFS, the resulting cost of PT for a 60-year-old man was $65,000, compared with $40,000 for IMRT, which would result in a cost-effectiveness of $56,000 per quality-adjusted life year (QALY). When compared to the commonly accepted standard of $50,000 per QALY, the value for PT indicated that it was not cost-effective. Although this study reaches some intriguing conclusions, the results are based on models and do not take into consideration a number of critical factors. First, Peeters et al[33] have predicted that PT may allow for hypofractionation, which would reduce the treatment costs of this therapy. Studies currently investigating hypofractionation with PT are ongoing at both Loma Linda University and the University of Florida Proton Therapy Institute. Second, a reduction in significant rectal and urinary toxicity afforded by PT will have a positive impact on overall costs of care in prostate cancer patients. Finally, the dose escalation and dose intensification via hypofractionation permitted by PT may result in increased cure rates, particularly in intermediate- and high-risk prostate cancer patients,[34] which may also translate into reduced costs of care.
REFERENCE GUIDE
Therapeutic Agents
Mentioned in This Article
Docetaxel (Taxotere)
Brand names are listed in parentheses only if a drug is not available generically and is marketed as no more than two trademarked or registered products. More familiar alternative generic designations may also be included parenthetically.
A Randomized Study Comparing Photons and Protons?
There has already been a great deal of discussion in the literature regarding the feasibility of a randomized study comparing PT and IMRT for prostate cancer, which is an issue beyond the scope of this review.[35-38] It is unclear how much dose escalation and dose intensification the improved dose distribution from PT will permit. Thus, at this point in time, the degree of benefit achievable with PT is unknown, so it seems premature to commit significant resources to a randomized trial testing a mature technology against an immature technology. Funds and research resources would be better spent at this point in developing PT and in determining how best to maximize its benefits.
Conclusions
PT is a promising treatment option for prostate cancer patients. Studies have already demonstrated extremely low rates of grade > 3 GU and GI toxicities and extremely high disease control, presumably related to improved radiation dose distributions over what can be achieved with IMRT. More follow-up is needed to confirm the promising early results. A reduction in the integral dose to the body with PT compared to XRT may have other important implications in the future, including a decrease in secondary-malignancy risks.
Financial Disclosure:The authors have no significant financial interest or other relationship with the manufacturers of any products or providers of any service mentioned in this article.
References:
References:
1. Shipley WU, Tepper JE, Prout GR, Jr, et al. Proton radiation as boost therapy for localized prostatic carcinoma. JAMA. 1979;241:1912-5.
2. Vargas C, Fryer A, Mahajan C, et al. Dose-volume comparison of proton therapy and intensity-modulated radiotherapy for prostate cancer. Int J Radiat Oncol Biol Phys. 2008;70:744-51.
3. Goitein M. Magical protons? Int J Radiat Oncol Biol Phys. 2008;70:654-6.
4. Vargas C, Wagner M, Mahajan C, et al. Proton therapy coverage for prostate cancer treatment. Int J Radiat Oncol Biol Phys. 2008;70:1492-1501.
5. Pollack A, Zagars GK, Starkschall G, et al. Prostate cancer radiation dose response: results of the M. D. Anderson phase III randomized trial. Int J Radiat Oncol Biol Phys. 2002;53:1097-1105.
6. Mendenhall NP, Li Z, Hoppe BS, et al. Early outcomes from three prospective trials of image-guided proton therapy for prostate cancer. Int J Radiat Oncol Biol Phys. 2010 Nov 17. [Epub ahead of print]
7. Travis LB, Hill DA, Dores GM, et al. Breast cancer following radiotherapy and chemotherapy among young women with Hodgkin disease. JAMA. 2003;290:465-75.
8. Travis LB, Gospodarowicz M, Curtis RE, et al. Lung cancer following chemotherapy and radiotherapy for Hodgkin's disease. J Natl Cancer Inst. 2002;94:182-92.
9. Fontenot JD, Lee AK, Newhauser WD. Risk of secondary malignant neoplasms from proton therapy and intensity-modulated X-ray therapy for early-stage prostate cancer. Int J Radiat Oncol Biol Phys. 2009;74:616-22.
10. Zagars GK, Pollack A. Serum testosterone levels after external beam radiation for clinically localized prostate cancer. Int J Radiat Oncol Biol Phys. 1997;39:85-9.
11. King CR, Maxim PG, Hsu A. Kapp DS. Incidental testicular irradiation from prostate IMRT: it all adds up. Int J Radiat Oncol Biol Phys. 2010;77:484-9. Epub 2009 Sep 3.
12. Oermann EK, Suy S, Hanscom HN, et al. Low incidence of new biochemical and clinical hypogonadism following hypofractionated stereotactic body radiation therapy (SBRT) monotherapy for low- to intermediate-risk prostate cancer. J Hematol Oncol. 2011;4:12.
13. Nichols RC, Jr, Morris CG, Hoppe BS, et al. Proton radiotherapy for prostate cancer is not associated with posttreatment testosterone suppression. Int J Radiat Oncol Biol Phys. 2011. [In Press].
14. Trofimov A, Nguyen PL, Coen JJ, et al. Radiotherapy treatment of early-stage prostate cancer with IMRT and protons: a treatment planning comparison. Int J Radiat Oncol Biol Phys. 2007;69:444-53.
15. Institute for Clinical and Economic Review (ICER). Management options for low-risk prostate cancer. 2010.
16. Valery JR, Hoppe BS, Henderson R, et al. Risk of hip and femoral neck fractures following proton therapy for prostate cancer. [Abstr.] Int J Radiat Oncol Biol Phys. 2010;78:S192-S193.
17. Telhaug R, Fossa SD, Ous S. Definitive radiotherapy of prostatic cancer: the Norwegian Radium Hospital's experience (1976-1982). Prostate. 1987;11:77-86.
18. Perez CA, Walz BJ, Zivnuska FR, et al. Irradiation of carcinoma of the prostate localized to the pelvis: analysis of tumor response and prognosis. Int J Radiat Oncol Biol Phys. 1980;6:555-63.
19. Lawton CA, Won M, Pilepich MV, et al. Long-term treatment sequelae following external beam irradiation for adenocarcinoma of the prostate: analysis of RTOG studies 7506 and 7706. Int J Radiat Oncol Biol Phys. 1991;21:935-9.
20. Paulson DF, Lin GH, Hinshaw W, et al. Radical surgery versus radiotherapy for adenocarcinoma of the prostate. J Urol. 1982;128:502-4.
21. Duttenhaver JR, Shipley WU, Perrone T, et al. Protons or megavoltage X-rays as boost therapy for patients irradiated for localized prostatic carcinoma. An early phase I/II comparison. Cancer. 1983;51:1599-1604.
22. Shipley WU, Verhey LJ, Munzenrider JE, et al. Advanced prostate cancer: the results of a randomized comparative trial of high dose irradiation boosting with conformal protons compared with conventional dose irradiation using photons alone. Int J Radiat Oncol Biol Phys. 1995;32:3-12.
23. Yonemoto LT, Slater JD, Rossi CJ, Jr, et al. Combined proton and photon conformal radiation therapy for locally advanced carcinoma of the prostate: preliminary results of a phase I/II study. Int J Radiat Oncol Biol Phys. 1997;37:21-9.
24. Slater JD, Rossi CJ, Jr, Yonemoto LT, et al. Conformal proton therapy for early-stage prostate cancer. Urology. 1999;53:978-84.
25. Slater JD, Rossi CJ, Jr., Yonemoto LT, et al. Proton therapy for prostate cancer: the initial Loma Linda University experience. Int J Radiat Oncol Biol Phys. 2004;59:348-52.
26. Zietman AL, DeSilvio ML, Slater JD, et al. Comparison of conventional-dose vs high-dose conformal radiation therapy in clinically localized adenocarcinoma of the prostate: a randomized controlled trial. JAMA. 2005;294:1233-9.
27. Zietman AL. Correction: Inaccurate analysis and results in a study of radiation therapy in adenocarcinoma of the prostate. JAMA. 2008;299:898-9.
28. Zietman AL, Bae K, Slater JD, et al. Randomized trial comparing conventional-dose with high-dose conformal radiation therapy in early-stage adenocarcinoma of the prostate: long-term results from Proton Radiation Oncology Group/American College of Radiology 95-09. J Clin Oncol. 2010;28:1106-11.
29. Mayahara H, Murakami M, Kagawa K, et al. Acute morbidity of proton therapy for prostate cancer: the Hyogo Ion Beam Medical Center experience. Int J Radiat Oncol Biol Phys. 2007;69:434-43.
30. Nihei K, Ogino T, Onozawa M, et al. Multi-institutional phase II study of proton beam therapy for organ-confined prostate cancer focusing on the incidence of late rectal toxicities. Int J Radiat Oncol Biol Phys. 2010 Sep 8. [Epub ahead of print]
31. Coen JJ, Bae K, Zietman AL, et al. Acute and late toxicity after dose escalation to 82 GyE using conformal proton radiation for localized prostate cancer: initial report of American College of Radiology phase II study 03-12. Int J Radiat Oncol Biol Phys. 2010 Oct 5. [Epub ahead of print]
32. Konski A, Speier W, Hanlon A, et al. Is proton beam therapy cost effective in the treatment of adenocarcinoma of the prostate? J Clin Oncol. 2007;25:3603-8.
33. Peeters A, Grutters JP, Pijls-Johannesma M, et al. How costly is particle therapy? Cost analysis of external beam radiotherapy with carbon-ions, protons and photons. Radiother Oncol. 2010;95:45-53.
34. Arcangeli G, Saracino B, Gomellini S, et al. A prospective phase III randomized trial of hypofractionation versus conventional fractionation in patients with high-risk prostate cancer. Int J Radiat Oncol Biol Phys. 2010;78:11-18.
35. Brada M, Pijls-Johannesma M, De Ruysscher D. Proton therapy in clinical practice: current clinical evidence. J Clin Oncol. 2007;25:965-970.
36. Tepper JE. Protons and parachutes. J Clin Oncol. 2008;6:2436-7.
37. Goitein M, Cox JD. Should randomized clinical trials be required for proton radiotherapy? J Clin Oncol. 2008;26:175-6.
38. Glatstein E, Glick J, Kaiser L, et al. Should randomized clinical trials be required for proton radiotherapy? An alternative view. J Clin Oncol. 2008;26:2438-9.