Allogeneic BMT Ups 5-Year EFS in Ph- ALL
ORLANDO-Allogeneic bone marrow transplant (BMT) significantly reduced relapse rates and increased event-free survival (EFS) rates, but not overall survival, in adults with Philadelphia chromosome (Ph)-negative acute lymphoblastic leukemia (ALL) in first complete remission.
ORLANDOAllogeneic bone marrow transplant (BMT) significantly reduced relapse rates and increased event-free survival (EFS) rates, but not overall survival, in adults with Philadelphia chromosome (Ph)-negative acute lymphoblastic leukemia (ALL) in first complete remission.
Jacob M. Rowe, MD, of Rambam Medical Center, Haifa, Israel, reported the intent-to-treat analysis at the 43rd Annual Meeting of the American Society of Hematology (abstract 2009) on behalf of researchers in an ongoing joint Medical Research Council/Eastern Cooperative Oncology Group study (E2993).
All patients in this protocol receive two phases of standard induction chemotherapy. If the regimen produces a complete response, patients are assigned to allogeneic BMT if they have an HLA-matched sibling donor and are age 50 or under. Other complete remission patients are randomized to either standard consolidation/maintenance therapy for 2½ years or autologous BMT.
All patients receive identical intensification with high-dose methotrexate prior to undergoing their assigned or randomized therapy.
Over 1,200 patients have been registered, 93% of whom achieved a complete remission. The median age is 30 years (range, 14 to 60 years). The induction death rate is 5%.
Dr. Rowe’s presentation was based on 173 Ph-negative patients assigned to allogeneic BMT and 264 Ph-negative patients who were randomized. Standard risk was defined as Ph-negative, age over 35 years, time to complete remission longer than 4 weeks, and white blood cell count below 30,000/µL for B lineage disease and below 100,000/µL for T lineage disease.
Overall survival was 44% at 5 years and 35% at 7 years in the Ph-negative patients. "We have over 100 patients already out past 5 years," Dr. Rowe said.
The 5-year event-free survival was 54% in the Ph-negative patients who had allogeneic BMT vs 34% for all randomized Ph-negative patients (P = .04). The 5-year overall survival was 54% vs 43%, respectively (P = .4), and the 5-year relapse rate was 23% vs 61% (P = .001), illustrating what Dr. Rowe described as "a very potent graft-vs-leukemia effect for leukemia patients in first remission."
Analysis by Risk Group
The most impressive differences were for standard-risk patients (see Table). In this group, event-free survival was 67% with allogeneic BMT vs 44% for the randomized patients; overall survival was 69% vs 50%, respectively; and the relapse rate was 15% vs 51%, respectively.
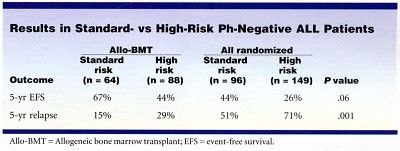
"For each risk subgroup, the allogeneic group appears to do better than the randomized cohort, but these are small numbers," Dr. Rowe said. In the best subgroup, overall survival was 80% for allogeneic BMT for B lineage, standard-risk patients vs 58% for similar patients in the randomized population.
"Even though we are dealing with relatively small numbers, this is notable because there has been a persistent objection to submitting standard-risk patients, particular T-lineage patients, to transplant, because they do well with standard therapy," he said. "We agree that they do well, with a 60% overall survival in the literature, but they appear to do even better with allogeneic transplant."
He concluded that allogeneic BMT "can provide a potent antileukemia effect to all adult patients with ALL in first complete remission. Despite increased early toxicity and a transplant-related mortality of 21%, allogeneic BMT provides favorable long-term results."
Overall Survival an Issue
The lack of significant difference in overall survival associated with allogeneic BMT for the patients as a whole sparked considerable discussion. One attendee said that since overall survival was not changed for the group as a whole, "why should I recommend this very toxic procedure to a patient?"
Dr. Rowe said that the reason was the greater chance of a cure at 5 years. He attributed the lack of significance in overall survival to study statisticians’ use of log-rank tests, which he said "may not be the most appropriate, as this is an ongoing study."
The study continues to accrue patients, predominantly to complete accrual to answer the "autologous transplant vs chemotherapy question" in the randomized arm, Dr. Rowe said.