Antidepressants continue to show increased inhibition of colorectal tumor cell growth
Use of antidepressants, particularly selective serotonin reuptake inhibitors and possibly tricyclic antidepressants, is associated with a reduced risk of colorectal cancer, according to research by the Group Health Research Institute in Seattle. But it’s too soon to make specific recommendations on how to harness this potential value of these drugs in cancer prevention.
Use of antidepressants, particularly selective serotonin reuptake inhibitors and possibly tricyclic antidepressants, is associated with a reduced risk of colorectal cancer, according to research by the Group Health Research Institute in Seattle. But it’s too soon to make specific recommendations on how to harness this potential value of these drugs in cancer prevention.
“The first thing we really have to make sure of is that the benefits are real: That the results are not confounded, and to see some consistency across studies, and really believe that we are observing a causal association,” said Jessica Chubak, PhD, while presenting the study at the 2009 American Society of Preventive Oncology meeting in Tampa, Fla.

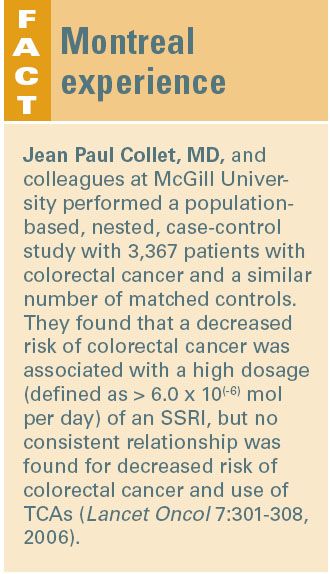
But the finding is consistent with other studies that suggest a reduced risk of colorectal cancer with use of SSRIs (see Fact Box). “SSRIs have been linked to hematosis and to inhibition of growth of colorectal tumor cells that are dependent on serotonin for their growth,” she said. “This led to our hypothesis of a reduced risk of colorectal cancer associated with their use.” There has also been a suggestion that the TCAs might increase cellular proliferation, which would lead to an increased risk of colorectal cancer, she said. “So going into the study, we had a hypothesis that if we were going to see an association, SSRIs would be associated with a reduced risk and TCAs would be associated with either a reduced or increased risk or possibly nothing at all,” she said.
The study was a case-control analysis of antidepressant use in 641 patients with colorectal cancer and 641 controls (healthy people who had the same health insurance payer as the patients). The information on medication use came from the Group Health pharmacy records. The researchers looked at antidepressant use in the 10 years before a diagnosis of colorectal cancer was made. Patients who first used an SSRI or a TCA in the year before they received a diagnosis of colorectal were excluded to control for any possible bias that they may have started using an antidepressant because of their disease.
As evidence that individuals were taking the medication as it was prescribed, two prescriptions for a particular class of antidepressant were required to be filled within a six-month period. Both cases and controls were closely matched with regard to age (mean age 70 years) and gender, although the cases tended to have a higher body mass index than the controls. They also were more likely to have diabetes and to be current or former smokers.
Twenty percent (n = 127) of the case patients and 24% (n = 155) of the controls used antidepressants for a median of 1.8 and 1.1 years, respectively.
Antidepressant use was associated with a 30% reduction in the risk of colorectal cancer, after adjusting for the confounders of smoking, NSAID and aspirin use, and diabetes, Dr. Chubak said. “This result is consistent with other studies suggesting a reduced risk of colorectal cancer with SSRIs, and also with TCAs.”
The goal now is to translate the finding into clinical practice, starting with making sure that the benefits of antidepressants are well characterized. “We want to know not only that antidepressant use in general might reduce the risk of colorectal cancer, but to find out which antidepressants specifically,” she said. “Not just SSRIs, but which SSRIs. What kind of dosing are we talking about? So I think it involves digging a lot deeper.”
Ultimately, the risks and benefits must be weighed. “It is reassuring that we are not seeing increased risk because antidepressants are so commonly used. I think there is potential if we see a lot of other studies that are consistent and we can address some of the questions,” she said. “I don’t think we are able to come up with specific recommendations yet.”