Stop and smell the volatile organic compounds in lung ca
SAN FRANCISCO-Studies have identified specific volatile organic compounds in the breath of lung cancer patients, but the origin of those compounds is still ambiguous: Are they from the tumor itself, the tumor micro-environment, or a reaction to the tumor by the human body?
SAN FRANCISCO-Studies have identified specific volatile organic compounds in the breath of lung cancer patients, but the origin of those compounds is still ambiguous: Are they from the tumor itself, the tumor micro-environment, or a reaction to the tumor by the human body? A group from the Technion-Israel Institute of Technology in Haifa, led by Hossam Haick, PhD, has developed a nanotechnology that detects patterns of volatile organic compounds that are unique to cancer.

"When exhaled breath is tested using gas chromatography/mass spectrometry, there are significant differences between breath of people who are healthy and those with cancer," said Nir Peled, MD, PhD, at the 2009 World Conference on Lung Cancer. Dr. Peled is a researcher and a Fulbright scholar at the University of Colorado in Denver who works in tight collaboration with Dr. Haick.
"Exhaled breath is going to become a medium that will be prominent in the next few years in medicine," he predicted. "We can trap these volatile organic compounds with high sensitivity these days. The sensing nanotechnology we used in our research can now detect one part per billion of these compounds."
The group set out to show that the source of the cancer's smell print is probably the cancer cells themselves. "We took different types of cancer cell lines: non-small-cell lung cancer (NSCLC), small-cell lung cancer (SCLC), and pancreatic cancer cell lines," Dr. Peled explained.
"We put the cells in a dish and put a solvent around the head space to collect the odor-print over several days. Then we sent the samples to Dr. Haick's laboratories in Israel where they disrobed the odor-print and carried out analysis by their "electronic nose" device based on nanosensors and, also, gas chromatography/mass spectrometry.
"Using this ‘electronic nose' we detected a signal with different electrical signals, allowing us to differentiate between the different groups of cancer," Dr. Peled said. The researchers found that lung cancer cells share five unique volatile organic compounds (see Table).
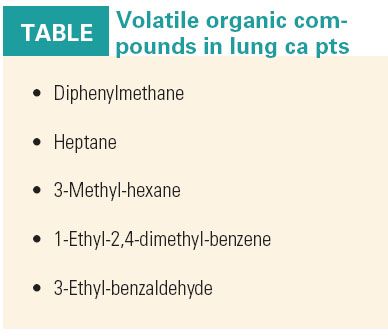
Three of these compounds occurred in the exhaled breath of more than 90% of NSCLC patients, indicating that the compounds are transferred to the breath via a metabolic pathway of the tumor cells (abstract B3.5).
"We are really excited about these results," Dr. Peled said. He added that a practical device, which is capable of determining different types of cancers before they become symptomatic, might be possible in the next several years.