PERSPECTIVE
Michael S. Lee, MD and Shubham Pant, MD discuss barriers to pancreatic cancer clinical trial enrollment at cancernetwork.com/barriers-perspective
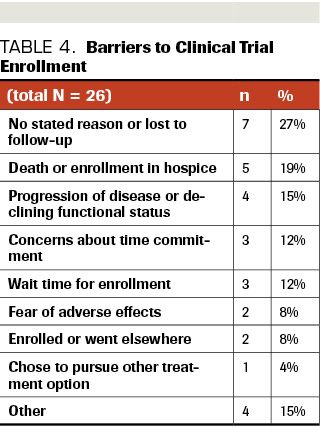
ABSTRACT BACKGROUND: Early-phase clinical trials are critical to the advancement of cancer care, especially in patients with pancreatic ductal adenocarcinoma, given its aggressive nature and limited available therapeutic options. METHODS: A retrospective chart review of all patients with refractory or metastatic pancreatic ductal adenocarcinoma, referred to the Sarah Cannon Research Institute at HealthONE between 2014 and 2019, were reviewed. Patients who completed genomic profiling and qualified for a phase 1 trial (primarily 1a but some 1b) were identified to assess barriers to trial enrollment. RESULTS: Of 74 identified patients, 54 patients (73%) qualified for at least 1 clinical trial based on eligibility criteria and alterations detected via molecular profiling. Up to 40 industry-sponsored clinical trials were available during this time for consideration. Of the 54, 28 patients (52%) enrolled in a clinical trial, while 26 (48%) did not enroll. The most frequently cited barriers to enrollment were concerns regarding time commitment (12%), prolonged wait time for enrollment (12%), and fear of adverse events (8%). Seven of the 26 patients (27%) were lost to follow-up or had no stated reason for declining enrollment; others did not go on trial due to death/transition to hospice (n=5; 19%) or progression of disease/declining functional status (n=4; 15%). There were few statistically significant differences between patients who chose to go on trial and those who declined. CONCLUSIONS: An understanding of why eligible patients elect not to participate in early-phase clinical trials provides insight into the patient experience and can help identify misperceptions and areas for improvement in education and the clinical trial enrollment process.
Rachael Galvin, DO, MPH, Department of Surgery, Swedish Medical Center, Englewood, CO

Chirstine Chung, DO, Department of Surgery, Swedish Medical Center, Englewood, CO

Ella Achenbach, Department of Clinical Oncology Research, Sarah Cannon Research Institute at HealthONE, Denver, CO

Pancreatic ductal adenocarcinoma (PDAC) is an aggressive malignancy with limited effective therapeutic options available. Surgical resection remains first-line treatment, but most patients are not candidates due to advanced stage at initial presentation. For these patients with advanced unresectable disease, few standard-of-care therapeutic options are available, and overall the 5-year survival for patients with PDAC is about 9% to 10%.1,2
In recent years, data from clinical trials have identified potentially actionable molecular alterations in these cancers that may improve clinical outcomes,3-6 and many early-phase clinical trials investigating novel treatment options for patients with PDAC are ongoing. However, impediments to participation exist. Many barriers to enrollment in late-phase clinical trials have been identified in individuals with cancer, including uncertainty about associated risks, fear of randomization, and strict eligibility criteria.7-11 Whether barriers to enrollment in nonrandomized, early-phase clinical trials exist in patients who meet all eligibility criteria has yet to be studied. This study analyzes factors leading individuals with advanced PDAC to not enroll in such trials, despite meeting eligibility criteria.
Oliwier Dziadkowiec, PhD, Graduate Medical School Education HCA Healthcare, Denver, CO

Shiraj Sen, MD, PhD, Department of Clinical Oncology Research, Sarah Cannon Research Institute at HealthONE, Denver, CO

We performed a retrospective chart review of all patients with refractory or metastatic PDAC who were referred to the Sarah Cannon Research Institute at HealthONE from between 2014 and 2019. Patients who completed genomic profiling via FoundationOne (Foundation Medicine) tissue-based sampling and/or Guardant360 (Guardant Health) blood-based sampling were identified. Included in our analysis were those patients who qualified for enrollment onto an early-phase clinical trial enrollment based on biomarkers identified via molecular profiling and meeting all other eligibility criteria. Those patients who qualified for early-phase clinical trial enrollment, but chose not to enroll, were evaluated to determine cited barriers to clinical trial participation. All patients provided written informed consent for treatment consideration at Sarah Cannon Research Institute at HealthONE. An institutional review board (IRB) exemption was obtained from the HCA HealthONE Physician Services Group/Graduate Medical Education IRB for an ad hoc analysis reported in this manuscript.
A multivariate logistic regression analysis was performed to compare patients who qualified for a clinical trial and went on to enroll with those patients who declined enrollment. This analysis was completed using R Studio.12 A Fisher’s exact test was used to assess categorical variables, and t test and Mann-Whitney U tests were used for continuous variables. Statistical significance was set at P < .05.
A total of 74 patients who completed genomic profiling via FoundationOne and/or Guardant360 were identified. Of these 74 patients, 54 (73%) qualified for at least 1 clinical trial based on eligibility criteria as well as on alterations detected via molecular profiling (Table 1). A total of 28 patients (52%) enrolled in a clinical trial, while 26 patients (48%) did not enroll. One patient in each of the groups had missing information and was excluded from the multivariate and univariate analysis, bringing down the sample for statistical analysis to 52.
TABLE 1: Characteristics of Patients with PDAC
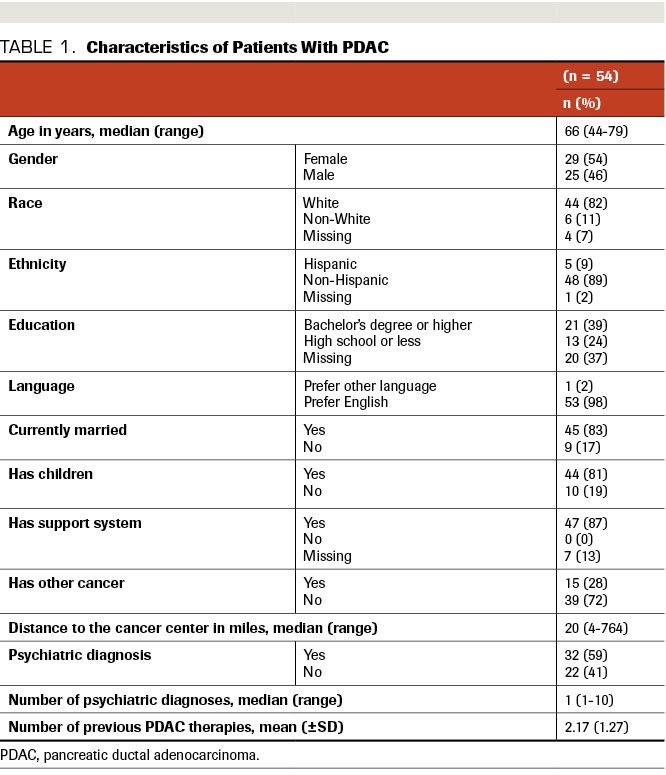
The study population included 54 patients, 6 (11)% of whom were non-White (Table 1). There were more male than female patients (29 vs 25). Median age was 66 years (range, 44-79). The majority of patients were married (83%) and had children (81%). All respondents indicated they had good social support on clinic intake forms; 7 patients chose not to respond to this item. English was the preferred/primary language of 98% of patients. Less than half (39%) had obtained a bachelor’s degree or higher, though education level was not reported by a significant number of patients (20; 37%). Most patients did not have a history of prior cancer (72%) and the majority did have a prior diagnosis of anxiety, depression, or other psychiatric diagnosis (59%). The median distance lived from the trial site was 20 miles, but the range was wide (4 to 764 miles). The range narrowed to 4 to 117 when 1 patient who traveled 764 miles was excluded. Almost all patients (83.3%) who qualified for phase 1 clinical trials were classified as ECOG performance status (PS) of 0 to 1, likely because most of the phase 1 clinical trials for which these patients qualified required an ECOG PS of 0 to 1; only 5 patients had ECOG PS of 2 to 3, and 4 patients did not have ECOG PS recorded in the chart. Thus, the data set does not allow for evaluation of whether a patient’s ECOG PS impacted their desire to enroll onto a trial. Patient demographics are summarized in Table 1.
When comparing those who enrolled in a clinical trial with those who did not enroll, no significant differences emerged between the groups in terms of age, sex, race, ethnicity, language preference, education level, marriage status, or history of prior cancer (Table 2). As mentioned above, we were unable to evaluate whether a patient’s ECOG PS impacted their desire to enroll onto trial, as most of our study participants had excellent ECOG PS (0-1). Additionally, insurance status did not play a role, as all patients in our trial were insured with either Medicare (42.5%), Medicaid (5.5%), or another insurance plan (52.0%). We could not assess whether religious or spiritual beliefs played a role in patients’ motivation to go on trial, as this was a retrospective chart review and such information was not typically recorded in the patients’ charts.
TABLE 2: Differences Between PDAC Patients Who Qualified for Clinical Trials and Participated and Those Who Qualified but Decided Not to Participate (univariate analysis)
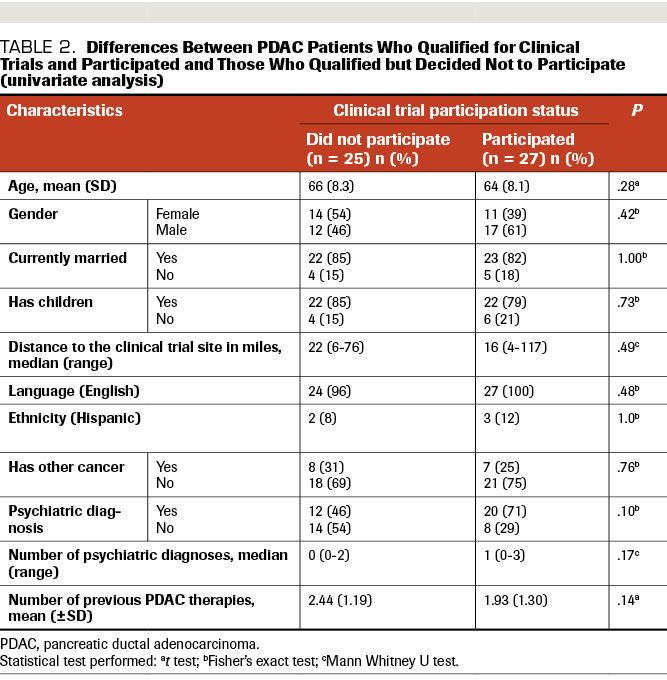
There was a trend toward significant difference between the 2 groups with regard to number of prior treatments for their PDAC and number of psychiatric comorbidities. The patients who declined trial enrollment had, on average, undergone more PDAC therapies prior to clinical trial qualification (2.44 vs 1.93) and had fewer clinical diagnoses of anxiety/depression (0.69 vs 1.04). The only significant difference between the groups related to median distance from their home to the trial site: Those who declined enrollment lived farther away (median 57.15 vs 31.46 miles). However, when we further examined the distance lived from the trial site, the significant difference was caused by 1 outlier, a patient who have had to travel more than 700 miles to participate. When this outlier was removed and the Mann–Whitney U repeated, there remained no significant difference between the 2 groups in terms of distance traveled to the trial site.
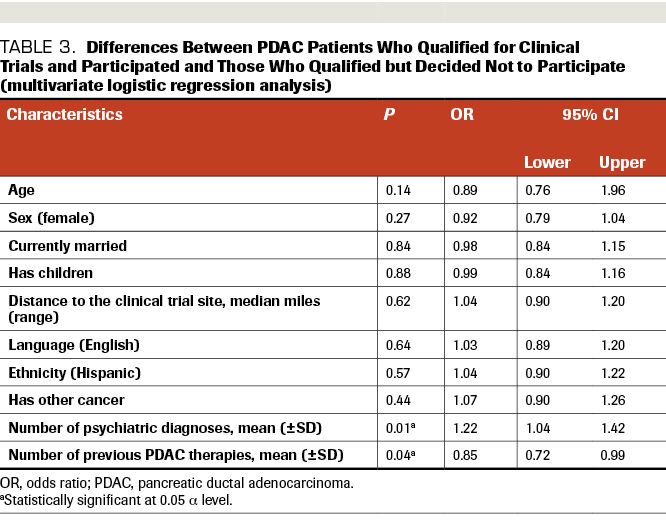
After controlling for age, sex, marital status, children, distance lived from trial site, language preference, ethnicity, and history of prior cancer, 2 factors became statistically significant: the number of prior PDAC therapies received and the number of psychiatric comorbidities (Table 3).
Cited reasons for not participating in a clinical trial were obtained via documentation, and they fell primarily into 1 of 9 categories. Of the 26 patients who qualified for a clinical trial but chose not to participate, 7 (27%) were lost to follow-up or had no stated reason for declining enrollment documented in their chart. Another subset of patients did not go on to participate in a trial due to death/transition to hospice (5; 19%) or progression of disease/declining functional status (4; 15%). The most frequently cited barriers to enrollment included concerns regarding time commitment (12%), fear of adverse effects (AEs; 8%), and prolonged wait time for enrollment in trial of interest (12%). The most common reasons for prolonged wait times in industry-sponsored trials included trial slot availability (specific trials sometimes had a wait time of a few weeks before the next set of slots opened) and delay in starting dosing on a trial as a result of screening requirements (ie, additional physician visits, labs, and imaging, which vary by trial). Less common reasons for prolonged wait times include trial amendments that may be required throughout the course of a study as updated data are obtained, and unexpected delays in trial slot availability due to other regulatory considerations. Two patients chose to transfer care elsewhere and 1 chose to pursue other treatment options. Four patients stated reasons other than the above for not enrolling. Cited barriers to clinical trial enrollment are summarized in Table 4.
TABLE 3: Differences Between PDAC Patients Who Qualified for Clinical Trials and Participated and Those Who Qualified but Decided Not to Participate (multivariate logistic regression analysis)
Despite the National Comprehensive Cancer Network statement that “the best management for any cancer patient is a clinical trial,” only 2% to 7% of cancer patients ultimately participate in these studies.8 Clinical trial enrollment is particularly important for advancing the treatment of pancreatic cancer, given its aggressive nature, high mortality, and short expected survival. Given that most patients with PDAC present with advanced-stage disease not amenable to surgical resection and have very few effective therapeutic options, a significant need exists for novel treatment options. Molecular profiling and targeted therapy based on identified somatic alterations has tremendous potential for patients with metastatic or refractory PDAC. In fact, the POLO trialdemonstrated efficacy of PARP inhibition in germline BRCA-mutated pancreatic cancers, and in 2019 the FDA approved olaparib, the first BRCA-targeted therapy for patients with PDAC.5,6 Most of these treatment options are still in early phases of development. Therefore, continued trial enrollment is critical in determining which treatment options may be effective for patients with specific gene mutations.
Barriers to cancer clinical trial enrollment have been well studied, with the hopes of developing interventions aimed at overcoming these impediments. Financial burden, distance from the cancer center, strict eligibility criteria, fear of randomization or placebo, and concerns about risks and AEs have been cited across numerous studies as significant barriers to participation, according to both patients and oncologists.7-10,13. Another significant barrier to clinical trial success includes the substantial regulatory and administrative burdens that can significantly delay trial completion and patient enrollment. While most of the patients in our study experienced delays in industry trial enrollment due to lack of trial slot availability, some of the trials were impacted by delays related to regulatory burden. In our study, we looked specifically at patients who qualified for clinical trials and elected not to enroll; strict eligibility criteria did not play a role. Additionally, we focused on early-phase clinical trials, which have no randomization and are reserved for patients in whom all standard-of-care options have been exhausted. Thus, fear of randomization was not a factor influencing our patient population.
TABLE 4: Barriers to Clinical Trial Enrollment
Surprisingly, none of the patients in our population cited financial concerns as a reason for declining to participate. This may be because fear regarding out-of-pocket expenses, like those for treatment drugs, is a major concern for many cancer patients, and trial drugs are provided for free on early-phase clinical trials.14 Additionally, most patients were referred to our center by their oncologist and had insurance (Medicare, Medicaid, or private plans) that would cover the cost of trial expenses.
Indirect costs, such as productivity loss and patient time costs, are other major concerns for cancer patients, which could explain why fears regarding time commitment, including driving to treatment sessions and follow-up appointments, was the primary barrier cited for 12% of patients.14 Interestingly, however, distance lived from the trial site was not a statistically significant variable when comparing those who did not enroll with those who did. This could be because most patients lived within a reasonable distance from the trial site, with few patients traveling from outside the Denver metropolitan area.
Most of the drug regimens offered on these phase 1 trials involved at least 1 intravenous or subcutaneous injection drug (17 of 27 trials); 10 trials involved oral drugs only. None of the patients specifically cited mode of drug administration as a deterrent to participation, but patients were not directly asked whether this factored into their decision to pursue a clinical trial or not.
Similar to responses given in prior studies, fear of AEs was cited among the top reasons for nonparticipation. Evidence supports the use of patient navigators and in-depth patient education sessions to improve the informed consent process and minimize barriers such as this during trial recruitment.7,15,16 Educating patients regarding realistic expectations about the true risk of severe AEs attributed to trial participation vs those associated with typical disease progression may aid in lessening trial refusal based on fear of AEs.15,16 However, this can prove challenging in early-phase clinical trials, given that the AEs of the drug under investigation may not be fully known. Perhaps education regarding the class of drug being studied and potential AEs could be improved upon. Additionally, the use of patient navigators to assess health literacy and to guide conversations between patients and providers may aid in these processes, and could be better implemented at our institution. No significant differences in education level, language preference, or age were seen between trial enrollees and those who declined. Thus, across the board, there is a need to provide better education about clinical trial expectations to our patients.
Improving timely access to trial participation could also improve recruitment, given that 19% of patients did not enroll due to wait time for enrollment or chose to enroll elsewhere. As mentioned previously, wait time in most instances was due to lack of trial slot availability, additional screening requirements prior to starting trial dosing, or delays due to trial amendments or other administrative/regulatory considerations. The oncology community recognizes the need to reduce administrative and regulatory burden on cancer clinical trials. In fact, according to a survey conducted by the American Society of Clinical Oncology (ASCO) and Association of American Cancer Institutes (AACI), the main barriers to conducting cancer clinical trials include contract negotiations, compliance with research organization requirements, site monitoring visits, management of regulatory documents, and external AE reporting.17,18 The survey’s respondents, who included physician-investigators, research staff, and administrators at both academic and community clinical research centers, indicated that 58% did not have adequate staffing to handle regulatory burden and 41% did not have adequate staffing to monitor regulatory compliance.17,18 The “Best Practices in Cancer Clinical Trial Initiative,” proposed by ASCO and AACI in response to these survey results, is aimed at addressing these regulatory and administrative burdens that hinder cancer research.17 There is a significant need for additional ongoing initiatives that address these barriers and prevent delays in patient access to clinical trial treatment options due to regulatory burden.
Michael S. Lee, MD and Shubham Pant, MD discuss barriers to pancreatic cancer clinical trial enrollment at cancernetwork.com/barriers-perspective
Timely access to clinical trials is particularly important in this patient population, as patients with refractory or metastatic PDAC have such a short life expectancy. Delays in enrollment could lead to disease progression and disqualification from the trial during the waiting period. In fact, 35% of patients did not go on to clinical trial due to death, enrollment in hospice, decline in functional status, or progression of disease, making this the largest barrier to participation reported in our study. This demonstrates the need for improvement in assessing prognosis in metastatic cancers and also highlights the importance of improving timely access to clinical trial participation and minimizing the regulatory/administrative burdens that make clinical trials increasingly challenging to conduct.17,18
While empiric evidence and education regarding expectations is important, the decision to participate in a clinical trial is also based on the patient’s health-related values, cognitive–emotional state, and coping mechanisms.8 Thus, we chose to assess marital status, whether patients had children, perceived social support, psychiatric comorbidities, and number of previous PDAC treatments in our analysis. The majority of our patients were married, had children, and indicated that they had good social support; so, while previous research has shown a propensity for those who enroll in clinical trials to be more influenced by friends, family, and their physician than those who decline, family and support system did not seem to influence trial enrollment in our population.10
Significant differences were found in the number of patients with anxiety and/or depression and in the number of prior PDAC treatments patients had undergone. Interestingly, the patients who agreed to participate in a clinical trial had, on average, more clinically diagnosed depression and/or anxiety. Because timing of the initial diagnosis of anxiety/depression is not well documented in the chart, it is difficult to say if most of these patients had this diagnosis prior to their cancer detection or if it was a reactionary anxiety/depression related to their cancer diagnosis. More research into the impact of anxiety/depression and decisions to pursue clinical trial enrollment is needed.19 Previous research has found that cancer patients who participate in clinical trials often overestimate the likelihood that they will have a positive response; this “treatment-specific optimism” reportedly helps patients cope with a poor prognosis and is associated with better mental health outcomes.20 On the other hand, treatment-specific optimism is negatively associated with baseline depressive or anxiety symptoms.20 While many patients disclosed a diagnosis of depression or anxiety on their intake forms, the majority were already being treated for these conditions and we do not have information regarding whether patients felt their symptoms were well controlled. Future research could benefit from eliciting more information regarding baseline depressive symptoms and timing of psychiatric diagnoses, as up to 19% of cancer patients develop an adjustment disorder in response to their cancer diagnosis.21 A more thorough understanding of patients’ baseline cognitive–emotional health could aid clinicians in identifying patients who could benefit from mental health interventions concurrent with their cancer care. This in turn could improve clinical trial enrollment, as willingness to participate has been linked to the patients’ perceived likelihood to benefit from the trial and treatment-related optimism.11,20
Overall, the patients who declined clinical trial enrollment had undergone more prior treatment modalities for their cancer. This could represent more aggressive tumor biology in these patients, and could thus explain why more than one-third of the patients cited transition to hospice, progression of disease, declining functional status, or death as the reason for not enrolling. ECOG PS did not play a role, given that all patients were ECOG PS 0 or 1 at time of acceptance into a phase 1 clinical trial. Another possible explanation is that patients may have more negative perceptions regarding the potential benefit of a trial, after undergoing a higher number of failed therapies.
One meaningful limitation of this study is the total small sample size. Given that these patients have advanced disease, life expectancy is short, which limits our ability to study this population in larger numbers. In fact, our study population is fairly robust for this specific cancer type and given that it is a single-site retrospective review. Referral bias was also a limitation of our study. Almost all patients (93%) were referred to our institution by their oncologist; only 4 were self-referred. Thus, we could not determine whether trial knowledge/awareness was different between the 2 groups. Due to this referral bias, all patients had some type of health insurance, whether Medicare, Medicaid, or another health plan that generally covers the cost of clinical trial expenses (eg, Blue Cross Blue Shield, Kaiser, etc). There was not significant geographic or cultural/ethnic diversity as most of our patients were from the Denver metropolitan area, primarily Caucasian, and English speaking.
Additionally, the logistic regression was not optimally powered due to the smaller sample size and nature of the disease. It is possible that with a larger sample size, we could have observed more significant differences. When we examine the size of odds ratios and confidence intervals, that possibility becomes less likely. The use of multivariate analysis allowed us to determine a significant difference between the 2 groups, while controlling for all other differences, which would not have been possible in a univariate analysis. Future research could benefit from larger sample sizes, which may be better achieved via a multi-institution study.
This study is novel, as it is the first study to our knowledge that has examined barriers to clinical trial enrollment in patients who are eligible for phase 1 trial enrollment. We found that of all patients who were eligible for trial enrollment, underwent molecular profiling, and qualified for a clinical trial, almost half chose not to enroll. While 27% of patients who did not enroll were lost to follow-up or did not provide a specific reason for declining trial participation, a multitude of reasons were given for why the remaining patients did not wish to enroll. While trial participation may not be the right choice for every patient, an understanding of why patients choose not to enroll does provide important insight into the patient experience and can help identify common patient misperceptions and areas for improvement in the clinical trial enrollment process. This study highlights the need for improved patient education regarding clinical trials and expected AEs, better assessment of prognosis in patients with metastatic cancer, and the need for further research examining the impact of a patient’s cognitive–emotional health on willingness to participate in cancer research. Further characterization of barriers to clinical trial enrollment in pancreatic cancer patients could be used to develop interventions aimed at addressing these perceived barriers specifically. Tailored interventions and further research in improving clinical trial enrollment are critical to making advances in treating this aggressive malignancy.
References