Clinical Management of EGFRI Dermatologic Toxicities: US Perspective
Management of dermatologic toxicities from epidermal growth-factor receptor inhibitors (EGFRIs) is best tailored to the type of skin lesions present, extent of body surface involvement, and anatomic location affected. Although few randomized trials have been undertaken to address treatment of skin, hair, or nail side effects to this class of drugs, some basic principles of therapy based on experience of referral centers can help mitigate these toxicities and ensure consistent EGFRI administration and maintenance of patient quality of life. Patient education as to the expected EGFRI side effects and early physician intervention when these side effects appear can improve outcomes. Two dermatologists who treat high numbers of patients affected by these EGFRI-induced cutaneous side effects submit their recommendations for management.
Management of dermatologic toxicities from epidermal growth-factor receptor inhibitors (EGFRIs) is best tailored to the type of skin lesions present, extent of body surface involvement, and anatomic location affected. Although few randomized trials have been undertaken to address treatment of skin, hair, or nail side effects to this class of drugs, some basic principles of therapy based on experience of referral centers can help mitigate these toxicities and ensure consistent EGFRI administration and maintenance of patient quality of life. Patient education as to the expected EGFRI side effects and early physician intervention when these side effects appear can improve outcomes. Two dermatologists who treat high numbers of patients affected by these EGFRI-induced cutaneous side effects submit their recommendations for management.
The dermatologic side effects of epidermal growth factor receptor inhibitors (EGFRIs) may be associated with significant pain and pruritus, as well as patient anxiety related to the cosmetic disturbance produced by this cancer therapy[1] (Figure 1). This may negatively impact quality of life and compromise patient compliance to anticancer therapy.[2] Thus, it is important to educate patients on these potential dermatologic events, and to provide effective treatment options for minimizing the progression and severity of such skin toxicity. Ideally, EGFRI dose modification and/or discontinuation, which was reported in 9% to 17% of patients in pivotal studies,[3,4] would not be necessary. In the postapproval setting, up to 32% of providers reported discontinuing EGFRI therapy due to rash; 76% of those surveyed stated that administration of the EGFRI was held at some point during therapy.[1] There is an overwhelming need for improved management strategies as more patients are undergoing this form of targeted cancer therapy.
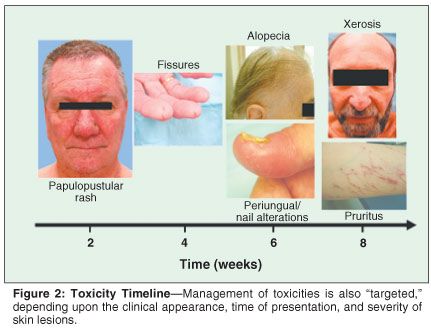
Numerous anecdotal reports on the successful management of the cutaneous side effects of EGFRI therapy have led to several controlled studies currently underway and two that have been completed (Table 1). Treatment is best tailored to the type of skin lesions, severity of the lesions, and anatomic site affected by the EGFRI treatment. Knowledge of the chronology and appearance of skin toxicities is key, as it allows for early recognition of these cutaneous side effects and ensures prompt therapy (Figure 2). A multidisciplinary approach with frequent follow-ups (every 2 to 4 weeks until resolution) is advisable[5] so that treatment is optimized and the likelihood of EGFRI drug discontinuation is minimal.
The recommendations set forth below are generated from the experiences of dermatologists who encounter patients treated with EGFRI agents in different clinical settings: a dermatologist who practices in a referral center for cutaneous toxicities (M. Lacouture, SERIES clinic) and a dermatologist who specializes in the evaluation of hospital inpatients with dermatologic complaints (J. Cotliar, David Geffen School of Medicine at UCLA).
Papulopustular Reaction
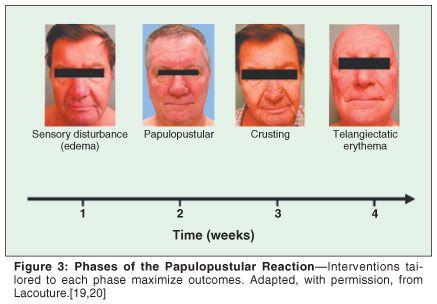
Figure 3 shows the phases generally experienced during the course of a papulopustular reaction. Clinical experience suggests that topical corticosteroids can be effective in the management of these skin reactions.[6] However, the need for high-potency formulations precludes the long-term use of topical corticosteroids on frequently affected areas, such as the face.[7] The use of colloidal oatmeal lotion (Aveeno), which has anti-inflammatory properties and a beneficial toxicity profile, resulted in four of seven patients exhibiting a complete response and three of seven experiencing a partial response.[8] The topical antibiotic clindamycin phosphate 1% gel has demonstrated favorable results, producing a drying effect on inflammatory pustules.[6] Topical retinoids, α-hydroxyacids, and benzoyl peroxide have also been reported to be effective in some cases, but use of these agents is associated with significant irritation and skin dryness and should be generally avoided.[9]
For mild/moderate eruptions (those causing some symptomatic or cosmetic discomfort but not interfering with activities of daily living), oral semisynthetic tetracycline antibiotics, such as doxycycline or minocycline 100 mg bid, alone or in combination with the topical treatments indicated above, are effective in most cases (Figure 4).[5] These are given over a course of at least 4 to 6 weeks and are usually well tolerated. Although the eruption does not seem to be mediated by infectious agents, the tetracyclines' anti-inflammatory properties, via matrix metalloproteinase (MMP) inhibition, may explain their effectiveness.[10,11] Doxycycline, the agent of this class with the highest MMP activity,[12] can be used in doses of 50 to 100 mg twice daily, typically resulting in a decrease in number of skin lesions within 1 to 2 weeks. No interactions have been reported with the use of tetracyclines in combination with EGFRIs.
For papulopustular reactions that have not improved despite 2 weeks of high-dose (100 mg twice daily) tetracycline therapy and topical steroids, systemic steroids can be administered as an adjunct to systemic antibiotics and the topical agents. Short courses of prednisone (0.35 to 0.5 mg/kg qd) or methylprednisolone (Medrol dose pack) can be effective in controlling flares.[13] Improvement in both the symptoms and extent of skin lesions are observed within a few days. Failure to improve after this step has been taken should lead to EGFRI dose interruption for 14 days or until the rash is ≤ grade 1 in severity, at which point reescalation should be intitiated in accordance with package insert recommendations. In cases where the aforementioned interventions have failed and when evidence of tumor response to the EGFRI has been demonstrated, the use of oral isotretinoin may be considered, as was reported to be effective in two cases of patients with papulopustular reactions to cetuximab (Erbitux).[14] However, little is known about the effects of isotretinoin on tumor biology or interactions with EGFRIs and this treatment should be undertaken on a per patient basis.
Moreover, failure of improvement of papulopustular reactions with the use of a topical steroid and an oral tetracycline mandates culture of lesions, to identify pathogen and antibiotic sensitivities. Both gram-positive and gram-negative organisms, as well as fungi, have been cultured from such patients (M. Lacouture, unpublished data). With the decrease or cessation of the EGFR inhibitor, rapid improvement of skin lesions follows, generally in 1 to 2 weeks, after which EGFRI treatment is usually continued or resumed at a lower dose. Thus, it may be of benefit to continue concurrent topical and oral therapy if dose interruptions of EGFRI medications are needed, in order to prevent or minimize recurrent episodes of these expected dermatologic side effects.
Universally, authors report that the papulopustular eruption disappears within a few days or weeks after treatment with EGFRI agents is discontinued. No relationship has been observed between the appearance or severity of the papulopustular eruption and a particular patient's history of oily skin, acne, or rosacea. One study reported a more frequent occurrence in photoexposed areas.[15] Therefore, patients should be counseled to minimize sun exposure and use broad-spectrum sunscreens, as photoexacerbation of the rash may occur. In the rare instance that a severe, life-threatening, and disabling skin reaction from the use of EGFRIs occurs, the EGFRI should be stopped immediately and the patient should be monitored in a hospital setting. Reinstitution of EGFRI therapy should only be considered in a supervised setting.
Paronychia
Paronychia associated with the use of EGFRIs may last for months if untreated. See Figure 5 for an algorithm detailing management of nail/periungual toxicities. This side effect can be very painful and can render the nail folds susceptible to infection. Patients should be encouraged to use a daily emollient (ammonium lactate 12% cream or urea 40% cream) on their palms and soles, as well as the nails and periunguium. The softening and moisturizing of these tissues may prevent paronychia and skin fissuring. If edema or erythema occurs, a high-potency topical corticosteroid (clobetasol ointment or flurandrenolide (Cordran) adhesive steroid tape) may be used.
When discharge is present, cultures should be obtained; sensitivities should dictate the systemic antibiotic of choice. Soaking fingertips in 1:10 white vinegar in water solution for 5 minutes a day may also help due to its bactericidal effect. Splinting can prevent trauma and pain. If these interventions have failed, intralesional corticosteroids (triamcinolone 10 mg/cc, 0.02 cc per lateral nail fold) or nail avulsion may be needed. Although nail avulsion is not an innocuous procedure, pain relief often occurs shortly thereafter.
Xerosis and Pruritus
Dryness of the skin in response to EGFRI therapy is common and may take place at sites distant from where papulopustular lesions occur. This xerosis may also plague patients at locations where papulopustular outbreaks previously arose and were effectively treated. All patients should be encouraged to apply highly occlusive emollients (Aquaphor or Vaseline) to both prevent and alleviate xerosis, except in regions where the application may further potentiate the characteristic inflammatory papulopustular lesions associated with EGFRI treatment. These moisturizing preparations may be mixed with 10% to 20% urea or 12% lactic acid to aid with desquamation, if there are no signs of skin inflammation (ie, redness, sensitivity). See Figure 6 for a xerosis management algorithm.
Sensitive skin care recommendations and the use of hypoallergenic products such as Vanicream are advisable. These preparations have been found to be particularly useful in formulations with or without sunscreen, given that they are devoid of the numerous potential irritants and fragrances found in the majority of widely available commercial emollients. The pruritus that stems from severe xerosis can be a difficult, chronic symptom that, if left untreated, can lead to widespread excoriations and an increased risk of secondary skin infection. This can be remedied with oral antihistamines such as diphenhydramine, cetirizine (Zyrtec), loratadine, or hydroxyzine based on the patient's severity of pruritus, tolerability of the antihistamine, and need for soporific effect. Pregabalin (Lyrica), which works via the inhibition of calcitonin gene-related peptide,[16] was reported to be effective in patients on cetuximab who had previously failed to respond to oral antihistamines.[17] Pregabalin, which is indicated for the management of neuropathic pain and post-herpetic neuralgia, is usually administered at doses of 75 to 100 mg bid. See Figure 7 for a pruritus management algorithm.
Telangiectasia
Telangiectasias caused by treatment with EGFRIs often appear in areas where papulopustules formerly occurred. Pulsed-dye laser therapy can be used to accelerate resolution of individual lesions[18] but should only be considered in extreme cases or after EGFRI therapy has been discontinued. Due to the impaired wound healing transiently caused by EGFR inhibition, the use of lower fluences is recommended (S.S. Yoo, personal communication, March 2007).
Hair Abnormalities
Hypertrichosis of the face may be treated with depilatory methods such as electrolysis, or laser hair removal. Chemical depilatories should be avoided due to extreme sensitivity of skin in these patients. Waxing may also be problematic due to skin fragility. Trichomegaly of the eyelashes and eyebrows can be treated with trimming performed by an ophthalmologist. No agents have been evaluated for the treatment of alopecia associated with EGFRI use, but some patients have reported spontaneous improvement of hair growth after several months of continued EGFRI therapy. For the initial alopecia, topical corticosteroids will relieve the inflammation and papulopustules, minimizing follicular inflammation and hair loss.
Conclusions
In order to ensure patient quality of life and compliance to antineoplastic therapy, a multidisciplinary approach including care provided by oncologists, dermatologists, and ophthalmologists is advisable. Cutaneous side effects may be difficult to tolerate, which necessitates vigilance on behalf of the physician so that interruption or cessation of EGFRI therapy is not the first or only management strategy. Patient education with respect to the cutaneous side effects associated with EGFRIs will allow for earlier recognition of these toxicities and prompt intervention. This will ensure long-term compliance with the targeted cancer therapy.
Few randomized, controlled trials have been conducted to assess the efficacy of agents for the management of the dermatologic side effects associated with EGFRIs. In these studies, prophylactic management with tetracycline 250 mg bid was shown to reduce the severity but not the incidence of papulopustular reaction,[21] whereas another showed that minocycline 100 mg twice daily reduced the number of papulopustular lesions.[22] Studies to address the histology, key structures, and mediators involved, as well as why they occur in specific anatomic locations, are needed. Moreover, since the papulopustular reaction is established as an indicator of both EGFRI efficacy and patient survival, understanding of the correlation between PPR and survival will serve as a predictive tool. A more accurate grading system is needed so that more consistency and accuracy is obtained during gradation.
The future direction of clinical trials performed to study the cutaneous adverse events of EGFRIs will hopefully address these critical issues and facilitate the progress of anticancer therapies.
Disclosures:
Mario E. Lacouture has received honoraria from OSI Pharmaceuticals, Imclone Systems. Jonathan Cotliar has served as a consultant for Amgen; Edith Mitchell has served as a consultant for Genentech, Sanofi-Aventis, Pfizer; received honoraria from Genentech, Sanofi-Aventis, Pfizer; and received research funds from Sanofi-Aventis, Pfizer.
Funding for this supplement was provided by Amgen.
References:
1. Lacouture M, Lai S, Rademaker A, et al: Patterns of management of rash associated with epidermal growth factor receptor inhibitors (EGFRIs): A national practice survey (abstract 14081). J Clin Oncol 25(suppl 18S), 2007 (slide presentation available at www.asco.org).
2. Wagner L, Lai S, Aneja P, et al: Development of a functional assessment of side effects to therapy (FAST) questionnaire to assess dermatology-related quality of life in patients treated with EGFR inhibitors (EGFRIs): The FAST-EGFRI (abstract 19532). J Clin Oncol 25(suppl 18S), 2007 (slide presentation available at www.asco.org).
3. Shepherd F, Rodrigues P, Ciuleanu T, et al: Erlotinib in previously treated non-small cell lung cancer. N Engl J Med 353:123-132, 2005.
4. Cunningham D, Humblet Y, Siena S, et al: Cetuximab monotherapy and cetuximab plus irinotecan in irinotecan-refractory metastatic colorectal cancer. N Engl J Med 351:337-345, 2004.
5. Lacouture M, Basti S, Patel J, et al: The SERIES clinic: An interdisciplinary approach to the management of toxicities of EGFR inhibitors. J Support Oncol 4:236-238, 2006.
6. Shah N, Kris M, Pao W, et al: Practical management of patients with non-small cell lung cancer treated with gefitinib. J Clin Oncol 23:165-174, 2005.
7. Brazzini B, Pimpinelli N: New and established topical corticosteroids in dermatology: Clinical pharmacology and therapeutic use. Am J Clin Dermatol 3:47-58, 2002.
8. Alexandrescu D, Vaillant J, Dasanu C: Effect of treatment with a colloidal oatmeal lotion on the acneform eruption induced by epidermal growth factor receptor and multiple tyrosine-kinase inhibitors. Clin Exp Dermatol 32:71-74, 2007.
9. Cortesi E, DePasquale C, D'Auria G, et al: management of cutaneous adverse effects during treatment with ZD1838 in advanced non-small cell lung cancer (NSCLC): surprising efficacy of early local treatment (abstract 7100). Proc Am Soc Clin Oncol 23:628, 2004 (slide presentation available at www.asco.org).
10. Lee H, Ciancio S, Tuter G, et al: Subantimicrobial dose doxycycline efficacy as a matrix metalloproteinase inhibitor in chronic peridontitis patients is enhanced when combined with a non-steroidal anti-inflammatory drug. J Periodontol 75:453-463, 2004.
11. Neiman G, Zerler B: A role for the anti-inflammatory properties of tetracyclines in the prevention of acute lung injury. Curr Med Chem 8:317-325, 2001.
12. Golub L, Lee H, Ryan M, et al: Tetracyclines inhibit connective tissue breakdown by multiple non-antimicrobial mechanisms. Adv Dent Res 12:12-26, 1998.
13. Lynch TJ, Kim ES, Eaby B, et al: Epidermal growth factor receptor inhibitor-associated cutaneous toxicities: an evolving paradigm in clinical management. Oncologist 12:610-621, 2007.
14. Gutzmer R, Werfel T, Mao R, et al: Successful treatment with oral isotretinoin of acneiform skin lesions associated with cetuximab therapy. Br J Dermatol 153:849-851, 2005.
15. Jacot W, Bessis D, Lorda E, et al: Acneiform eruption induced by epidermal growth factor receptor inhibitors in patients with solid tumors. Br J Dermatol 151:238-241, 2004.
16. Fehrenbacher J, Taylor C, Vasko M, et al: Pregabalin and gabapentin reduce release of substance P and CGRP from rat spinal tissues only after inflammation or activation of protein kinase C. Pain 105:133-141, 2003.
17. Porzio G, Aielli F, Verna L, et al: Efficacy of pregabalin in the management of cetuximab-related itch. J Pain Symptom Manage 32:397-398, 2006.
18. Smit J, Bauland C, Wijnberg D, et al: Pulsed dye laser treatment, a review of indications and outcome based on published trials. Br J Plast Surg 58:981-987, 2005.
19. Lacouture M: Mechanisms of cutaneous toxicities to EGFR inhibitors. Nat Rev Cancer 6:803-812, 2006.
20. Lacouture M, Lai S: The PRIDE (Papulopustules and/or paronychia, Regulatory abnormalities of hair growth, itching, and dryness due to epidermal growth factor receptor inhibitors) syndrome. Br J Dermatol 155:852-854, 2006.
21. Jatoi A, Rowland K, Sloan JA, et al: Does tetracycline prevent/palliate epidermal growth factor receptor (EGFR) inhibitor-induced rash? A phase III trial from the North Central Cancer Treatment Group (N03CB). J Clin Oncol 25(18S):494s, 2007 (abstract LBA9006).
22. Agero AL, Scope A, Myskowski P, et al: Prophylaxis with systemic minocycline and topical tazarotene for the cetuximab associated acne-like eruption (abstract). J Am Acad Dermatol 56:508, 2007 (abstract 42).
Oncology Peer Review On-The-Go: Cancer-Related Fatigue Outcome Measures in Integrative Oncology
September 20th 2022Authors Dori Beeler, PhD; Shelley Wang, MD, MPH; and Viraj A. Master, MD, PhD, spoke with CancerNetwork® about a review article on cancer-related fatigue published in the journal ONCOLOGY®.
Late Hepatic Recurrence From Granulosa Cell Tumor: A Case Report
Granulosa cell tumors exhibit late recurrence and rare hepatic metastasis, emphasizing the need for lifelong surveillance in affected patients.