Data Support Chemo for All Young Breast Cancer Patients
ATLANTA-All breast cancer patients under age 35 should be offered adjuvant chemotherapy even if they have low-risk disease, Mads Melbye, MD, PhD, said at the Era of Hope: U.S. Department of Defense Breast Cancer Research Program Meeting.
ATLANTAAll breast cancer patients under age 35 should be offered adjuvant chemotherapy even if they have low-risk disease, Mads Melbye, MD, PhD, said at the Era of Hope: U.S. Department of Defense Breast Cancer Research Program Meeting.
He presented results of a 10,000-patient retrospective study from Denmark to support the recommendation.
In this study, without follow-up chemotherapy, women under age 35 with low-risk disease were more than twice as likely to die of their disease as comparable patients aged 45 to 49 at diagnosis. In contrast, among those receiving adjuvant chemotherapy, young women did not die more often than middle-aged women.
Dr. Melbye is professor of epidemiology research, Statens Serum Institut, Copenhagen. He and his colleagues reviewed data from a population-based registry, maintained by the Danish Breast Cancer Cooperative Group since 1977, of 10,356 women who were less than 50 years of age when diagnosed with breast cancer.
The largest group was 4,402 women in the 45 to 49 age range, which the researchers set as the reference. The main outcome measure was the risk of dying within the first 10 years after diagnosis, adjusted for known prognostic factors and expected mortality.
Our detailed information on tumor characteristics at diagnosis enabled us to adjust for the effect of factors such as tumor size, nodal status, and histologic grade, and therefore judge more clearly the independent effect of age, Dr. Melbye commented.
Overall, the researchers found that the younger women had an elevated relative risk of dying; those under age 35 had the worst prognosis (relative risk, 1.46).
The researchers then examined risk of dying for different age groups among the 4,329 low-risk patients, none of whom received adjuvant chemotherapy, and among the 2,824 high-risk patients, all of whom received adjuvant chemotherapy.
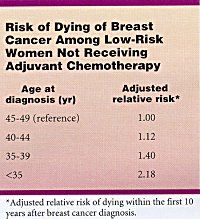
Among women with low-risk disease who received no adjuvant cytotoxic treatment, the risk of dying increased significantly with decreasing age at diagnosis (see Table). The researchers did not see a similar trend for younger women in the high-risk group who did receive chemotherapy.
Following the conference, Dr. Melbye told ONI, I want to stress that this study was not planned as an intervention trial where one arm got chemo and the other did not. The data derive from a very large, population-based registry on all women in Denmark treated for breast cancer. Nevertheless, the findings are so robust that we believe most young women might benefit from cytotoxic treatment.
He then added, There is always a price to paythe risk that we will overtreat some women. At the moment, we can only point out to women the poor survival among low-risk patients who are not getting chemotherapy.
More precise knowledge would require a clinical trial, but that might be difficult to do, Dr. Melbye said, in light of the findings from this retrospective study and the fact that breast cancer is rare among younger women, making it difficult to enroll sufficient patients.
Until this study, higher mortality rates in younger women were thought to be due to their having more aggressive tumors. Previous research had shown that younger breast cancer patients were more likely to have affected lymph nodes, be negative for estrogen receptors, and have tumors that are large with a high grade of anaplasia. Yet Dr. Melbyes group found that use of adjuvant chemotherapy was more important than age in determining outcomes.
No matter how we examine the data, the conclusions are the same, he said. The researchers had the same results when they looked exclusively at women with node-negative disease and again when they looked only at women with small tumors (2 cm or less) or large tumors (greater than 2 cm) at the time of diagnosis.
Although the study included 867 women under age 35 at diagnosis, the sample was too small to compare outcomes with chemotherapy vs without chemotherapy in that age group.
A direct comparison of those below 35 years with and without chemotherapy was difficult to perform simply because the recommendations for low-risk disease patients until recently had been not to give systemic chemotherapy, Dr. Melbye said. Thus, his group looked at the age effect within the group of women who did not receive chemotherapy and the group who did.
We found a clear indication that age was unimportant in the chemotherapy group whereas among those low-risk women who did not receive chemotherapy, the young women did significantly poorer than comparable middle-aged women.
The full report of the study has been published in the British Medical Journal (320:474-479, 2000).