HER-2/neu Activation May Predict Breast Cancer Prognosis
ATLANTA-Overexpression of HER-2/neu may not be as critical to breast cancer prognosis as its activation, according to research reported by Michael P. DiGiovanna, MD, PhD, at the Era of Hope: U.S. Department of Defense Breast Cancer Research Program Meeting. Dr. DiGiovanna is assistant professor of medicine and pharmacology, Yale University School of Medicine.
ATLANTAOverexpression of HER-2/neu may not be as critical to breast cancer prognosis as its activation, according to research reported by Michael P. DiGiovanna, MD, PhD, at the Era of Hope: U.S. Department of Defense Breast Cancer Research Program Meeting. Dr. DiGiovanna is assistant professor of medicine and pharmacology, Yale University School of Medicine.
HER-2/neu, a growth factor receptor protein, is overexpressed in about 30% of breast cancers, and its overexpression has been considered a sign of poor prognosis. However, in Dr. DiGiovannas review of 816 breast cancer cases, only those with the activated protein had poorer outcomes (disease-free survival and disease-specific overall survival).
We actually found activation in the minority of overexpressed cases, Dr. DiGiovanna said in an interview with ONI. The most important take-home message of my research is that overex-pression itself may not be the important factor. The most important factor may be the activation state.
The researchers also found a strong correlation between phosphorylated HER-2/neu (PNeu), the proteins activated form, and expression of epidermal growth factor (EGF) receptor.
We know the EGF receptor itself can activate HER-2/neu, Dr. DiGiovanna said. Potentially, drugs that inhibit EGF receptor might be a good regimen for breast cancer in clinical trials.
Dr. DiGiovanna used a database provided by Ann D. Thor, MD, a pathologist at Evanston Northwestern Healthcare and Northwestern University, Evanston, Illinois. The cases were diagnosed between 1976 and 1983 with a median follow-up of 16.3 years.
Detectable PNeu
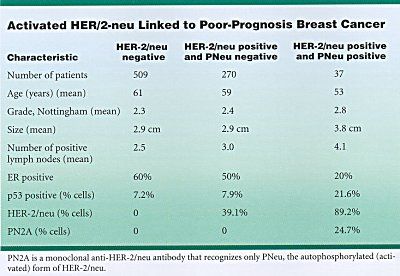
While 307 of the 816 cases (38%) showed overexpressed HER-2/neu, only 37 of these (12% or 5% of the total) had detectable PNeu. This group had clinical features linked to poor prognosis (see Table), and follow-up showed that these patients did, in fact, have a poorer outcome than those without detectable PNeu.
PNeu was associated with a higher percentage of HER-2/neu-positive cells in the tumor, higher number of involved lymph nodes, estrogen-receptor (ER) negativity, and abnormal copies of the tumor-suppressor gene p53.
In contrast, women with high levels of inactive HER-2/neu had clinical profiles associated with less aggressive tumors, similar to those of women with normal levels of HER-2/neu.
If this work holds up after larger follow-up studies, it may help guide treatment choices for women with breast cancer, Dr. DiGiovanna said. For example, it may help determine which women need adjuvant therapy and the aggressiveness of that treatment.
Three New Studies
As a result of the study, three new breast cancer trials at Yale are focusing on women with overexpressed and activated HER-2/neu. The first asks whether these women have a worse response to tamoxifen than do those without overexpressed and activated HER-2/neu.
The second explores whether they respond better to trastuzumab (Herceptin), a monoclonal antibody that interferes with the functioning of HER-2/neu. The third asks whether they respond differently to CAF (cyclophosphamide, Adriamycin, 5-fluorouracil).
Tumors that overexpress HER-2/neu are better treated by CAF than other therapies, Dr. DiGiovanna said. Again, we are going to do a retrospective study to see whether the activated state of HER-2/neu really makes a difference.
Among the overall questions still to be answered is why HER-2/neu would be overexpressed but not activated in some breast cancers. I suspect a continuum of activation, said Dr. DiGiovanna, who created a monoclonal antibody that detects PNeu (PN2A) for use in the study. Our test probably discriminated those with a low level of activation from those with a high level of activation.
One possibility, he suggested, is that overexpression may be important at the start of the cancer process. Weve known for a time that overexpression is more common in ductal carcinoma in situ [DCIS] than in invasive breast cancer. We dont understand what that means; we only have theories, he said. Maybe it means that HER-2 is very active in the genesis of a tumor.