Even Insured Cancer Patients May Stumble Over Co-pays and Drug Costs
Jeff Kranau’s story is a moving one but, during this economic downturn, not necessarily a unique one. The former South Florida salesman was successfully treated for squamous cell carcinoma of the larynx in 2009 and declared cancerfree. But what should have been a reason for celebration has, over time, sent Mr. Kranau’s life into a tailspin.
Financial assistance is available, but patients may need help negotiating the system.
Jeff Kranau’s story is a moving one but, during this economic downturn, not necessarily a unique one. The former South Florida salesman was successfully treated for squamous cell carcinoma of the larynx in 2009 and declared cancerfree. But what should have been a reason for celebration has, over time, sent Mr. Kranau’s life into a tailspin.
“I now have a permanent hole in my vocal cords from the radiation, which makes it quite difficult for me to project my voice any louder than a loud whisper. Part of my job involved taking potential sales calls and answering questions for customers over the phone,” Mr. Kranau told Oncology News International. “Obviously, I am no longer able to do that.”
Mr. Kranau eventually left his job and, subsequently, lost coverage for the multiple medications he needs to ease his postchemoradiotherapy complications. “Without insurance, I am in need of funds for help with medical bills and, most importantly, my medications, which I can no longer afford,” he said.
The ranks of the uninsured or underinsured have been on the rise, placing a burden on cancer patients and the programs that dispense treatment. A national poll conducted by the American Cancer Society Cancer Action Network found that, over the past two years, nearly one-half of cancer patients and survivors under age 65 said they are having difficulty affording healthcare costs, including paying for copays and prescription drugs (ACS CAN poll results, June 23, 2010).
As a result, one in three patients under age 65 diagnosed with cancer delayed needed cancer-related tests, treatments, checkups, and filling of prescription drugs over the past year.

Another survey by the Association of Community Cancer Centers (ACCC) found that patients over the past two years are increasingly asking treatment facilities for help with the cost of co-pays, prescription drug costs, and transportation.
“If you speak to oncologists, threequarters of the doctors in community practices in 2010 had seen the direct impact of the recession,” said Lee Blansett, senior vice president of Oncology Market Access for Kantar Health, based in Foster City, Calif. “Chief among those impacts was patients’ inability to pay for cancer treatments and, in some cases, an increasing number in whom treatment selection was based on the ability to pay.”
Mr. Blansett added that data prior to the recession were already showing a trend toward increased number of uninsured and underinsured patients, and he suggested that this trend will continue even if the recession is officially declared to be over.
• American Cancer Society Health Insurance and Financial Assistance
www.cancer.org/Treatment/FindingandPayingforTreatment/ManagingInsuranceIssues/ HealthInsuranceandFinancialAssistancefortheCancerPatient/index
• CancerCare
www.cancercarecopay.org/about.html
• Chronic Disease Fund
www.gooddaysfromcdf.org/patients/process
• Cancer Fund of America
www.cfoa.org
• Cancer Support Community/The Wellness Community
www.thewellnesscommunity.org/
• HealthWell Foundation
www.healthwellfoundation.org/
• Patient Advocate Foundation
www.patientadvocate.org
• Susan G. Komen for the Cure
www.komen.org
• Surgery on a Sunday
www.surgeryonasunday.org
• Life Beyond Cancer Foundation
www.lifebeyondcancer.org

Lee Blansett
Centralized support
For some independent practices, the most efficient way to manage uninsured or underinsured patients is to refer them to hospitals.
“Hospitals have more resources and revenue streams and therefore may also be better at organizing patient assistant programs,” Mr. Blansett said.
But that may place an undue strain on hospitals, which could come back to haunt a community practice that is in partnership with a larger facility. “We have been loath to send our patients to hospitals,” said Leonard Kalman, MD, an oncologist at Advanced Medical Specialties in Miami. “Hospitals are our partners so we don’t want to put a financial burden on them.”
• NCI Resources for Financial Assistance
https://cissecure.nci.nih.gov/factsheet/ FactSheetSearch8_3.aspx
• U.S. Department of Health and Human Services:
Agency for Healthcare Research and Quality
www.ahcpr.gov/consumer
• Hill-Burton Facilities Compliance & Recovery
www.hrsa.gov/gethealthcare/affordable/ hillburton/compliance.html
Advanced Medical Specialties is a member of the United Network of US Oncology, which offers its partners access to a centralized Patient Assistance Support (PAS) program designed to streamline the process for patients and clinics to gain access to needed funds.
Clinics within the United Network of US Oncology are encouraged to refer their underinsured and uninsured patients to the PAS program, where a centralized staff can help maneuver a patient through the often dense and difficult process of locating and applying for financial assistance, said Sharon Roeder, director of the United Network of US Oncology PAS program.
“For example, for a patient with breast cancer, there are multiple places to get help, including nonprofit charitable organizations,” she said (see Table 1). The program has minimized the need for community clinics in the United Network of US Oncology to refer patients in need to hospitals, Ms. Roeder added. She said that in 2010, the United Network of US Oncology PAS program served on average 130 more patients per month than in 2009.
Dr. Kalman said the PAS program has been a boon to the clinic and the patients: The latter benefit from getting the right treatment at the right time while the clinic maintains financial viability. “So far, from January through August of this year, our practice was able to obtain $1 million to cover co-pays that were not covered through insurance,” Dr. Kalman said.


Sharon Roeder Michele Mccourt
Nonprofit support
Where can cancer centers that don’t have the backing of the United Network of US Oncology send their patients for assistance? A network of nonprofit organizations exists to help patients with financial assistance, and CancerCare is at the forefront of this movement (see Tables 1-3).
In 2007, CancerCare established the CancerCare Co-Payment Assistance Foundation to help eligible patients obtain funding for their cancer treatment. Patients with an annual income up to four times the federal poverty level (eg, $58,280 for a family of two) are eligible for the program, said Michele McCourt, program director.
“Once approved, we attempt to work directly with the pharmacy or healthcare provider to set up a third-party billing process to bill us directly for the chemotherapy co-payments that the client would be responsible for,” Ms. McCourt said. “For payments, we require a health insurance claim form showing the date of service, a description of the medication, the quantity dispensed, the amount charged, the amount paid by the insurance provider, and the amount that is the patient’s responsibility.”
• Air Charity Network
www.aircharitynetwork.org
• Corporate Angel Network
www.corpangelnetwork.org
• National Patient Air Travel Helpline
www.patienttravel.org
• Raquel’s Wings for Life
www.raquelswingsforlife.com
The program only assists insured patients with their chemotherapy copayments, she added. No support is provided for drugs taken to manage symptoms.
A number of government-sponsored programs also exist to help patients find funding, said Allison Miller, media advocacy coordinator for the ACS Midwest division. The ACS Patient Navigator Program helps connect patients with local navigators at cancer treatment centers throughout the country to help with cost and insurance issues. Patients can also access the Health Insurance Assistance Service through the ACS that connects patients with health insurance specialists. More than 25,000 cases from 39 states have been addressed by this service to date, Ms. Miller said.
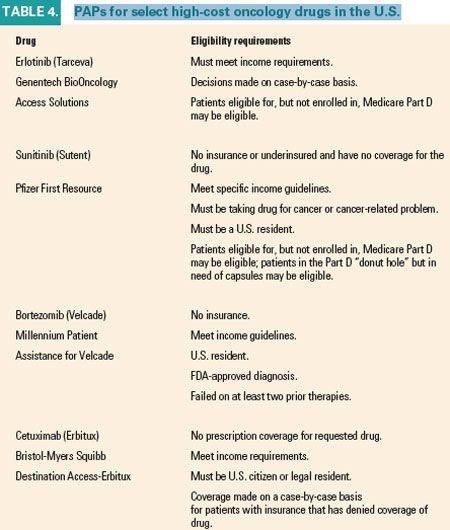
In addition to all of these programs are the patient assistance programs (PAPs) through the pharmaceutical companies. Many of these programs will waive the cost of drugs for patients in need, provided they meet specific criteria (see Table 4).
Gedatolisib Combo With/Without Palbociclib May Be New SOC in PIK3CA Wild-Type Breast Cancer
December 21st 2025“VIKTORIA-1 is the first study to demonstrate a statistically significant and clinically meaningful improvement in PFS with PAM inhibition in patients with PIK3CA wild-type disease, all of whom received prior CDK4/6 inhibition,” said Barbara Pistilli, MD.