Exercise Treatment as Part of Multidisciplinary Whole Person Care in Oncology
Neil M. Iyengar, MD, highlights how to best integrate exercise oncology into multidisciplinary care.
Neil M. Iyengar, MD
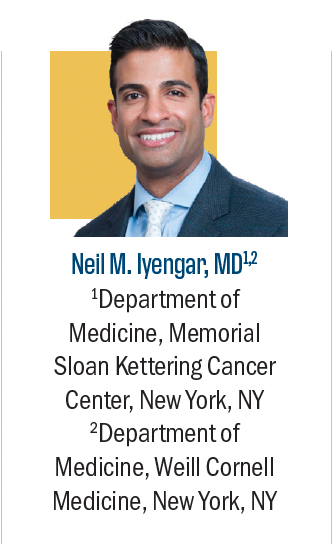
Several national agencies, including the American Society of Clinical Oncology (ASCO), recommend the prescription of exercise for patients diagnosed with cancer.1,2 The evidence base for this recommendation is derived from studies that showed exercise-related improvements in patient-reported outcomes (PROs), treatment-associated adverse effects, cardiorespiratory fitness (CRF), and overall physical functioning.3-6 Additionally, exercise may have direct anticancer effects and indirect effects by synergizing standard cancer therapies.7,8 Despite these benefits, the implementation of exercise oncology practice guidelines in the United States has been limited. A major barrier to the implementation of exercise therapy and other “whole person interventions” is the increasing complexity of clinical decision-making due to the greater availability of novel cancer therapeutics with clinical benefits ranging from low to high impact.
The associated decision-making paradigm requires highly nuanced conversations, planning, and more time for discussion between patients and their oncologists to develop an efficacious treatment approach that aligns with patient priorities while balancing potential toxicity. Within this context, the consideration of any additional treatment recommendation, such as exercise, is scrutinized against competing priorities to maximize clinical efficiency. Questions regarding the optimal use of exercise (eg, when to implement, type, and dosage of exercise) have made it challenging to prescribe exercise as part of a cancer treatment plan, relegating exercise to the realm of “general recommendations” that are mentioned but often forgotten.
Fortunately, guidelines from ASCO and the American College of Sports Medicine now include important details for exercise therapy implementation such as established safety and dosing information.2 Several randomized control trials have demonstrated that exercise after completion of cancer therapy improves various PROs and CRF.3,4 Additional studies have demonstrated that supervised exercise during chemotherapy is safe and tolerable.9 Supervised exercise during chemotherapy also has early efficacy for mitigating chemotherapy-related decline in CRF.10 Patients who initiate exercise after chemotherapy may also regain CRF and physical function to the same degree as those who started exercise during chemotherapy, which provides flexibility for patients unable to exercise. Exercise is also efficacious for improving fatigue, PROs, and other cancer-related symptoms in the setting of multimodality therapy such as chemoradiation.10 Taken together, the extant data indicate that exercise may be implemented at nearly any point during the cancer treatment spectrum with favorable effects.
Adherence and tolerability are critical factors that impact the feasibility and efficacy of exercise therapy, perhaps even more so than pharmacologic therapies. For example, CRF recovery in patients who start supervised exercise after completing chemotherapy has been shown to catch up with that of patients who start exercise during chemotherapy but transition to home-based exercise after chemotherapy.10 These findings suggest the superiority of supervised exercise over home-based exercise, though maintaining adherence can be a challenge. In this regard, smartphone mobile applications and other virtual/remote platforms could provide a scalable digital solution. Our group at Memorial Sloan Kettering Cancer Center recently demonstrated high engagement among survivors of breast cancer with a commercially available smartphone application that led to an average weight loss of approximately 5% of baseline weight.11
In addition to smartphone applications, several existing web-based programs may be leveraged for patients with cancer. For example, the SurvivorSHINE program utilizes web-based diet and exercise counseling and has been shown to improve diet quality, increase physical activity, and reduce functional decline in cancer survivors.12,13 The intervention consists of an interactive online program that has been subjected to rigorous formative research (focus groups, extensive beta testing, and stakeholder interviews) in diverse samples that informed and refined the yearlong intervention.14 Website engagement data show weekly logins that are 2- to 3-fold higher than online lifestyle interventions of similar duration that are not tailored to oncology populations. Another important resource for implementing lifestyle interventions is the American Institute for Cancer Research, which offers continuous updates from published data and patient-facing educational information regarding diet and exercise.
Efforts are underway to include exercise oncology as a reimbursable service for cancer care. The success of such efforts stands to have a large potential impact on the availability and accessibility of exercise programs for patients with cancer throughout the US. Until exercise oncology programs become more accessible, it is our responsibility as oncologists to endorse the inclusion of exercise as part of cancer therapy and guide patients to appropriate resources. For now, the use of digital and web-based platforms provides an implementable and convenient approach to incorporating exercise therapy as part of whole-person care in oncology.
References
- Ligibel JA, Bohlke K, May AM, et al. Exercise, diet, and weight management during cancer treatment: ASCO guideline. J Clin Oncol. 2022;40(22): 2491-2507. doi:10.1200/JCO.22.00687
- Campbell KL, Winters-Stone K, Wiskemann J, et al. Exercise guidelines for cancer survivors: consensus statement from International Multidisciplinary Roundtable. Med Sci Sports Exerc. 2019;51(11):2375-2390. doi:10.1249/MSS.0000000000002116
- Furmaniak AC, Menig M, Markes MH Exercise for women receiving adjuvant therapy for breast cancer. Cochrane Database Syst Rev. 2016;9(9):CD005001. doi:10.1002/14651858.CD005001.pub3
- Yunfeng G, Weiyang H, Xueyang H, Yilong H, Xin G. Exercise overcome adverse effects among prostate cancer patients receiving androgen deprivation therapy: an update meta-analysis. Medicine (Baltimore). 2017;96(27):e7368. doi:10.1097/MD.0000000000007368
- Scott JM, Zabor EC, Schwitzer E,et al. Efficacy of exercise therapy on cardiorespiratory fitness in patients with cancer: a systematic review and meta-analysis. J Clin Oncol. 2018;36(22):2297-2305. doi:10.1200/JCO.2017.77.5809
- Mishra SI, Scherer RW, Snyder C, Geigle PM, Berlanstein DR, Topaloglu O. Exercise interventions on health-related quality of life for people with cancer during active treatment. Cochrane Database Syst Rev. 2012;2012(8):CD008465. doi:10.1002/14651858.CD008465.pub2
- Iyengar NM, Jones LW. Development of exercise as interception therapy for cancer: a review. JAMA Oncol. 2019;5(11):1620-1627. doi:10.1001/jamaoncol.2019.2585
- Koelwyn GJ, Quail DF, Zhang X, White RM, Jones LW. Exercise-dependent regulation of the tumour microenvironment. Nat Rev Cancer. 2017;17(10):620-632. doi:10.1038/nrc.2017.78
- Scott JM, Lee J, Herndon JE,et al. Timing of exercise therapy when initiating adjuvant chemotherapy for breast cancer: a randomized trial. Eur Heart J. 2023;44(46):4878-4889. doi:10.1093/eurheartj/ehad085
- van der Schoot GGF, Ormel HL, Westerink NL, et al. Optimal timing of a physical exercise intervention to improve cardiorespiratory fitness: during or after chemotherapy. JACC CardioOncol. 2022;4(4):491-503. doi:10.1016/j.jaccao.2022.07.006
- Shen S, Salehi E, White C, Chen Y, Iyengar NM. Evaluation of a mobile behavior change program for weight loss in breast cancer survivors. NPJ Breast Cancer.2024;10(1):53. doi:10.1038/s41523-024-00659-x
- Pekmezi D, Fontaine K, Rogers LQ,et al. Adapting MultiPLe behavior Interventions that eFfectively Improve (AMPLIFI) cancer survivor health: program project protocols for remote lifestyle intervention and assessment in 3 inter-related randomized controlled trials among survivors of obesity-related cancers. BMC Cancer. 2022;22(1):471. doi:10.1186/s12885-022-09519-y
- Williams VA, Brown NI, Johnson R,et al. A web-based lifestyle intervention for cancer survivors: feasibility and acceptability of SurvivorSHINE. J CancerEduc. 2022;37(6):1773-1781. doi.10.1007/s13187-021-02026-x
- Ivankova NV, Rogers LQ, Herbey II,et al. Features that middle-aged and older cancer survivors want in web-based healthy lifestyle interventions: qualitative descriptive study. JMIR Cancer. 2021;7(4):e26226. doi:10.2196/26226
How Supportive Care Methods Can Improve Oncology Outcomes
Experts discussed supportive care and why it should be integrated into standard oncology care.