Quadruplet Therapy May Be the New Frontline SOC in Multiple Myeloma
Quadruplet therapy is making a run to be a potential standard of care in frontline multiple myeloma, according to a panel of experts.
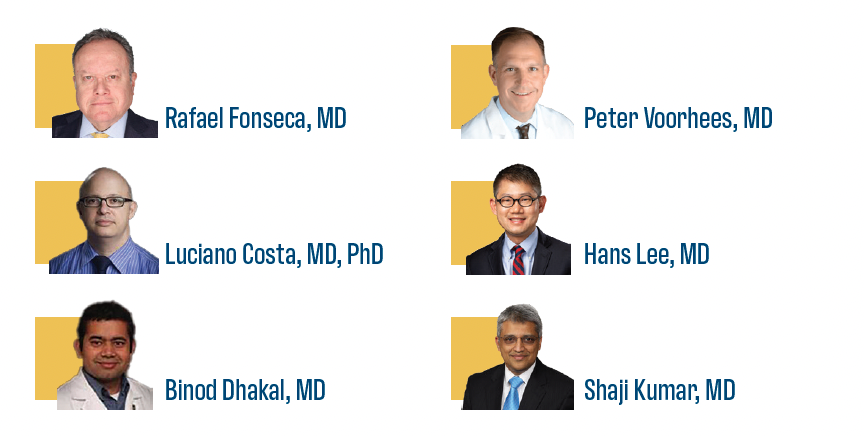
The expert panel.
During the 2024 European Hematology Association (EHA) Congress, experts in the field of multiple myeloma sat down to discuss the effect of earlier lines of
therapy on the disease.
The panel was led by Rafael Fonseca, MD, director for innovation and transformational relationships at Mayo Clinic in Arizona. He was joined by Luciano Costa, MD, PhD, professor at the University of Alabama at Birmingham, Heersink School of Medicine; Binod Dhakal, MD, associate professor at the Medical College of Wisconsin; Peter Voorhees, MD, professor and director of outreach services at Levine Cancer Institute, Atrium Health; Hans Lee, MD, associate professor in the Department of Lymphoma/Myeloma, Division of Cancer Medicine, The University of Texas MD Anderson Cancer Center; and Shaji Kumar, MD, a hematologist from Mayo Clinic.
The conversation focused on frontline therapy, CAR T-cell therapy, and updated trial results. Additionally, the panelists could cover any data that emerged from EHA or the 2024 American Society of Clinical Oncology (ASCO) Annual Meeting.
Earlier-Line Options for Newly Diagnosed Multiple Myeloma
The PERSEUS Trial
The panel discussed the phase 3 PERSEUS trial (NCT03710603), which assessed the use of daratumumab (Darzalex) plus bortezomib (Velcade), lenalidomide (Revlimid), and dexamethasone (D-VRd) vs VRd for patients with transplant-eligible newly diagnosed multiple myeloma.1
Updated data found the minimal residual disease (MRD) rate at 10–6 was 34.4% and at 10–5 it was 57.5% for the end of consolidation in the D-VRd arm vs 16.1% and 32.5% in the VRd arm. Additional results were assessed up to 12 months were 43.9% and 65.1% vs 20.9% and 38.7%; up to 24 months it was 57.7% and 72.1% vs 27.4% vs 44.9%; and up to 36 months it was 63.9% and 74.6% vs 30.8% and 46.9% in the D-VRd and VRd arms, respectively.
While presenting these data, Fonseca noted that when a patient enters MRD, it becomes a major marker for good long-term outcomes. When the floor was opened to comments, the panel chimed in about the use of MRD and quadruplets in the space.
“We’re at a point now where induction therapy is so good that using MRD negativity at 10–5 is going to become increasingly difficult because there’s going to be such a high percentage of patients who achieve it. There’s no question that [quadruplet therapies] are the preferred standard for patients who are fit or transplant eligible.”
Costa noted that MRD plays a large role in determining outcomes. He believes that as trials develop and initial efficacy data emerge, the standard of care (SOC) may change, and it will help clinicians to adapt.
Fonseca asked Dhakal which patient populations, if any, should be treated with a triplet regimen vs a quadruplet.
“That is an important question for patients who are older than 80 years,” Dhakal said. “In my clinical practice, if I have to choose a regimen for a patient who is older than 80 years, unless they are ultra-high risk, I would be more inclined to choose just DRd-based regimens.” He tries to avoid bortezomib as it comes with increased neuropathy.
Lee believes that quadruplet therapies are superior to triplets but would prefer to think of the question as who is more eligible for a quadruplet vs a triplet. “If they’re eligible to receive 4 drugs, they should receive 4 drugs whether they’re transplant eligible or ineligible. If they’re triplet eligible, the favored regimen would be the DRd regimen because it’s so well tolerated.”
Lee wondered if adding daratumumab to lenalidomide maintenance as seen in PERSEUS and the phase 2 GRIFFIN trial (NCT02874742) yielded positive efficacy.2 He believes the results observed especially from PERSEUS with the MRD data show a benefit to the population.
Kumar thinks of the daratumumab plus lenalidomide maintenance therapy as a package and continues with it after transplant. He believes there is knowledge missing on how to effectively use this treatment.
The CASSIOPEIA Trial
The next trial of discussion was the phase 3 CASSIOPEIA trial (NCT02541383). The trial assessed bortezomib, thalidomide (Thalomid), and dexamethasone (VTd) with or without daratumumab (D-VTd) maintenance or observation for patients with transplant-eligible, newly diagnosed multiple myeloma.
Topline efficacy results included a median progression-free survival (PFS) from first randomization regardless of second randomization of 83.7 months
(95% CI, 70.2-not estimable) in the D-VTd group vs 52.8 months (95% CI, 47.5-58.7) in the VTd group (HR, 0.61; 95% CI, 0.52-0.72; P <.0001). The median overall survival from first randomization despite second randomization was not reached in either group, with 72-month rates of 86.5% (95% CI, 83.5%-89.3%) in the D-VTd group and 77.7% (95% CI, 73.9%-81.0%) in the VTd group.
A subgroup analysis was conducted to analyze the PFS of D-VTd maintenance vs D-VTd plus observation. The PFS was significantly longer in the maintenance group vs observation (HR, 0.76; 95% CI, 0.58-1.00; P = .048).
Looking at these data, Fonseca said he struggles with using maintenance and determining the amount of benefit a patient gets from it. Dhakal hypothesized based on the data presented that daratumumab maintenance will “win” as longer follow-up occurs. Following this treatment plan is also similar to what was discussed with PERSEUS.
“We’ve struggled with this question at our institution, and most of my colleagues use single-agent lenalidomide maintenance after induction and transplant therapy. The CASSIOPEIA data are starting to make me want to go back to the group and reevaluate how we approach this. In this analysis, the D-VTd followed by daratumumab was not compared with the VTd followed by daratumumab, where the PFS curves are similar, even with long-term follow-up,” said Voorhees.
Voorhees concluded that while these data were beneficial, it was not a home run.
CAR T-Cell Therapy Options
Quadruplet therapies are a big topic in the conversation about the use of CAR T-cell therapy. The phase 3 CARTITUDE-4 trial (NCT04181827) assessed ciltacabtagene autoleucel (cilta-cel; Carvykti) vs SOC for patients with functional high-risk multiple myeloma.3
In patients with 1 prior line of therapy and functional high-risk multiple myeloma, the overall response rate was 87.5% in the cilta-cel arm vs 79.5% in the SOC arm. The OR for a complete response or better was 3.3 (95% CI, 1.3-8.4; P = .0102).
The overall MRD negativity at the 10–5 threshold was 65.0% in the cilta-cel arm vs 10.3% in the SOC arm (OR, 16.3; 95% CI, 4.8-55.1; P <.0001).
Kumar often hesitates to use CAR T-cell therapy during a first relapse. Adding CAR T-cell therapy comes with increased toxicity, and Kumar sometimes does not want to interrupt the first or second progression-free interval with that.
“This is a very good clinical dilemma that I have in the clinic. If somebody is daratumumab naive, are you OK with giving these patients CAR T-cell therapy in the second line? Looking at the data, at face value, it looks solid, right? Because 25% of the patients there are exposed or refractory in CARTITUDE-4, and 75% are daratumumab naive, and they still did very well,” said Dhakal.
Voorhees uses cilta-cel depending on his patients as he worries about secondary malignancies and neurotoxicities. If a patient is standard risk, he prefers to look at other options. He believes the term functional high-risk needs a better definition so patients can be treated more accurately.
Lee believes more decisions can be made when additional CARTITUDE-4 data come out, and those who are functional high-risk should be prioritized for use with cilta-cel.
Kumar commented on the best time to sequence CAR T-cell therapy. “You have to start thinking about what we are going to give in the first-line therapy and second-line therapy that least impacts the ability of CAR T to give the maximum benefit. We don’t have much data at this point, but I think as we start dosing more and more patients in the first and second line, we’ll get a better sense of whether certain regimens used in the first and second line impact the outcome of the CAR T later.”
Looking Toward the Future
As the discussion ended, the panelists were asked how they hope to see the field evolve. Kumar wants to maximize the intensity of treatment in the up-front setting, specifically looking at quadruplets plus transplant. For those in the first relapse, CAR T-cell therapy can be considered, but in second relapse and beyond, the patient should be consulted, as it may impact their quality of life.
Dhakal highlighted that quadruplet regimens have cemented their positions in the newly diagnosed setting. He is still hesitant about the use of maintenance therapy, but the data with doublet maintenance seem promising. He is also keeping an eye on the B-cell maturation antigen setting, as it is an emerging field.
Costa agreed that more data and trials are needed for the maintenance setting so providers can provide clear and concrete answers to their patients.
For patients with standard-risk multiple myeloma, Voorhees believes the progress made there has been “phenomenal”; however, for those with ultra-high risk, a new regimen is essential.
Lee is looking forward to subset analyses for patients aged 65 to 75 years, as this is a gray area for data and how to treat the population.
Fonseca concluded that education in the community needs to be improved so that all patients are getting the same level of care.
References
- Rodriguez-Otero P, Moreau P, Dimopoulos MA, et al. Daratumumab (DARA) + bortezomib/lenalidomide/dexamethasone (VRd) in transplant-eligible (TE) patients (pts) with newly diagnosed multiple myeloma (NDMM): analysis of minimal residual disease (MRD) in the PERSEUS trial. J Clin Oncol. 2024;42(suppl_16):7502. doi:10.1200/JCO.2024.42.16_suppl.7502
- Voorhees PM, Sborov DW, Laubach J, et al. Addition of daratumumab to lenalidomide, bortezomib, and dexamethasone for transplantation-eligible patients with newly diagnosed multiple myeloma (GRIFFIN): final analysis of an open-label, randomised, phase 2 trial. Lancet Haematol. 2023;10(10):e825-e837. doi:10.1016/S2352-3026(23)00217-X
- Costa LJ, Weisel KC, van de Donk NWCJ, et al. Ciltacabtagene autoleucel vs standard of care in patients with functional high-risk multiple myeloma: CARTITUDE-4 subgroup analysis. J Clin Oncol. 2024; 42(suppl_16):7504. doi:10.1200/JCO.2024.42.16_suppl.7504
Navigating AE Management for Cellular Therapy Across Hematologic Cancers
A panel of clinical pharmacists discussed strategies for mitigating toxicities across different multiple myeloma, lymphoma, and leukemia populations.