Fiberoptic Ductoscopy for Nipple Discharge DisWomen With Nipple Discharge
SAN ANTONIO-By inserting a thin, hollow fiberoptic ductoscope through breast ducts in the nipple, physicians can examine the ductal system of the breast and accurately locate ductal lesions (see images).
SAN ANTONIOBy inserting a thin, hollow fiberoptic ductoscope through breast ducts in the nipple, physicians can examine the ductal system of the breast and accurately locate ductal lesions (see images).
"Fiberoptic ductoscopy allows direct visual access to the ductal system," said Kun-Wei Shen, MD, of the Cancer Hospital/Cancer Institute, Fudan University (formerly Shanghai Medical University). Dr. Shen presented the research at the 23rd Annual San Antonio Breast Cancer Symposium.
Fiberoptic Ductoscopy Allows Direct Visual Access to the Breast Ductal System
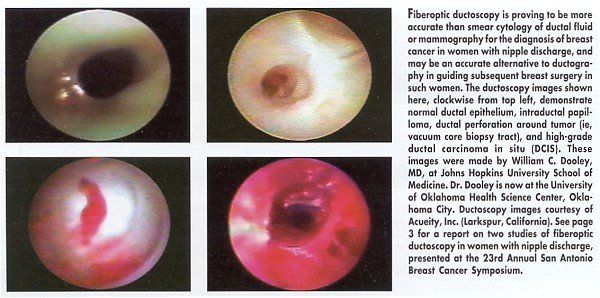
In this study of nearly 400 women with nipple discharge, fiberoptic ductoscopy was found to be more accurate than smear cytology of ductal fluid or mammography in diagnosing breast cancer associated with nipple discharge.
Although the study did not compare ductoscopy with ductography specifically, the researchers concluded that fiberoptic ductoscopy is a safe alternative to ductography in guiding subsequent breast surgery in women with nipple discharge.
The ductoscope used in this study (manufactured by Fujikura Co., Tokyo) is 6.5 cm long with a tip 0.72 mm in diameter. It contains a light source and a camera. In the study, the procedure took 20 minutes and was simple to do even on nulliparous women. This is because in women with nipple discharge, the ducts are dilated due to the abnormality causing the discharge, Dr. Shen said.
The most common cause of nipple discharge in study participants was a papillary lesion. "The ductal wall is pale yellow or pink," Dr. Shen said. "You can sometimes see the papillary vessel in the wall." Another common finding in patients was "fibrous bridging," which is a product of inflammatory changes, he said.
The study enrolled 382 women with spontaneous nipple discharge between October 1997 and December 1999. The study subjects underwent fiberoptic ductoscopy, ductal washings, and subsequent cytology of the ductal fluid.
In 174 (45.5%) of these women, the procedure was successful in visualizing an intraductal papillary lesion. Of these cases, 80.5% (140) had a single papilloma, 17.8% (31) had multiple discrete papillomas, and 1.7% (3) had diffuse intraductal thickening that corresponded to diffuse papillomatosis on histopathologic analysis.
The sensitivity of fiberoptic ductoscopy to diagnose breast cancer in women with nipple discharge compared very favorably with that of smear cytology and mammography, Dr. Shen said. Ten women were diagnosed with cancer after ductoscopy with one false positive (sensitivity, 91%). By comparison, the sensitivity of smear cytology was 73% and of mammography, less than 40%.
The overall positive predictive value of fiberoptic ductoscopy screening was 83%. The presence of clumps (more than 50 ductal cells) in the ductal washings combined with a positive fiberoptic ductoscopy examination increased the positive predictive value of the screening to 90%. The clumps are assumed to reflect the exfoliation of an intraductal papillary lesion.
Of the lesions observed, 37.6% were located in the main (segmental) duct, 35.3% in the first branch, 21.6% in the second branch, 4.5% in the third branch, and 0.9% in the fourth branch, with an overall average distance of 2.54 cm from the nipple orifice. Lesions that were missed by fiberoptic ductoscopy were missed either because they were beyond the reach of the ductoscope or the researcher failed to visualize a duct, Dr. Shen said.
US Study
In a poster presentation at the San Antonio symposium, Jill R. Dietz, MD, and her colleagues at the Cleveland Clinic Foundation, described their phase I study using the Acueity mammary ductoscope (Acueity, Inc., Larkspur, California) in 51 patients with pathologic nipple discharge prior to ductal excision.
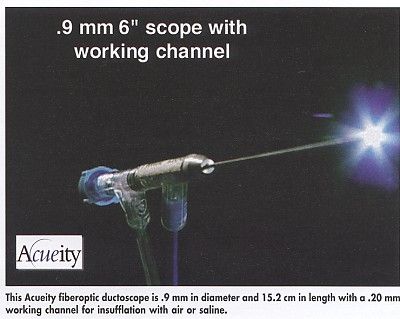
The Acueity system used in this study consists of a viewing screen and a 1.2 mm rigid microendoscope that houses a .08 mm optical channel and a .35 mm working channel for irrigation and introduction of therapeutic tools. The company also now manufacturers a .9 mm rigid scope with a .20 mm working channel (see Figure).
Patients were given intravenous sedation and underwent a four-quadrant nipple block with local anesthesia prior to the procedure. "Ductoscopy was well tolerated by the conscious, sedated patient," Dr. Dietz said, with only one surgical complication (wound infection). Cannulation of the symptomatic duct was uniformly successful, she said. Visualization of the distal ductal system or of the lesion was possible in 48 of the 51 cases.
Localization of the pathology was achieved in 45 patients (88%), compared with 30 of 40 patients (75%) undergoing ductography. Ductoscopy allowed for localization of the abnormality in 9 of the 10 patients who had a nonlocalizing ductogram, Dr. Dietz said.
Intraductal papillomas with or without associated benign proliferative changes were identified in 36 patients (70%). Ductal carcinoma in situ (DCIS) was found in 5 patients (10%). Seven patients (14%) had intraductal epithelial hyperplasia with associated changes as the only finding. Six unsuspected lesions were found deep within the ductal system during ductoscopy.
When a lesion was identified, ductal washings were obtained for cytology, and a blue dye was instilled into the duct to assist the surgeon in visualizing the lesion during excision.
Dr. Dietz concluded that ductoscopy is safe and feasible in the conscious sedated patient. She is currently testing the feasibility of the procedure in the office setting.