Glutamine Supplementation Could Reduce Toxicities of Treatment
INDIANAPOLIS-"Preclinical models suggest a role for glutamine supplementation in patients with cancer, but confirmation of clinical efficacy is needed," according to Patrick J. Loehrer, Sr., MD. "Glutamine plays an important and varied role in normal humans, and cancer significantly alters glutamine synthesis and catabolism," explained Dr. Loehrer, who is professor of medicine at Indiana University Medical Center in Indianapolis.
INDIANAPOLIS"Preclinical models suggest a role for glutamine supplementation in patients with cancer, but confirmation of clinical efficacy is needed," according to Patrick J. Loehrer, Sr., MD. "Glutamine plays an important and varied role in normal humans, and cancer significantly alters glutamine synthesis and catabolism," explained Dr. Loehrer, who is professor of medicine at Indiana University Medical Center in Indianapolis.
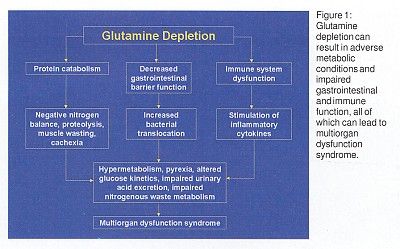
"Organs that regularly consume glutamine include the GI tract," he continued. Glutamine is an essential amino acid for growth of the gut epithelium, and human colon cancers use glutamine at a higher rate than normal tissue. Dr. Loehrer said that hepatic stores become depleted, which leads to cachexia, mucosal defects, and immune dysfunction (Figure 1).
Preclinical Studies
Preclinical studies showed that glutamine supplementation increased tumorocidal effect and decreased bacteremia and mortality in rats treated with methotrexate. Glutamine supplementation also improved villous height and decreased gut injury in radiation-treated rats.
"In tumor-bearing rats, glutamine supplementation increases glutathione levels, leading to increased chemosensitivity, decreased tumor expansion, and improved natural killer cell activity. Supplementation also increases intratumoral glutamine concentrations and may decrease methotrexate efflux. Data on mucositis and stomatitis are mixed, but there is an indication that glutamine reduces mucositis in dogs receiving radiation therapy," Dr. Loehrer said.
European researchers reported a study of fluorouracil (5-FU)-based therapy with or without glutamine in 24 patients with metastatic colorectal cancer (CRC). Supplementation was with parenteral glycyl-L glutamine. "There was no difference in clinical side effects, but a significant reduction in mucositis and ulcerations in the gastric mucosa and in the duodenal mucosa was seen in the glutamine group," Dr. Loehrer said. "The villous height/crypt depth ratio was also significantly greater in the glutamine group."
Prevention of Diarrhea
This has promising implications for prevention of diarrhea induced by irinotecan (Camptosar). "Up to 80% of patients have some degree of diarrhea, and there is a 10%-24% incidence of grade 4 diarrhea. Median time to onset of delayed diarrhea is 5 days in patients treated with irinotecan every 3 weeks or 11 days with weekly irinotecan," Dr. Loehrer said.
Management is most commonly with loperamide (Imodium). However, octreotide (Sandostatin), diphenoxylate HCl with atropine sulfate (Lomotil), and tincture of opium are also used sometimes.
"Glutamine and COX-2 inhibitors are also potential andiarrheal agents," Dr. Loehrer said. He described treatment of five patients with late-onset diarrhea from irinotecan who were treated again with irinotecan plus Glutamine Enriched Formula (Cambridge Nutraceuticals, Boston, Massachusetts). Patients were treated with a 10-gm packet PO every 8 hours for the first 48 hours after irinotecan treatment.
"Patients say the supplement makes them feel better and may improve their appetite," Dr. Loehrer said.
The Hoosier Oncology Group is following this up with a trial in patients with advanced colorectal cancer that includes both celecoxib and glutamine administration.