Ultrasound Contrast Agents Help Diagnose Prostate Cancer
BETHESDA, Maryland-Although many prostate cancers are not visible on conventional ultrasound, new methods of improving image contrast may allow better visualization and improved ultrasound-guided biopsy results in the next 3 to 5 years, Leonard G. Gomella, MD, said at a conference on urologic oncology sponsored by the National Cancer Institute (NCI) and the Society of Urologic Oncology.
BETHESDA, MarylandAlthough many prostate cancers are not visible on conventional ultrasound, new methods of improving image contrast may allow better visualization and improved ultrasound-guided biopsy results in the next 3 to 5 years, Leonard G. Gomella, MD, said at a conference on urologic oncology sponsored by the National Cancer Institute (NCI) and the Society of Urologic Oncology.
Gray-scale, transrectal ultrasound-guided (TRUS) biopsies are the gold standard of diagnostic tools for prostate cancer, but they have significant limitations, said Dr. Gomella, the Bernard W. Goodwin Jr., Associate Professor of Prostate Cancer, Thomas Jefferson University, and director of Urologic Oncology, Kimmel Cancer Center. He reported on work done in collaboration with radiologist Dr. Ethan Halpern.
For one thing, Dr. Gomella said, the ultrasound image contains 256 shades of gray, but the human eye is capable of resolving only 32 shades, meaning that image interpretation is subjective and depends greatly on the skill and experience of the operator. Thus, the technique is only 18% to 60% predictive of cancer, at present. "It’s scary to think that repeat sextant biopsies of known cancer patients are negative 31% to 45% of the time," he said.
The use of ultrasound contrast agents combined with gray-scale ultrasound could improve prostate cancer diagnosis, he said.
Such agents are marketed as Optison, Echogen, Sonovue, Imagent, and Definityand some have been approved by the Food and Drug Administration for use in echocardiography.
Now they are under intense study for enhancing visibility of malignant prostate neovascularity and producing 3-dimensional reconstructions of the prostate. They may also be useful for local drug delivery in the targeted organ.
At Thomas Jefferson University, Drs. Halpern and Gomella’s team compared conventional and contrast-enhanced ultrasound in 60 men with suspected prostate cancer. Biopsy showed prostate cancer in 37 sites from 20 patients. Standard gray-scale techniques found 14 cancer sites in 11 men, while ultrasound with contrast agents found 24 sites in 15 men. Sensitivity improved from 38% at base-line to 65% with contrast, he said, while specificity remained nearly the same (83% and 80%, respectively).
These contrast agents consist of small, gas-filled microbubbles, 1 to 10 microns in diameter, given as an IV bolus. They enhance parenchymal and vascular visualization.
They are, Dr. Gomella said, very safe, and should induce no fears of embolism. "The worst side effects thus far are tingling in the lips, although they are contraindicated for patients with shunting or atrial septal defects," he said.
The key to their use is the neovascularity associated with prostate cancer. "Neovessels are microvessels," he said. "While microvessel density studies focus on vessels less than 20 microns, we believe that the vessels seen by color Doppler studies using contrast agents are larger than 20 microns."
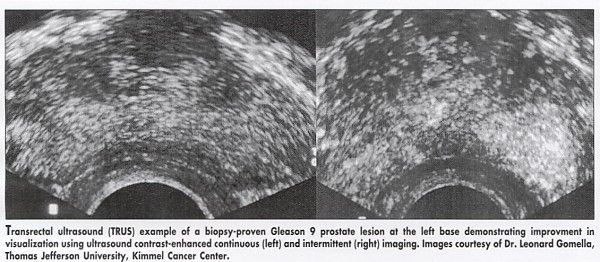
A problem associated with the use of contrast agents is that a continuous beam of ultrasound disrupts the bubbles. To eliminate this, Dr. Gomella suggests shifting to an "intermittent imaging" technique, in which the ultrasound turns on and off for brief periods. This allows the bubbles to get into the smaller vessels and permit imaging (see Figure).
The group is now working on finding the optimum sequence of times for intermittent imaging. A 0.5- to 1.0-second delay between pulses has provided good results so far, he said.
Adoption of the intermittent imaging technique may not involve buying a new ultrasound machine, Dr. Gomella said. Technicians can program their current software to produce the proper effect.
He noted that other ultrasound techniques such as compression of the prostate can also be used for elastography, that is, the mapping of prostate tissue stiffness. This is already the basis for the digital rectal examination, in which subtle differences in tissue stiffness make the cancers palpable.
Prolaris in Practice: Guiding ADT Benefits, Clinical Application, and Expert Insights From ACRO 2025
April 15th 2025Steven E. Finkelstein, MD, DABR, FACRO discuses how Prolaris distinguishes itself from other genomic biomarker platforms by providing uniquely actionable clinical information that quantifies the absolute benefit of androgen deprivation therapy when added to radiation therapy, offering clinicians a more precise tool for personalizing prostate cancer treatment strategies.