Hodgkin Lymphoma in Older Patients: An Uncommon Disease in Need of Study
Hodgkin lymphoma (HL) is one of the most curable malignancies in adults. However, survival rates for elderly patients with HL (often defined as ≥ 60 years of age) are inferior to those achieved by younger populations.
ABSTRACT: Elderly Hodgkin lymphoma (HL), commonly defined as occuring in patients over 60 to 65 years of age, is an uncommon disease. In population-based studies, the proportion of HL patients over age 60 years has ranged from 15% to 30%. However, the proportion of patients over age 60 years in clinical trials has been considerably lower, typically constituting Hodgkin lymphoma (HL) is one of the most curable malignancies in adults. However, survival rates for elderly patients with HL (often defined as ≥ 60 years of age) are inferior to those achieved by younger populations. The 5-year event-free survival or freedom from treatment failure rates for elderly HL range from 30% to 40%,[1-4] with 5-year overall survival rates ranging from 40% to 55%.[2-5] This compares to 5-year event-free survival rates of > 70% to 80% and overall survival rates of > 80% to 90% for patients aged < 40 years.[1,3-5]
Suboptimal staging and inadequate treatment delivery for older patients may compromise the rate of cure.[6,7] Furthermore, comorbidities may preclude the delivery of standard chemotherapy.[8,9] Intensive treatments such as BEACOPP (bleomycin, etoposide, doxorubicin [Adriamycin], cyclophosphamide, vincristine [Oncovin], procarbazine, and prednisone) are too toxic for older HL patients,[10] while bleomycin-containing regimens including ABVD (doxorubicin, bleomycin, vinblastine, dacarbazine) are often poorly tolerated.[4,7,11-14] Treatment delivery and comorbidity do not appear to completely explain the observed differences in outcome, however, implicating the biology of HL in the elderly.[15-17]
Elderly HL has been aptly described as an orphan disease,[18] defined as a disease that affects fewer than 200,000 persons at a given time.[19] Furthermore, elderly HL is a disease for which (1) there is no agreed upon standard treatment approach; (2) it is difficult to investigate in classical trial format (due to the rarity of the disease, the advanced age of patients, and their underrepresentation in clinical trials); (3) there are large numbers of subjects who are frail or have excessive comorbidities; and (4) the approach to curative treatment is absent or inconsistent. Clinical data regarding elderly HL are derived mainly from registries and retrospective series, which have included heterogeneous patient populations. In addition, several sources of evidence suggest a different biology in patients with elderly HL.[1,15-17] An improved understanding of the epidemiology, biology, outcomes, and treatment options for elderly HL is needed.
Epidemiology
Descriptive Epidemiology
Within population-based studies, the proportion of HL patients aged 60 years or more has ranged from 15% to 30%.[1,5,13,20-22] However, the proportion of patients ≥ 60 years in clinical trials has been considerably lower, typically constituting < 5% to 10% of participants.[4,5,7]
Among two Swedish population reports from 1979 to 1988[22] and 1973 to 1994,[20] 31% and 26% of all HL patients, respectively, were ≥ 60 years. The British National Lymphoma Investigation (BNLI) compared the number of patients aged ≥ 65 years enrolled in clinical trials with the total number of older patients in their population-based cancer registry (1970–1987).[5] Approximately 15% of HL patients in the population were ≥ 65 years, whereas < 5% of patients in the same age group were entered onto BNLI trials. Investigators from the United Kingdom prospectively studied the incidence and outcomes of HL patients diagnosed between 1991 and 1998.[1,21] They reported that 20% of newly diagnosed HL patients were ≥ 60 years old. Moreover, the median overall survival of elderly HL patients was significantly inferior compared with a “normal” age- and sex-matched population (26 vs 150 months, respectively; P < .0001).
FIGURE 1
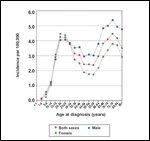
Incidence of Hodgkin Lymphoma in the United States, 2000-2005, by Age
Among recent data from the US National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) program, evidence of an age-related bimodal incidence pattern in HL persists (Figure 1). The increased incidence beyond age 65 is more pronounced for men vs women. Furthermore, in the 2000–2005 SEER-17 database, the incidence rates for elderly HL according to race are highest among Hispanics (6.5/100,000), followed by whites (4.5/100,000) and blacks (3.4/100,000). In addition, in part due to the inferior outcomes for older HL patients, the US prevalence among patients aged > 60 years is 15,400 compared with 140,700 for age < 30 years.[23]
Biologic Epidemiology
Epstein-Barr virus (EBV) is associated with a variety of hematopoietic malignancies including HL. Approximately 30% to 50% of all HL cases are EBV-positive, as identified by latent membrane protein (LMP)-1 or EBV-encoded RNA (EBER) immunostaining of the malignant cells.[24,25] The highest percentages of EBV-positive cases are seen in HL patients aged < 10 years or > 55 years.[15,24,25] Two population-based studies showed that the survival of older patients with EBV-positive tumors was significantly inferior compared with EBV-negative tumors.[1,15] Among 922 classical HL patients, Keegan et al showed that the presence of EBV independently predicted inferior survival for older adults (age 45–96 years), with significantly increased HL-specific mortality (hazard ratio [HR] for death = 2.5).[17]
In a prospective population-based elderly HL study, Stark et al reported that 34% of cases were EBV-positive and that EBV status correlated with stage at presentation (EBV-positive: 9% early stage vs 50% advanced stage, P = .0006).[1] Moreover, EBV-positive HL was associated with an inferior overall survival (median overall survival = 20 months vs not reached, respectively; P = .007). Recent reports have confirmed the inferior survival for older patients with EBV-positive HL vs EBV-negative disease.[26,27] Although the basis for this prognostic association is unknown, reduced EBV-specific cellular immunity of older patients has been proposed. The weaker immunocompetence in older patients may allow increased proliferation of an EBV-related tumor, and/or EBV antigens might induce a less robust immune response.[16,28]
Other pathologic and genetic features have emerged as potentially important prognostic factors in HL. Kelley and colleagues showed that HL patients with more intratumor T-cell regulatory cells (Tregs) and fewer activated cytotoxic T/NK lymphocytes had superior survival.[29] Interestingly, older age (> 45 years) in that analysis was associated with decreased forkhead box P3 (FOXP3) Tregs and increased granzyme-B–positive cells compared with younger patients. Diepstra et al reported that the lack of HLA class II cell-surface expression on HRS cells was associated with inferior failure-free and overall survival.[30] The only other factor in that study associated with increased risk of death was older age (> 65: relative risk of death = 6.47).
Prognosis andClinical Presentation
Prognosis: Age and IPS
Older age has been a consistent adverse prognostic factor for HL survival in population studies and clinical trial reports. The outcome for patients on the randomized Cancer and Leukemia Group B (CALGB) 8251 study (MOPP [mechlorethamine (Mustargen), vincristine, procarbazine, prednisone] vs ABVD vs alternating MOPP/ABVD) was dependent on age.[4] The 5-year overall survival was 31% for patients at least 60 years old vs 63% for patients aged 40 to 59 years, and 79% for age < 40 years (P < .0001). The median disease-free survival rates were 8.9 years for ages 16 to 45 years, 3.5 years for 46 to 55 years, 1.5 years for 56 to 65 years, and 0.7 years for > 65 years (P < .0001).
FIGURE 2

Survival Rate of Hodgkin Lymphoma by Age/Decade at Diagnosis in the United States, 1988-2004
In a recent analysis of US SEER data (1979–2004), Brenner et al reported increasing survival associated with HL, including elderly patients.[31] The 5-year survival rate increased 24% from 1980–1984 to 2000–2004 for HL patients over 60 in this analysis (35% to 59%, respectively). However, the 2000–2004 survival rates for older HL patients were still markedly inferior (> 30% lower) compared with younger populations. Current US SEER data show continued age-disparate outcomes in HL, as illustrated in Figure 2.
The BNLI compared survival of patients participating in randomized clinical trials from 1970 to 1987 with population-based data.[5] Age was the strongest risk factor for survival. Of note, both 5- and 10-year overall survival among BNLI trial participants aged 65 to 74 years were higher than for population-based patients. Among older patients entered on German Hodgkin Study Group (GHSG) protocols, patients ≥ 60 years old also had significantly worse freedom from treatment failure than younger patients (60% vs 80%, P < .001) and inferior overall survival (65% vs 90%) at 5 years.[7] This difference remained significant with the exclusion of events unrelated to HL.
One of the most commonly used prognostic tools in advanced-stage HL is the International Prognostic Score (IPS), which identified seven adverse prognostic factors, including age > 45 years.[32] Of note, only 9% of patients in the study that established the IPS were over 55, and no patients over 65 were included. Enblad et al analyzed registry data according to IPS from 1985 through 1992, consisting of 139 HL patients aged 60 and older.[33] When analyzing patients who were treated with curative intent, 29% had an IPS ≥ 4. These patients had a borderline worse prognosis compared to those with an IPS of 1 to 3.
Clinical Characteristics
TABLE 1

Clinical Characteristics of Elderly Hodgkin Lymphoma
Clinical characteristics of elderly HL patients are available through registry databases and some prospective clinical trials. Mir et al reported the clinical characteristics of HL patients at least 60 years old who were entered onto four consecutive CALGB randomized trials from 1969 to 1988 (Table 1).[4] In the most recent trial (CALGB 8251), 8% of patients were at least 60 years old. Mixed cellularity histology was more frequent in older patients, whereas mediastinal disease was less common. Levis et al compared a registry cohort of HL patients < 65 years old to patients ≥ 65.[13] These investigators also found frequent mixed cellularity among older patients, while younger patients more commonly presented with bulky mediastinal disease (22% vs 2%, respectively; P < .01).
Engert et al compared the characteristics and outcomes of all HL patients enrolled in GHSG clinical trials by age (> 60 years vs younger).[7] In that series, B symptoms, mixed cellularity, and poorer performance status were more common in older patients. According to IPS, older patients had more unfavorable risk factors vs younger patients, although when age was removed from the IPS calculation, that difference was no longer significant (age-adapted IPS 4–6: 13% vs 11%, respectively). Kim et al reported characteristics of 52 elderly patients treated over a 26-year period, finding that nodular sclerosis histology predominated in early-stage disease, whereas mixed cellularity was more common in advanced disease.[34]
Comorbidity
The presence of comorbidity as an independent prognostic factor is particularly relevant for older patients. Levis et al reported results of a trial including 105 elderly HL patients in which all patients received a lower-intensity regimen, VEPEMB (vinblastine, cyclophosphamide, procarbazine, etoposide, mitoxantrone, bleomycin).[35] Approximately 37% of patients had a comorbidity, defined as the presence of a concomitant disease requiring specific treatment. On multivariate analysis, in addition to stage and presence of B symptoms, presence of comorbidity was independently associated with inferior survival. Of note, the effect on disease-specific survival was as significant as the impact on overall survival, which suggests ineffective treatment and/or biology related to comorbidity rather than death from other causes.
In a population-based study, van Spronsen et al reported on 194 HL patients diagnosed between 1993 and 1996.[9] Among patients < 60 years old, 13% had a serious comorbid condition compared to 56% for older patients (P < .0001). The prevalence of comorbidity among HL patients was similar among early vs advanced stage. The most common comorbid conditions were cardiovascular disease (18%), hypertension (13%), chronic obstructive pulmonary disease (13%), and diabetes (10%). The proportion of elderly patients who received chemotherapy was 50% lower among those with a comorbidity vs no comorbidity (P = .01). Furthermore, elderly patients with early-stage HL and a comorbid condition received chemotherapy much less often (90% vs 33%, P = .05).
Guinee et al compared the outcomes for HL patients aged 60 to 79 years with those for patients aged 40 to 59 years from 1977 to 1983. The older group experienced twice the risk of dying from HL and four times the risk of dying from other causes compared with the younger group. Of note, older patients responded to therapy with similar complete response rates in their analysis (84% vs 88% in the younger group).[12] As proposed by Levis et al[35] and Proctor et al,[18] documentation of comorbid conditions and objective assessment of functional status such as the Comprehensive Geriatric Assessment[9] should be included in prospective studies. It may be possible to modify regimens and/or dosing based on objective criteria that predict for prohibitive morbidity and mortality.
Therapy and Clinical Outcomes
ABVD- and MOPP-Based Therapy
TABLE 2

Chemotherapy Series in Elderly Hodgkin Lymphoma
Few prospective or randomized HL trials have specifically studied older patients (age ≥ 60–65 years). The majority of treatment outcome data are derived from registry data and retrospective reports (Table 2). Internationally, the standard chemotherapeutic regimen for most HL patients is ABVD. Furthermore, three recent retrospective analyses have reported that ABVD may be safely administered at very high-dose intensity, although few patients were over age 60 in these series.[36-38] When ABVD is given with curative intent to patients over age 65 years, chemotherapy-related toxicities are often prohibitive (especially bleomycin-related toxicity).[4,7,13,14]
The report by Levis et al analyzed outcomes in patients ≥ 65 years who had received a registry-recommended protocol of ABVD, MOPP, or ABVD/MOPP therapy.[13] As noted, the 8-year event-free and overall survival rates were 41% and 46%, respectively-both significantly worse than the outcomes seen in patients < 65 years. One critical factor associated with the inferior outcomes among older patients was the 23% acute treatment-related death rate associated with ABVD-based therapy.
Age and Chemotherapy Dose Intensity
The impact of dose intensity on HL-related survival has been poorly studied, although a few studies have found that reduced drug intensity was associated with higher relapse and inferior survival.[20,39] One study found that patients aged > 50 were much more likely to receive suboptimal drug dosing.[39] Through registry data, Levis et al showed that the mean relative dose intensity (RDI) of ABVD-based therapy was significantly influenced by age.[13] Patients ≥ 65 years had 65% RDI through three cycles of chemotherapy and only 47% RDI through six cycles. This compared with 86% and 75%, respectively, for patients < 65 years.
For the GHSG, Engert et al studied chemotherapy administration differences based on age.[7] Patients ≥ 60 years old were more prone to dose reductions and had more frequent dose reductions (25% vs 11% for patients < 60 years old). They also showed that 75% of older patients received ≥ 85% of the intended chemotherapy compared with 91% for younger patients (P < .001).
Landgren et al reported outcomes based on RDI among 59 patients who received ABVD-based and MOPP-based therapy.[20] RDI > 65% was associated with improved cancer-specific survival (P = .024) and overall survival (P = .029) compared with RDI ≤ 65%. Moreover, patients who received ABVD-based chemotherapy with an RDI > 65% had significantly improved overall survival (P = .0011) compared with RDI ≤ 65% of ABVD- and MOPP-based chemotherapy, the latter irrespective of RDI.[20]
Unfortunately, as discussed before, it is often difficult to maintain a high/adequate ABVD RDI for elderly patients. It should also be recognized that the majority of these study comparisons are retrospective. The data need to be interpreted carefully-in part, since the explanations for dose reduction were often not available, and patient selection is likely a contributing factor.
Individualized Dosing/Decreased Intensity
Efforts to improve outcomes in elderly HL have included decreased intensity of chemotherapy and use of regimens with individualized dosing in order to minimize toxicity. Levis et al used CVP/CEB (chlorambucil, vinblastine, procarbazine, prednisone, cyclophosphamide, etoposide, bleomycin), a regimen with a relatively lower RDI, for HL patients aged > 65 years (Table 2).[2] CVP/CEB resulted in a 73% complete response rate, although the relapse-free survival rate was high compared with more aggressive regimens.
Levis et al also reported a prospective trial using the lower-intensity regimen VEPEMB in 105 patients aged > 65 years.[35] Patients with early-stage disease received three VEPEMB cycles followed by involved-field radiation therapy (IFRT), whereas patients with advanced-stage disease received six cycles. For advanced-stage patients, the complete response rate was 58% with a 5-year relapse-free survival of 66% and overall survival of 32%. On multivariate analysis, early stage, absence of B symptoms, and absence of comorbidity were all associated with improved survival.
Enblad et al compared outcomes in patients from 1989 to 1992 using the LVPP/OEPA regimen (chlorambucil, vinblastine, procarbazine, vincristine, etoposide, prednisone, doxorubicin), incorporating individualized dosing based on performance status and comorbidities.[33] Outcomes were compared to the prior time period (1985–1988), when patients received MOPP/ABVD or MOPP. Overall, survival rates were similar between the two time periods. Infection rates were similar in the two cohorts (31%–42%), and most infections were opportunistic (eg, pneumocystis, fungal, herpetic).
Other lower-intensity nonanthracycline regimens include ChlVPP (chlorambucil, vinblastine, procarbazine, prednisone)[40] and BCVPP (carmustine [BiCNU], cyclophosphamide, vinblastine, procarbazine, prednisone),[41] but the BCVPP regimen has never been studied exclusively in an elderly HL patient population.
Other Chemotherapy Regimens
TABLE 3

Outcomes for Early-Stage Elderly Hodgkin Lymphoma
Macpherson et al studied higher-dose regimens by increasing the number of non–cross-resistant drugs and attempting to deliver therapy without treatment delays.[42] Prior to 1986, older patients were treated with MOPP/ABV-based therapy, while after 1986, patients received the regimen ODBEP (vincristine, doxorubicin, bleomycin, etoposide, prednisolone). Outcomes for ODBEP therapy did not differ compared with MOPP/ABV treatment (Table 3).
An intensive therapeutic regimen such as BEACOPP is too toxic for HL patients aged > 60 years. The GHSG reported outcomes for 75 patients aged 66 to 75 years with advanced-stage HL in the randomized study HD9elderly, comparing a baseline BEACOPP regimen with COPP (cyclophosphamide, vincristine, procarbazine, prednisolone)-ABVD.[10] The investigators observed no remission or survival differences between the regimens with pooled 5-year freedom from treatment failure and overall survival rates of 46% and 50%, respectively. Of note, the GHSG currently only enrolls patients < 60 years of age for all BEACOPP trials (personal communication, V. Diehl).
Role of Anthracycline
The inclusion of anthracycline therapy is likely an important factor in terms of attaining a durable disease-free survival for HL.[3,43,44] The Nebraska group reported results among 262 newly diagnosed HL patients, of which 21% were aged ≥ 60 years, treated with either ChlVPP or ChlVPP plus ABV hybrid, a modified anthracycline-based regimen (Table 2).[3] Among patients ≥ 60 years, the only factor associated with improved outcome on multivariate analysis was treatment with ChlVPP/ABV hybrid (n = 25) vs ChlVPP therapy (n = 31).
Early-Stage Disease
Few reports are available that have analyzed early-stage elderly HL patients. Kim et al reported the outcomes of 52 early-stage patients over a 26-year period (Table 3).[34] Patients received radiation alone (n = 37), chemotherapy alone (n = 9), or combined chemotherapy/radiation (n = 6). The chemotherapy regimens used were heterogeneous with a median of six cycles delivered. The crude relapse rates were 20% for combined-modality therapy, 33% for chemotherapy alone, and 46% for radiation alone, but these differences did not achieve statistical significance as the sample sizes were small. The 5- and 10-year overall survival rates for early-stage patients were 55% and 31%, respectively.
The prospective phase II study by Levis et al using VEPEMB included 48 patients with stage IA–IIA disease.[35] Therapy was well tolerated, with a 5-year disease-specific survival of 97%, failure-free survival of 79%, and overall survival of 94% (Table 3).
Klimm et al reported results among HL patients ≥ 60 years old who enrolled onto the GHSG HD8 phase III trial (89/1,064).[45] HD8 was an early-stage, unfavorable (intermediate) HL trial, in which after two cycles each of ABVD and COPP, patients were randomized to 40 Gy of extended-field RT (EFRT) or 40 Gy of IFRT. At a 60-month median follow-up, outcomes were superior for younger patients (age < 60 vs ≥ 60 years) with 5-year freedom-from-treatment-failure rates of 87% vs 64%, respectively (P < .001), and 5-year overall survival rates of 94% vs 70%, respectively (P < .001). Grade 3/4 toxicity was more common among elderly patients who received EFRT vs IFRT, including leukopenia, anemia, and nausea.
Landgren et al compared results among HL patients aged ≥ 60 years with those aged < 60 years, all of whom received RT alone for early-stage disease.[46] The complete response rate was lower for patients aged ≥ 60 years, while the relapse rate was similar at 42%, at a median of 21 months (range = 3–165 months). In terms of relapse, age ≥ 60 years was an adverse prognostic factor for overall survival (HR = 9.59, P < .0001).
Chemotherapy-Related Toxicity
Treatment-related toxicity is a significant concern for elderly HL patients undergoing chemotherapy-in particular, myelosuppression, pulmonary toxicity, and cardiac toxicity. The GHSG showed that severe toxicity (ie, World Health Organization grade 4) was more common in older patients vs younger patients (42% vs 27%; P < .001).[7] The most common toxicity in older patients was hematologic. In addition, grade 3/4 infections were more common in older vs younger patients, as was fatal treatment-related toxicity (6% vs 0.6%, P < .001).
The incidence of bleomycin lung toxicity in the literature is variable, but has been reported as high as 46%.[47,48] Older age has been a consistent risk factor associated with bleomycin lung toxicity in addition to cumulative bleomycin dose, renal insufficiency, pulmonary radiation, underlying lung disease, and tobacco history.[47-49] Initial phase I trials of bleomycin suggested an increased risk of bleomycin lung toxicity among elderly patients.[50] More recently, the Mayo Clinic reported a 33% incidence rate of bleomycin lung toxicity for patients > 40 years old compared with 11% for younger patients.[14] The CALGB also reported a higher rate of pulmonary toxicity in patients > 40 years vs younger patients (38% vs 22%, respectively).[51]
In addition, preclinical data[52,53] and case series[14,54,55] have suggested that granulocyte colony-stimulating factor (G-CSF, Neupogen) may increase the incidence of bleomycin-induced lung damage, related in part to extensive neutrophil recruitment following G-CSF administration, with associated free radical–induced pulmonary damage. Of note, the retrospective report from the Mayo Clinic showed a significant increase in lung toxicity when G-CSF was used during bleomycin-containing chemotherapy (26% vs 9% without G-CSF, P = .014).[14] Moreover, all patients who died of bleomycin lung toxicity were > 40 years, yielding an associated death rate of 40%.
Future Directions
FDG-PET
18F-fluorodeoxyglucose (FDG)–positron emission tomography (PET) has become a standard imaging modality for the evaluation of HL.[56-59] Gallamini and colleagues reported on the prognostic importance of “early PET” following two of six planned cycles (PET-2) of ABVD for 190 patients with advanced-stage HL.[60] It is not clear if the prognostic results of early PET can be applied to older HL patients and/or when using less-intensive regimens. Among the Gallamini and Hutchings PET-2 series, 20 of 260 patients (7.7%) were aged ≥ 60 years; 15 of 15 PET-2–negative older patients are in continued remission at a median follow-up of 3 years, while 4 of 5 PET-2–positive patients relapsed within 1 year following completion of therapy (personal communication, M. Hutchings). Further evaluation of the prognostic value of early PET in elderly HL is warranted.
Rituximab
The majority of experience using rituximab in HL is with nodular lymphocyte-predominant HL (NLPHL). Rituximab as a single-agent in untreated and relapsed CD20-positive NLPHL is associated with objective response rates of 86% to 100%.[61-63] With extended follow-up in the German series (median 63 months), the median time to disease progression was 33 months, and the median overall survival was not reached (> 90% alive).[63]
Fanale and colleagues reported on the outcomes of NLPHL patients treated with various treatment regimens over a 10-year period.[64] Patients who received R-CHOP (rituximab [Rituxan], cyclophosphamide, doxorubicin, vincristine, prednisone) had a reported complete response rate of 94% and event-free and overall survival rates of nearly 100%. Outcomes of R-CHOP–treated NLPHL patients was superior vs all other treatment regimens.
For classical HL, most Hodgkin/Reed-Sternberg (H-RS) cells do not express CD20 and, even when expressed, there is marked variability within a single tissue sample. However, Ambinder et al recently documented in HL cell lines and patient samples that a subpopulation of stem cells related to H-RS cells expressed CD20.[65] In addition, after isolation of H-RS tumor cells, immunoglobulin gene rearrangements were found to be clonal and express CD20.
Rituximab may play a role in classical HL by targeting the surrounding nonmalignant B cells that support H-RS cells. Younes et al treated 22 patients (median age = 35 years, range = 17–66) with recurrent classical HL with six weekly doses of rituximab.[66] The objective response rate was 22%, with a median response duration of 7.8 months. Responses were independent of CD20 status and were limited to patients without extranodal involvement. The same group also combined rituximab with ABVD for untreated disease[67] and with gemcitabine (Gemzar) for relapsed HL.[68]
CHOP
Kolstad and colleagues recently reported encouraging results using CHOP (cyclophosphamide, doxorubicin, vincristine, prednisone) for elderly HL.[69] They studied 29 older patients who were treated with CHOP every 21 days (early-stage: 2–4 cycles and IFRT; advanced-stage: 6–8 cycles with or without IFRT). At the completion of CHOP with or without radiation for all patients, the complete response rate was 93%. With 41-month median follow-up, the 3-year progression-free and overall survival rates were 76% and 79%, respectively (Table 2). Two patients had grade 3 cardiac toxicity (both had prior cardiac conditions), and two treatment-related deaths were seen (one myocardial infarction and another due to pneumonia).
Novel Therapeutics
Autologous stem cell transplantation for relapsed/refractory HL may be considered for selected older patients with chemotherapy-sensitive disease and good functional status. A multitude of new targeted treatments are being developed and investigated in relapsed/refractory HL. These novel agents include receptor-specific antibodies (eg, CD30, CD40), radiolabeled antibodies (eg, anti-CD25, anti-CD30), antiapoptotic agents including inhibitors of I-kappaB kinase and nuclear factor–kappaB cascade as well as X-linked inhibitors of apoptosis proteins (eg, antisense oligonucleotides), transcription pathway modulators such as histone deacetylase (HDAC) and mammalian target of rapamycin (mTOR) inhibitors, as well as EBV-directed therapy (eg, EBV-cytotoxic T-cells, LMP2A-based).
SHIELD Program
The Study for Hodgkin’s In the Elderly Lymphoma Database (SHIELD), initiated by Proctor and colleagues from the United Kingdom, is an important ongoing international effort to provide prospective data collection and clinical study of elderly HL.[18] Through an interactive Web-based program (www.shieldstudy.co.uk), individual physicians are able to register and treat elderly HL patients through the assigned SHIELD phase II clinical trial (using VEPEMB) or with an alternative regimen. The program includes assessment and documentation of comorbidity and functional scales of daily living.[9] As of October 2008, 187 patients have been recruited including 103 registration patients and 84 patients enrolled onto the phase II clinical trial.
Conclusions
Elderly HL remains a disease for which no standard treatment recommendations exist. Moreover, elderly patients are underrepresented in HL prospective clinical studies, and survival rates in this population are disproportionately inferior to those of younger patients. Elderly HL patients commonly present with mixed-cellularity histology, EBV-positive disease, poor performance status, presence of B symptoms, absence of bulk, and advanced stage. Examination of the biologic, molecular, and genetic factors in elderly HL should continue.
Generally, treatment of elderly HL patients for all disease stages should be given with curative intent, but more effective, tolerable therapeutic regimens are needed. Bleomycin-containing regimens including ABVD are associated with pulmonary toxicity, and intensive therapy such as BEACOPP is not tolerated; whereas less intensive regimens such as CVP/CEB and ChlVPP are ineffective. Inclusion of anthracycline therapy appears to improve outcomes, and limited data with CHOP look promising. In addition, further evaluation of the prognostic value of early PET in elderly HL is warranted. Finally, continued multicenter collaborations with prospective clinical trials including formal assessment of comorbidity and functional status will be critical to the successful study and treatment of elderly HL.
References:
References
1. Stark GL, Wood KM, Jack F, et al: Hodgkin’s disease in the elderly: A population-based study. Br J Haematol 119:432-440, 2002.
2. Levis A, Depaoli L, Bertini M, et al: Results of a low aggressivity chemotherapy regimen (CVP/CEB) in elderly Hodgkin’s disease patients. Haematologica 81:450-456, 1996.
3. Weekes CD, Vose JM, Lynch JC, et al: Hodgkin’s disease in the elderly: Improved treatment outcome with a doxorubicin-containing regimen. J Clin Oncol 20:1087-1093, 2002.
4. Mir R, Anderson J, Strauchen J, et al: Hodgkin disease in patients 60 years of age or older. Histologic and clinical features of advanced-stage disease. The Cancer and Leukemia Group B. Cancer 71:1857-1866, 1993.
5. Roy P, Vaughan Hudson G, Vaughan Hudson B, et al: Long-term survival in Hodgkin’s disease patients. A comparison of relative survival in patients in trials and those recorded in population-based cancer registries. Eur J Cancer 36:384-389, 2000.
6. Erdkamp FL, Breed WP, Bosch LJ, et al: Hodgkin disease in the elderly. A registry-based analysis. Cancer 70:830-834, 1992.
7. Engert A, Ballova V, Haverkamp H, et al: Hodgkin’s lymphoma in elderly patients: A comprehensive retrospective analysis from the German Hodgkin’s Study Group. J Clin Oncol 23:5052-5060, 2005.
8. Janssen-Heijnen ML, van Spronsen DJ, Lemmens VE, et al: A population-based study of severity of comorbidity among patients with non-Hodgkin’s lymphoma: Prognostic impact independent of International Prognostic Index. Br J Haematol 129:597-606, 2005.
9. van Spronsen DJ, Janssen-Heijnen ML, Lemmens VE, et al: Independent prognostic effect of co-morbidity in lymphoma patients: Results of the population-based Eindhoven Cancer Registry. Eur J Cancer 41:1051-1057, 2005.
10. Ballova V, Ruffer JU, Haverkamp H, et al: A prospectively randomized trial carried out by the German Hodgkin Study Group (GHSG) for elderly patients with advanced Hodgkin’s disease comparing BEACOPP baseline and COPP-ABVD (study HD9elderly). Ann Oncol 16:124-131, 2005.
11. Diaz-Pavon JR, Cabanillas F, Majlis A, et al: Outcome of Hodgkin’s disease in elderly patients. Hematol Oncol 13:19-27, 1995.
12. Guinee VF, Giacco GG, Durand M, et al: The prognosis of Hodgkin’s disease in older adults. J Clin Oncol 9:947-953, 1991.
13. Levis A, Depaoli L, Urgesi A, et al: Probability of cure in elderly Hodgkin’s disease patients. Haematologica 79:46-54, 1994.
14. Martin WG, Ristow KM, Habermann TM, et al: Bleomycin pulmonary toxicity has a negative impact on the outcome of patients with Hodgkin’s lymphoma. J Clin Oncol 23:7614-7620, 2005.
15. Enblad G, Sandvej K, Sundstrom C, et al: Epstein-Barr virus distribution in Hodgkin’s disease in an unselected Swedish population. Acta Oncol 38:425-429, 1999.
16. Gandhi MK, Tellam JT, Khanna R: Epstein-Barr virus-associated Hodgkin’s lymphoma. Br J Haematol 125:267-281, 2004.
17. Keegan TH, Glaser SL, Clarke CA, et al: Epstein-Barr virus as a marker of survival after Hodgkin’s lymphoma: A population-based study. J Clin Oncol 23:7604-7613, 2005.
18. Proctor SJ, White J, Jones GL: An international approach to the treatment of Hodgkin’s disease in the elderly: Launch of the SHIELD study programme. Eur J Haematol Suppl 75(s66):63-67, 2005.
19. US Food and Drug Administration: The orphan drug act. Available at
http://www.fda.gov/orphan/oda.htm
. Accessed September 17, 2008.
20. Landgren O, Algernon C, Axdorph U, et al: Hodgkin’s lymphoma in the elderly with special reference to type and intensity of chemotherapy in relation to prognosis. Haematologica 88:438-444, 2003.
21. Proctor SJ, Rueffer JU, Angus B, et al: Hodgkin’s disease in the elderly: Current status and future directions. Ann Oncol 13(suppl 1):133-137, 2002.
22. Enblad G, Glimelius B, Sundstrom C: Treatment outcome in Hodgkin’s disease in patients above the age of 60: A population-based study. Ann Oncol 2:297-302, 1991.
23. Surveillance Epidemiology and End Results: SEER stat fact sheets. Available at
http://www.seer.cancer.gov/statfacts/html/hodg.html
. Accessed September 17, 2008.
24. Armstrong AA, Alexander FE, Cartwright R, et al: Epstein-Barr virus and Hodgkin’s disease: Further evidence for the three disease hypothesis. Leukemia 12:1272-1276, 1998.
25. Glaser SL, Lin RJ, Stewart SL, et al: Epstein-Barr virus-associated Hodgkin’s disease: Epidemiologic characteristics in international data. Int J Cancer 70:375-382, 1997.
26. Diepstra A, van Imhoff GW, Karim-Kos H, et al: Latent EBV infection of Hodgkin Reed-Sternberg cells predicts adverse outcome in older adult classical Hodgkin lymphoma patients. 7th International Symposium on Hodgkin Lymphoma (abstract C016). Haematologica 92(s5):29, 2007.
27. Asano N, Tamaru JI, Kinoshita TO, et al: Age-related EBV-associcated B-cell lymphoproliferative disorders: Comparison with EBV-positive classical Hodgkin lymphoma in elderly patients. 7th International Symposium on Hodgkin Lymphoma (abstract P039). Haematologica 92(s5):44, 2007.
28. Frisan T, Sjoberg J, Dolcetti R, et al: Local suppression of Epstein-Barr virus (EBV)-specific cytotoxicity in biopsies of EBV-positive Hodgkin’s disease. Blood 86:1493-1501, 1995.
29. Kelley TW, Pohlman B, Elson P, et al: The ratio of FOXP3+ regulatory T cells to granzyme B+ cytotoxic T/NK cells predicts prognosis in classical Hodgkin lymphoma and is independent of bcl-2 and MAL expression. Am J Clin Pathol 128:958-965, 2007.
30. Diepstra A, van Imhoff GW, Karim-Kos HE, et al: HLA class II expression by Hodgkin Reed-Sternberg cells is an independent prognostic factor in classical Hodgkin’s lymphoma. J Clin Oncol 25:3101-3108, 2007.
31. Brenner H, Gondos A, Pulte D: Ongoing improvement in long-term survival of patients with Hodgkin disease at all ages and recent catch-up of older patients. Blood 111:2977-2983, 2008.
32. Hasenclever D, Diehl V: A prognostic score for advanced Hodgkin’s disease. International Prognostic Factors Project on Advanced Hodgkin’s Disease. N Engl J Med 339:1506-1514, 1998.
33. Enblad G, Gustavsson A, Sundstrom C, et al: Patients above sixty years of age with Hodgkin’s lymphoma treated with a new strategy. Acta Oncol 41:659-667, 2002.
34. Kim HK, Silver B, Li S, et al: Hodgkin’s disease in elderly patients (> or =60): Clinical outcome and treatment strategies. Int J Radiat Oncol Biol Phys 56:556-560, 2003.
35. Levis A, Anselmo AP, Ambrosetti A, et al: VEPEMB in elderly Hodgkin’s lymphoma patients. Results from an Intergruppo Italiano Linfomi (IIL) study. Ann Oncol 15:123-128, 2004.
36. Chand VK, Link BK, Ritchie JM, et al: Neutropenia and febrile neutropenia in patients with Hodgkin’s lymphoma treated with doxorubicin (Adriamycin), bleomycin, vinblastine and dacarbazine (ABVD) chemotherapy. Leuk Lymphoma 47:657-663, 2006.
37. Boleti E, Mead GM: ABVD for Hodgkin’s lymphoma: Full-dose chemotherapy without dose reductions or growth factors. Ann Oncol 18:376-380, 2006.
38. Evens AM Cilley J, Ortiz T, et al: G-CSF is not necessary to maintain over 99% dose-intensity with ABVD in the treatment of Hodgkin lymphoma: Low toxicity and excellent outcomes in a 10-year analysis. Br J Haematol 137:545-552, 2007.
39. Yarnold JR, Jelliffe AM, Hudson GV: Factors affecting relapse following chemotherapy for Hodgkin’s disease. Clin Radiol 33:627-629, 1982.
40. McElwain TJ, Toy J, Smith E, et al: A combination of chlorambucil, vinblastine, procarbazine and prednisolone for treatment of Hodgkin’s disease. Br J Cancer 36:276-280, 1977.
41. Bakemeier RF, Anderson JR, Costello W, et al: BCVPP chemotherapy for advanced Hodgkin’s disease: Evidence for greater duration of complete remission, greater survival, and less toxicity than with a MOPP regimen. Results of the Eastern Cooperative Oncology Group study. Ann Intern Med 101:447-456, 1984.
42. Macpherson N, Klasa RJ, Gascoyne R, et al: Treatment of elderly Hodgkin’s lymphoma patients with a novel 5-drug regimen (ODBEP): A phase II study. Leuk Lymphoma 43:1395-1402, 2002.
43. Canellos GP, Anderson JR, Propert KJ, et al: Chemotherapy of advanced Hodgkin’s disease with MOPP, ABVD, or MOPP alternating with ABVD. NÂ Engl J Med 327:1478-1484, 1992.
44. Radford JA, Crowther D, Rohatiner AZ, et al: Results of a randomized trial comparing MVPP chemotherapy with a hybrid regimen, ChlVPP/EVA, in the initial treatment of Hodgkin’s disease. J Clin Oncol 13:2379-2385, 1995.
45. Klimm B, Eich HT, Haverkamp H, et al: Poorer outcome of elderly patients treated with extended-field radiotherapy compared with involved-field radiotherapy after chemotherapy for Hodgkin’s lymphoma: An analysis from the German Hodgkin Study Group. Ann Oncol 18:357-363, 2007.
46. Landgren O, Axdorph U, Fears TR, et al: A population-based cohort study on early-stage Hodgkin lymphoma treated with radiotherapy alone: With special reference to older patients. Ann Oncol 17:1290-1295, 2006.
47. Coiffier B, Lepage E, Briere J, et al: CHOP chemotherapy plus rituximab compared with CHOP alone in elderly patients with diffuse large-B-cell lymphoma. N Engl J Med 346:235-242, 2002.
48. Sleijfer S: Bleomycin-induced pneumonitis. Chest 120:617-624, 2001.
49. Azambuja E, Fleck JF, Batista RG, et al: Bleomycin lung toxicity: Who are the patients with increased risk? Pulm Pharmacol Ther 18:363-366, 2005.
50. Blum RH, Carter SK, Agre K: A clinical review of bleomycin-a new antineoplastic agent. Cancer 31:903-914, 1973.
51. Duggan DB, Petroni GR, Johnson JL, et al: Randomized comparison of ABVD and MOPP/ABV hybrid for the treatment of advanced Hodgkin’s disease: Report of an intergroup trial. J Clin Oncol 21:607-614, 2003.
52. Adach K, Suzuki M, Sugimoto T, et al: Granulocyte colony-stimulating factor exacerbates the acute lung injury and pulmonary fibrosis induced by intratracheal administration of bleomycin in rats. Exp Toxicol Pathol 53:501-510, 2002.
53. Azoulay E, Herigault S, Levame M, et al: Effect of granulocyte colony-stimulating factor on bleomycin-induced acute lung injury and pulmonary fibrosis. Crit Care Med 31:1442-1448, 2003.
54. Matthews JH: Pulmonary toxicity of ABVD chemotherapy and G-CSF in Hodgkin’s disease: Possible synergy. Lancet 342:988, 1993.
55. Dirix LY, Schrijvers D, Druwe P, et al: Pulmonary toxicity and bleomycin. Lancet 344:56, 1994.
56. Friedberg JW, Fischman A, Neuberg D, et al: FDG-PET is superior to gallium scintigraphy in staging and more sensitive in the follow-up of patients with de novo Hodgkin lymphoma: A blinded comparison. Leuk Lymphoma 45:85-92, 2004.
57. Jerusalem G, Beguin Y, Fassotte MF, et al: Early detection of relapse by whole-body positron emission tomography in the follow-up of patients with Hodgkin’s disease. Ann Oncol 14:123-130, 2003.
58. Jerusalem G, Beguin Y, Fassotte MF, et al: Whole-body positron emission tomography using 18F-fluorodeoxyglucose compared to standard procedures for staging patients with Hodgkin’s disease. Haematologica 86:266-273, 2001.
59. Stumpe KD, Urbinelli M, Steinert HC, et al: Whole-body positron emission tomography using fluorodeoxyglucose for staging of lymphoma: Effectiveness and comparison with computed tomography. Eur J Nucl Med 25:721-728, 1998.
60. Gallamini A, Hutchings M, Rigacci L, et al: Early interim 2-[18F]fluoro-2-deoxy-D-glucose positron emission tomography is prognostically superior to international prognostic score in advanced-stage Hodgkin’s lymphoma: A report from a joint Italian-Danish study. J Clin Oncol 25:3746-3752, 2007.
61. Ekstrand BC, Lucas JB, Horwitz SM, et al: Rituximab in lymphocyte-predominant Hodgkin disease: Results of a phase 2 trial. Blood 101:4285-4289, 2003.
62. Rehwald U, Schulz H, Reiser M, et al: Treatment of relapsed CD20+ Hodgkin lymphoma with the monoclonal antibody rituximab is effective and well tolerated: Results of a phase 2 trial of the German Hodgkin Lymphoma Study Group. Blood 101:420-424, 2003.
63. Schulz H, Rehwald U, Morschhauser F, et al: Rituximab in relapsed lymphocyte-predominant Hodgkin lymphoma: Long-term results of a phase 2 trial by the German Hodgkin Lymphoma Study Group (GHSG). Blood 111:109-111, 2008.
64. Fanale MA, Fayed LE, Romaguera JE, et al: Experience with R-CHOP in patients with lymphocyte predominant Hodgkin lymphoma (LPHL). 7th International Symposium on Hodgkin Lymphoma (abstract P077). Haematologica 92(s5):57, 2007.
65. Ambinder RF, Jones RJ, Matsui W: Hodgkin’s lymphoma (HL): Evidence for a cancer stem cell and therapeutic implications. 7th International Symposium on Hodgkin Lymphoma (abstract I038). Haematologica 92(s5):12, 2007.
66. Younes A, Romaguera J, Hagemeister F, et al: A pilot study of rituximab in patients with recurrent, classic Hodgkin disease. Cancer 98:310-314, 2003.
67. Younes A, Fayad L, Goy A, et al: Phase II study of rituximab plus ABVD for the treatment of newly diagnosed patients with advanced stage classical Hodgkin lymphoma. 7th International Symposium on Hodgkin Lymphoma (abstract C024). Haematologica 92(s5):33, 2007.
68. Oki Y, Pro B, Fayad LE, et al: Phase 2 study of gemcitabine in combination with rituximab in patients with recurrent or refractory Hodgkin lymphoma. Cancer 112:831-836, 2008.
69. Kolstad A, Nome O, Delabie J, et al: Standard CHOP-21 as first line therapy for elderly patients with Hodgkin’s lymphoma. Leuk Lymphoma 48:570-576, 2007.
70. Feltl D, Vitek P, Zamecnik J: Hodgkin’s lymphoma in the elderly: The results of 10 years of follow-up. Leuk Lymphoma 47:1518-1522, 2006.