Immunoglobulin Light-Chain Amyloidosis: Growing Recognition, New Approaches to Therapy, Active Clinical Trials
When light-chain amyloidosis is diagnosed prior to the development of advanced cardiomyopathy, systemic therapy is capable of producing hematologic responses that will translate into organ responses and prolonged survival. Advances in the management of multiple myeloma are currently being translated into a variety of clinical trials designed to improve the quality of life and survival of patients with light-chain amyloidosis.
Immunoglobulin light-chain amyloidosis needs to be considered in any patient presenting with cardiomyopathy with preserved systolic function, heavy albuminuria, an unexplained sensorimotor peripheral neuropathy, hepatomegaly, or atypical MGUS (monoclonal gammopathy of undetermined significance) or myeloma. The prognosis of the disease is determined by the levels of cardiac biomarkers and the pretreatment levels of immunoglobulin free light chains. All patients with systemic light-chain amyloid require therapy. There is no presymptomatic phase that warrants observation. Stem-cell transplantation produces a high response rate but is a viable option in only 20% of patients. Corticosteroids, alkylating agents, immunomodulatory drugs, and proteasome inhibitors all have shown activity in this disorder, and combinations are currently being explored in clinical trials. Despite advances in the past decade, 30% of patients still die within a year of diagnosis, suggesting that failure to recognize this disorder prior to advanced organ dysfunction remains a major impediment to improving outcomes.
Introduction
Light-chain (AL) amyloidosis occurs when a clonal population of bone marrow plasma cells secretes an immunoglobulin light chain that undergoes misfolding.[1] The resulting insoluble light-chain or heavy-chain fragments deposit in tissues in a β-pleated sheet configuration and lead to organ dysfunction.[2] There is no diagnostic blood test or imaging study for AL amyloidosis. Recognition requires a high index of suspicion and a tissue biopsy that demonstrates green birefringence when a Congo red–stained specimen is viewed under polarized light.[3]
Patient 1
FIGURE 1
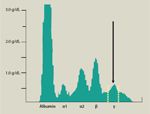
Serum Protein Electrophoretic Pattern of Patient 1
A 79-year-old male had symptomatic dyspnea on exertion and lower extremity edema for 1 year. The patient had CT imaging of the abdomen that showed small retroperitoneal nodes. This finding led to a laparoscopic biopsy. Sinus histiocytosis was found; no malignancy was present. He underwent echocardiography that showed concentric left ventricular hypertrophy. His ECG demonstrated an anterior infarction pattern. The ECG finding led to a cardiac catheterization that showed both a normal ejection fraction and normal coronary arteries. Following the catheterization, the patient was informed that his dyspnea did not have a cardiac cause, and he was referred to the Mayo Clinic Division of Thoracic Diseases for evaluation.
FIGURE 2
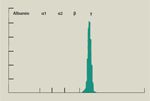
Urine Protein Electrophoretic Pattern of Patient 1
When the patient came to the Mayo Clinic, a serum protein electrophoresis was performed (Figure 1). The protein electrophoretic finding led to a 24-hour urine protein electrophoresis (Figure 2). The echocardiogram was repeated and was reinterpreted as showing thickening of the heart walls and valves consistent with an infiltrative cardiomyopathy with restrictive hemodynamics. A subcutaneous fat aspiration was performed, which demonstrated amyloid. The original retroperitoneal node biopsy was obtained from the local hospital. It was stained with Congo red and was positive.
Comments on Patient 1
This patient had an ECG that showed a pseudo-infarction pattern; considered in conjunction with his dyspnea, it was felt to represent silent ischemic heart disease. The presence of a pseudo-infarction pattern on ECG is a post-hoc diagnosis that requires knowledge of the correct process in order to be interpreted. The thickening of the ventricular walls was assumed to be hypertrophy rather than infiltration, presumably because hypertrophy secondary to hypertension is so much more common in the US population. The performance of cardiac catheterization without a right ventricular biopsy indicated a failure to recognize an important cause of heart failure with preserved systolic function. The key diagnostic test was the serum protein electrophoresis, which showed an extremely small (size, 0.5 g/dL) monoclonal protein migrating in the gamma fraction. The 24-hour urine protein measurement demonstrated only 220 mg for the 24-hour period, which is quantitatively insignificant; however, the electrophoresis demonstrated that all of the protein was monoclonal immunoglobulin light chain and not albumin. Most physicians assume that proteinuria equates to albuminuria, but this was not the case here. This patient had a 1-year delay in diagnosis, reducing the likelihood of chemotherapy being effective.
Light-chain amyloidosis should be considered in any patient who has symptoms consistent with cardiomyopathy. These may be as subtle as mild dyspnea on exertion or modest edema in the lower extremities. Exertional fatigue is a common presentation of cardiac amy-loidosis; to arrive at the correct diagnosis requires a careful physical examination that could reveal distention of the jugular veins. This finding reflects restriction to flow and high filling pressures on the right side of the heart. An assessment of cardiac biomarkers,[4] particularly brain natriuretic peptide (BNP) or N-terminal prohormone-BNP (NT-proBNP), and an echocardiogram with Doppler studies[5] that can recognize changes in diastolic flow patterns, will reveal infiltrative cardiomyopathy.
Patient 2
A 47-year-old male was found to have 9.7 grams of protein in a 24-hour urine collection. The patient received a trial of high-dose corticosteroids, which produced no reduction in urinary protein. Because of increasing edema and fatigue, an echocardiogram was performed; this showed a ventricular septal thickness of 18 mm. The cause of the thickening was not commented on. A renal biopsy was performed, and amyloid deposits were detected. Subsequent testing with serum and urine electrophoresis with immunofixation and serum immunoglobulin free light chains revealed monoclonal free λ light chains in the serum and urine (Bence-Jones proteinemia and proteinuria). The κ free light chain was 9.7 mg/L (normal, 3.3-19.4 mg/L), and the λ free light chain was 137 mg/L (normal, 5.7-26.3 mg/L), with a ratio of 0.07 (normal, 0.26-1.65), reflecting excess production of λ immunoglobulins.
Comments on Patient 2
All patients with heavy albuminuria that is not attributable to an obvious cause such as long-standing diabetes mellitus should be screened for amy-loidosis.[6] Frequently, these patients are assumed to have minimal-change glomerulonephropathy or membranoproliferative glomerulonephropathy and undergo an empiric trial of corticosteroids, which delays more effective interventions. Screening with the combination of a serum protein electrophoresis with immunofixation and a serum immunoglobulin free light chain has a sensitivity of 96% for detection of a monoclonal protein in patients with AL amyloidosis.[7] The addition of a urine immunofixation increases sensitivity to 98%. The detection of a monoclonal protein reduces the differential diagnosis to myeloma cast nephropathy, ? light chain deposition disease, cryoglobulin-emia, and light-chain amyloidosis. In this instance, the patient had an 8-month delay between the first recognition of proteinuria and the initiation of effective therapy. This patient underwent stem-cell transplantation and is alive with normal renal function at 180 months. His lowest recorded urinary protein post-transplant was 0.27 g/day.
TABLE 1
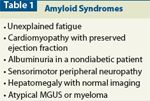
Recommended Diagnostic Testing for a Histologic Diagnosis of AmyloidosisTABLE 2

Recommended Diagnostic Testing for a Histologic Diagnosis of Amyloidosis
Light-chain amyloidosis, which is seen in 8 persons per million per year,[8] is a disease of small amounts of monoclonal protein. Although the majority of small monoclonal gammopathies are innocuous, they may be associated with a syndrome characterized by “dangerous small clones.”[9] Larger plasma cell clones are most often associated with multiple myeloma,[10] which is about five times as prevalent as light-chain amyloidosis.
Much has been written on the physical findings of tongue enlargement[11] and periorbital purpura.[12] These are found in no more than 15% of patients and are overlooked half of the time because the purpura may only be visible when the eyes are closed, and most of the tongue enlargement is at the base and is limited to dental indentations on the underside of the tongue. It would be wrong not to consider light-chain amyloidosis in a patient who has a completely normal physical examination. If the patient has any of the syndromes listed in Table 1, immunofixation and electrophoresis of the serum and urine, and free light chain analysis should be done.[13] If the results of any of these studies are positive, biopsies of the subcutaneous fat and bone marrow[14] are warranted. At some centers, endoscopic,[15] skin,[16] or salivary gland[17] biopsies are preferred, and these can be acceptable alternatives depending on the local expertise. A liver biopsy can lead to bleeding, and rarely to liver rupture,[18] but if the diagnosis is suspected, a noninvasive sampling of fat,[19] bone marrow, or skin will lead to the correct diagnosis with minimal risk. For the majority of patients, if light-chain studies are completely negative, the likelihood of light-chain systemic amyloidosis is very small and is probably not worth pursuing further. When amyloidosis is strongly suspected, biopsies are only required if the light-chain studies are abnormal. Localized forms of amyloidosis, secondary systemic amyloidosis, and familial forms of systemic amyloidosis are not associated with monoclonal light chains. The routine screening for amyloid deposits in the bone marrow of patients with multiple myeloma and smoldering myeloma is low yield and is not indicated unless the patient has symptoms consistent with amyloidosis.[20] Recommended testing for patients who have received a histologic diagnosis of light-chain amyloidosis is given in Table 2.
Prognosis
The extent of cardiac involvement determines the outcomes seen in patients with amyloidosis. Defining the extent of cardiac involvement has changed as technologies have improved. In the early 1970s, cardiac amyloid was defined using the criteria of classic congestive heart failure: the chest radiograph showed cardiomegaly, pleural effusions, and Kerley B lines.[21] In the 1980s, clinical assessment of cardiac failure was enhanced by the use of echocardiography. Thickening of the myocardial walls, a granular sparkling appearance, relaxation abnormalities seen during diastole, valvular thickening, right ventricular dysfunction, and echocardiographic strain abnormalities have all been shown to correlate with survival.[22] Cardiac amyloidosis is a classic cause of a presentation of heart failure with normal systolic function. The low cardiac output state is a consequence of poor relaxation, poor diastolic filling, and low end-diastolic volumes.
In the past 10 years, cardiac biomarker levels have developed into sensitive measures of cardiac dysfunction, are now part of the response criteria for cardiac amyloidosis, and are highly correlated with outcomes. These blood tests require no specific technical expertise and are widely available in laboratories throughout the world. The troponins T and NT-proBNP are the most thoroughly researched of the biomarkers. Using cutoffs of 0.035 µg/L for troponin T and 322 pg/mL for NT-proBNP, patients can be classified into three stages based on whether the two biomarkers are both low (stage 1), both high (stage 3), or one normal and one abnormal (stage 2). The median survivals in these patients are 26.4, 10.5, and 3.5 months, respectively, for stage 1, stage 2, and stage 3. The value of cardiac biomarkers has also been validated in patients treated with stem-cell transplantation.[23,24] The troponin T is used as an exclusion criterion for stem-cell transplantation. High-sensitivity cardiac troponin T assays are also an excellent predictor of long-term outcome.[25,26]
Other biologic factors that have predicted poor outcome include the level of the immunoglobulin free light chain at diagnosis,[27] with the free light chain level predicting early death, with a hazard ratio of 2.6. The number of organs involved also predicts survival, as does the serum uric acid level, but these features have not been incorporated into a staging system.[28,29]
Recently, new response criteria have been developed to define response. A complete response is defined as negative results on serum and urine immunofixation, a normal free light chain ratio, and normal bone marrow. A partial response is a 50% decline in the difference between involved and uninvolved serum free light chain levels (dFLC). A very good partial response has been defined as a dFLC < 40 mg/L. The new criteria for a cardiac response and cardiac progression are defined using the troponin NT-proBNP. An increase (or decrease) of 30% with a minimum absolute increase (or decrease) of 300 pg/mL are used to establish cardiac progression or response following treatment. To be considered evaluable for response, the level of pretreatment NT-proBNP must be > 600 pg/mL.[30]
Therapy of Amyloidosis in 2012
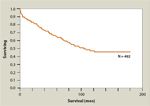
FIGURE 3

Overall Survival (OS) Among Patients With Primary Systemic Amyloidosis (AL) Based on Date of Diagnosis
Survival in AL amyloidosis has improved over time, with the greatest improvement occurring in the past decade (Figure 3).[31] However, death within the first year following diagnosis remains high at 30%. In theory, agents that interfere with the misfolding of the soluble light chain into the insoluble fibril protein should be highly desirable. Research into antibodies specific to the amyloid fibril protein[32] or to serum amyloid P,[33] an integral component of the fibril structure, has been undertaken. Exploration of interfering messenger RNAs that might block the expression of the amyloid precursor protein is also being conducted.[34] However, none of these techniques are ready for the bedside, and the mainstay of treatment since 1972[35] has been cytotoxic chemotherapy designed to destroy the plasma cells, the source of the immunoglobulin light chain that results in amyloidosis. Many of the advances in the treatment of amyloidosis are derived from our experience in the management of multiple myeloma, since both disorders share a clonal population of bone marrow plasma cells.[4] In the pretransplant era, the melphalan and prednisone–based regimens and high-dose dexamethasone therapy that were developed for multiple myeloma were explored in the treatment of light-chain amyloidosis. Melphalan and prednisone are active, but only in a minority of patients with light-chain amyloidosis.[36,37] Melphalan metabolism is minimally dependent on hepatic function and requires only minor dose modification for renal insufficiency. Dexamethasone as a single agent can produce significant organ responses in patients with amyloidosis who do not present with advanced cardiac failure.[36] There are very few patients who would not be eligible for a trial of melphalan-based treatment or single-agent corticosteroids.
FIGURE 4
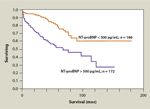
Survival of 358 Patients Treated With Myeloablative Therapy and Stem-Cell Transplantation Grouped According to Whether Pretransplant NT-proBNP Was > 500 pg/mL or < 500 pg/mLFIGURE 5
Survival of All 492 Patients With Primary Amyloidosis Who Have Received Transplants at the Mayo Clinic Since the Inception of Its Amyloidosis Transplantation Program
After stem-cell transplantation was validated as a method for improving the survival of patients with multiple myeloma, it was rapidly adapted to the management of patients with light-chain amyloidosis.[37] Unique differences in the application of this technique to these two diseases were quickly detected. Patients with multiple myeloma have a relatively high tumor mass in their marrow and preserved organ function. Thus, the consequences and the complications of high-dose therapy in myeloma were primarily associated with myelosuppression and mucositis.[38] The mortality rates for multiple myeloma transplant are approximately 0.5% when patients receive a transplant in the first plateau and 2% when patients have relapsing disease at the time of transplantation.[39] Amyloidosis, on the other hand, is characterized by a relatively small tumor mass, so small that induction chemotherapy is often not necessary before proceeding directly to high-dose therapy.[40] However, patients with amyloidosis are characterized by organ dysfunction, whether this be heart failure with preserved systolic function, massive proteinuria with resultant hypoalbuminemia, or reduced performance status related to peripheral or autonomic neuropathy. Transplantation in that setting not only carries the consequences of mucositis and myelosuppression but also hypotension, renal failure due to acute tubular necrosis, arrhythmia, intestinal bleeding from amyloid-laden blood vessels in the gastrointestinal tract, and sharp rises in serum alkaline phosphatase levels.[43-45] Thus, early trials of high-dose therapy for amyloidosis often resulted in mortality rates in the 15% range, and in the earliest studies rates approached more than 40%.[41] As centers gained experience and patient selection was improved (through the use of functional status, cardiac biomarkers [Figure 4], and free light chain levels), this mortality has been greatly reduced. Since 2006, the day-100 all-cause mortality in patients with amyloidosis at the Mayo Clinic has been 7%, and our program has not experienced any treatment-related deaths since December 2009 (n = 74).[28] For appropriately selected patients in whom it is believed stem-cell transplantation can be accomplished safely, 10-year survival is not uncommon (Figure 5). Complete hematologic responses are seen in 39%, organ responses in 47%.[42] The achievement of a very good partial response or better is the strongest predictor of outcome. For selected patients, stem-cell transplantation is an important consideration.[43]
The Use of Novel Agents in the Treatment of Light-Chain Amyloidosis
When thalidomide (Thalomid) was used as a single agent in combination with corticosteroids, hematologic responses were seen in 48% of patients, with no complete responses.[44] The treatment-related toxicity of thalidomide in amyloidosis is high; the agent is not well tolerated; and the starting dose is generally lower than that in patients with multiple myeloma, often 50 mg/day.[45] Thalidomide has been combined with cyclophosphamide and dexamethasone. The reported hematologic response rate for this regimen is 74%, with complete responses seen in 21%. Reported median overall survival from the start of therapy was 41 months, with a treatment-related mortality of 3%.[46] The use of cyclophosphamide-thalidomide-dexamethasone has the advantage of being all-oral. In addition to the usual treatment-related toxicities seen with thalidomide in patients with myeloma-somnolence, constipation, and peripheral neuropathy-patients with amyloidosis are also particularly prone to bradycardia and worsening fluid retention.
Lenalidomide
Lenalidomide (Revlimid) has been combined with dexamethasone in the treatment of light-chain amyloidosis. The associated toxicities include cytopenias, rash, fatigue, cramps, and renal dysfunction.[47] In one study, the hematologic response rate was 41%. The median overall survival was 31 months.[48] In an update of this study, progression-free survival in patients who achieved a hematologic complete response was 49.8 months.[49] Lenalidomide in combination with dexamethasone produced a hematologic complete response in 16% of previously treated patients, and 60% of the complete responses were durable.[49] A second study of lenalidomide with dexamethasone had a response rate of 67% in the patients with renal involvement; 41% of patients with renal involvement had a decrease in urinary protein excretion. High-risk patients were less likely to respond.[50]
In a phase I/II dose escalation study, lenalidomide was combined with melphalan and dexamethasone for patients with newly diagnosed amyloidosis. The maximum tolerated dose of lenalidomide when combined with melphalan and dexamethasone was 15 mg/day.[51] Hematologic responses were seen in 58%, with complete responses in 42%; 2-year event-free survival was 54%, and overall survival was 81%. Lenalidomide has also been combined with cyclophosphamide and dexamethasone. The hematologic response rate was 60%, and in patients evaluable for response (those who received four or more cycles), the hematologic response rate was 87%.[52]
Pomalidomide
Use of pomalidomide, a derivative of thalidomide with structural similaritiesto both thalidomide and lenalidomide, has been reported in 26 patients. All patients were previously treated with alkylating agents, autologous stem-cell transplantation, and in 13, prior lenalidomide or thalidomide. Nineteen patients evaluable for hematologic response had a response rate of 35%, with two confirmed and four unconfirmed organ responses.
Pomalidomide in combination with dexamethasone is a promising therapy for light-chain amyloidosis.[53]
Bortezomib
In an early study of bortezomib (Velcade), 80% of evaluable patients had a hematologic response.[54] A subsequent study of 18 patients reported hematologic responses in 77% and complete responses in 16%.[55] A phase I/II dose-escalation study of bortezomib that specifically excluded corticosteroids and that used both a biweekly and a weekly administration schedule of bortezomib reported hematologic responses in 50% of patients, 20% complete, with a median time to response of 1.2 months. One-year duration of response was 67%, and 2-year duration was 45%. Patients with New York Heart Association class III/IV heart disease were excluded from the study.[56] Bortezomib and dexamethasone have been used after stem-cell transplantation to improve the depth of response for patients who achieved less than a very good partial response. Nineteen of 28 patients received post-transplant bortezomib and dexamethasone; 67% of these achieved a complete response, 60% organ responses.[57] In a multinational survey study reporting on 94 patients who received bortezomib with or without dexamethasone, a hematologic response was seen in 71%, a complete response in 25%. A cardiac response was seen in 29%.[58] Addition of bortezomib to the high-dose melphalan (HDM) used as a conditioning regimen prior to stem-cell transplantation is feasible and well-tolerated by patients with AL amyloidosis. The combination resulted in no increase in adverse events beyond what is typically seen with HDM alone.[59]
REFERENCE GUIDE
Therapeutic Agents
Mentioned in This Article
Bendamustin (Treanda)
Bortezomib (Velcade)
Cyclophosphamide
Dexamethasone
Lenalidomide (Revlimid)
Melphalan
MLN9708
Pomalidomide
Prednisone
Thalidomide (Thalomid)
Brand names are listed in parentheses only if a drug is not available generically and is marketed as no more than two trademarked or registered products. More familiar alternative generic designations may also be included parenthetically.
Active Clinical Trials in the Management of Amyloidosis
TABLE 3

Selected Open Clinical Trials for Immunoglobulin LIght-Chain Amyloidosis
Based on the recognized single-agent activity of cyclophosphamide, melphalan, lenalidomide, bortezomib, and dexamethasone in the management of amyloidosis, a number of clinical trials are now exploring these agents in combination. These trials are listed in Table 3 and warrant specific comment. An important phase III study that is being conducted in the United States and Europe randomly assigns patients either to melphalan + dexamethasone, which is currently considered the default standard of care for non–transplant-eligible patients, or to melphalan-dexamethasone-bortezomib, based on the activity of bortezomib as a single agent as described above. Dosing of these agents is given in Table 3.
Lenalidomide is being explored in three phase II trials, combined with the alkylating agent cyclophosphamide in two and with melphalan in one. In one of the lenalidomide studies, the primary outcome is maximum tolerated dose, with the lenalidomide being increased from 5 to 25 mg/day, and cyclophosphamide from 50 to 100 mg/day. In the other lenalidomide study, which is a phase II study, the lenalidomide dose is fixed at 15 mg/day, and cyclophosphamide is fixed at 500 mg weekly.
Bortezomib is being explored as part of the induction therapy prior to stem-cell transplantation. In standard doses, bortezomib is combined with cyclophosphamide and dexamethasone (CyBorD) in an attempt to combine the rapid response rate of proteasome inhibitors with the effectiveness of alkylators. The oral proteasome inhibitor MLN9708 is also being explored in a phase I trial to determine the maximum tolerated dose and to assess whether the activity is comparable to that of bortezomib but with the added convenience of an oral regimen. Bendamustine (Treanda), which has shown activity in the treatment of multiple myeloma and low-grade lymphoma, is also being explored in combination with dexamethasone in a phase II trial in standard doses for patients with preserved renal function. Bendamustine is not approved for use in patients whose creatinine clearance is below 40 mL/min.
Relationship Between Hematologic Response and Organ Response
The endpoint of hematologic response is used primarily for rapid assessment of drug activity. Clinical benefit, however, is not dependent on hematologic response. Clinical benefit requires organ response. Reduction of urinary protein loss, improvement in echocardiographic changes, and clinically relevant reductions in NT-proBNP levels have been reported with stem-cell transplantation as well as with combination chemotherapy.[43,60] Using stem-cell transplantation, urinary protein levels as high as 21 g/24-hour period have fallen to < 0.2 g/day, a result associated with a survival of 72+ months (Gertz, unpublished). Others have reported similar organ responses.[61] Most investigators believe that an organ response cannot occur in the absence of a significant hematologic response; studies have shown that complete responders survive better than very good partial responders and that hematologic response is the best predictor of organ response and survival.[30] It is not known whether the amyloid deposits actually regress. It is believed that amyloid deposits may remain, yet significant organ healing nonetheless occurs, suggesting that soluble toxic intermediates may play a role in producing the organ dysfunction of amyloidosis.[62,63] If this is in fact the case, reduction of the free light chain level would directly impact organ dysfunction.
Conclusion
When light-chain amyloidosis is diagnosed prior to the development of advanced cardiomyopathy, systemic therapy is capable of producing hematologic responses that will translate into organ responses and prolonged survival. When a patient is seen with a compatible clinical syndrome, studies to confirm light-chain amyloidosis should be performed, and the deposits must be verified as being both systemic and light chain–derived. Some patients are appropriate candidates for stem-cell transplantation. Advances in the management of multiple myeloma are currently being translated into a variety of clinical trials designed to improve the quality of life and survival of patients with light-chain amyloidosis.
Financial Disclosure:Dr. Gertz receives honoraria from Millennium, Binding Site, and Celgene. Dr. Dispenzieri reports clinical trials for Celgene and Millennium, and has also served as an unpaid member of Millennium’s advisory board; she received a travel award from Binding Site.
References:
References
1. Baden EM, Sikkink LA, Ramirez-Alvarado M. Light chain amyloidosis-current findings and future prospects. Curr Protein Pept Sci. 2009;10:500-8.
2. Bhat A, Selmi C, Naguwa SM, et al. Currents concepts on the immunopathology of amyloidosis. Clin Rev Allergy Immunol. 2010;38:97-106.
3. Halloush RA, Lavrovskaya E, Mody DR, et al. Diagnosis and typing of systemic amyloidosis: the role of abdominal fat pad fine needle aspiration biopsy. Cytojournal. 2010;6:24.
4. Merlini G, Seldin DC, Gertz MA. Amyloidosis: pathogenesis and new therapeutic options. J Clin Oncol. 2011;29:1924-33.
5. Bellavia D, Abraham RS, Pellikka PA, et al. Utility of Doppler myocardial imaging, cardiac biomarkers, and clonal immunoglobulin genes to assess left ventricular performance and stratify risk following peripheral blood stem cell transplantation in patients with systemic light chain amyloidosis (AL). J Am Soc Echocardiogr. 2011;24:444-54.
6. Mesquita M, Fosso C, Bakoto Sol E, et al. Renal biopsy findings in Belgium: a retrospective single center analysis. Acta Clin Belg. 2011;66:104-9.
7. Katzmann JA, Kyle RA, Benson J, et al. Screening panels for detection of monoclonal gammopathies. Clin Chem. 2009;55:1517-22.
8. Gertz MA, Lacy MQ, Dispenzieri A, Hayman SR. Amyloidosis: diagnosis and management. Clin Lymphoma Myeloma. 2005;6:208-19.
9. Merlini G, Stone MJ. Dangerous small B-cell clones. Blood. 2006;108:2520-30.
10. Turesson I, Velez R, Kristinsson SY, Landgren O. Patterns of multiple myeloma during the past 5 decades: stable incidence rates for all age groups in the population but rapidly changing age distribution in the clinic. Mayo Clin Proc. 2010;85:225-30.
11. Angiero F, Seramondi R, Magistro S, et al. Amyloid deposition in the tongue: clinical and histopathological profile. Anticancer Res. 2010;30:3009-14.
12. Lee HJ, Chang SE, Lee MW, et al. Systemic amyloidosis associated with multiple myeloma presenting as periorbital purpura. J Dermatol. 2008;35:371-2.
13. Dispenzieri A, Kyle R, Merlini G, et al. International Myeloma Working Group guidelines for serum-free light chain analysis in multiple myeloma and related disorders. Leukemia. 2009;23:215-24.
14. Petruzziello F, Zeppa P, Catalano L, et al. Amyloid in bone marrow smears of patients affected by multiple myeloma. Ann Hematol. 2010;89:469-74.
15. Ohno F, Numata Y, Yamano T, et al. Gastroscopic biopsy of the stomach for the diagnosis of amyloidosis. Gastroenterol Jpn. 1982;17:415-21.
16. Fernandez-Flores A. Comparative study of Congo red fluorescence and immunohistochemistry in cutaneous amyloidosis. Rom J Morphol Embryol. 2010;51:683-6.
17. Foli A, Palladini G, Caporali R, et al. The role of minor salivary gland biopsy in the diagnosis of systemic amyloidosis: results of a prospective study in 62 patients. Amyloid. 2011;18(Suppl 1):75-7.
18. Tam M, Seldin DC, Forbes BM, et al. Spontaneous rupture of the liver in a patient with systemic AL amyloidosis undergoing treatment with high-dose melphalan and autologous stem cell transplantation: a case report with literature review. Amyloid. 2009;16:103-7.
19. Shidham VB, Hunt B, Jardeh SS, et al. Performing and processing FNA of anterior fat pad for amyloid. J Vis Exp. 2010; 44: pii 1747.
20. Siragusa S, Morice W, Gertz MA, et al. Asymptomatic immunoglobulin light chain amyloidosis (AL) at the time of diagnostic bone marrow biopsy in newly diagnosed patients with multiple myeloma and smoldering myeloma. A series of 144 cases and a review of the literature. Ann Hematol. 2011;90:101-6.
21. Shah KB, Inoue Y, Mehra MR. Amyloidosis and the heart: a comprehensive review. Arch Intern Med. 2006;166:1805-13.
22. Liu D, Niemann M, Hu K, et al. Echocardiographic evaluation of systolic and diastolic function in patients with cardiac amyloidosis. Am J Cardiol. 2011;108:591-8.
23. Dispenzieri A, Gertz MA, Kyle RA, et al. Serum cardiac troponins and N-terminal pro-brain natriuretic peptide: a staging system for primary systemic amyloidosis. J Clin Oncol. 2004;22:3751-7.
24. Dispenzieri A, Gertz MA, Kyle RA, et al. Prognostication of survival using cardiac troponins and N-terminal pro-brain natriuretic peptide in patients with primary systemic amyloidosis undergoing peripheral blood stem cell transplantation. Blood. 2004;104:1881-7.
25. Palladini G, Barassi A, Klersy C, et al. The combination of high-sensitivity cardiac troponin T (hs-cTnT) at presentation and changes in N-terminal natriuretic peptide type B (NT-proBNP) after chemotherapy best predicts survival in AL amyloidosis. Blood. 2010;116:3426-30.
26. Gertz M, Lacy M, Dispenzieri A, et al. Troponin T level as an exclusion criterion for stem cell transplantation in light-chain amyloidosis. Leuk Lymphoma. 2008;49:36-41.
27. Dispenzieri A, Lacy MQ, Katzmann JA, et al. Absolute values of immunoglobulin free light chains are prognostic in patients with primary systemic amyloidosis undergoing peripheral blood stem cell transplantation. Blood. 2006;107:3378-83.
28. Gertz MA, Lacy MQ, Dispenzieri A, et al. Trends in day 100 and 2-year survival after auto-SCT for AL amyloidosis: outcomes before and after 2006. Bone Marrow Transplant. 2011;46:970-5.
29. Kumar S, Dispenzieri A, Lacy MQ, et al. Serum uric acid: novel prognostic factor in primary systemic amyloidosis. Mayo Clin Proc. 2008;83:297-303.
30. Palladini G, Dispenzieri A, Gertz MA, et al. Validation of the criteria of response to treatment in AL amyloidosis. ASH Annual Meeting Abstracts 2010;116:1364.
31. Kumar SK, Gertz MA, Lacy MQ, et al. Recent improvements in survival in primary systemic amyloidosis and the importance of an early mortality risk score. Mayo Clin Proc. 2011;86:12-8.
32. Wall JS, Kennel SJ, Stuckey AC, et al. Radioimmunodetection of amyloid deposits in patients with AL amyloidosis. Blood. 2010;116:2241-4.
33. Bodin K, Ellmerich S, Kahan MC, et al. Antibodies to human serum amyloid P component eliminate visceral amyloid deposits. Nature. 2010;468:93-7.
34. Hovey BM, Ward JE, Soo Hoo P, et al. Preclinical development of siRNA therapeutics for AL amyloidosis. Gene Ther. 2011;18:1150-6.
35. Jones NF, Hilton PJ, Tighe JR Hobbs JR. Treatment of "primary" renal amyloidosis with melphalan. Lancet. 1972;2:616-9.
36. Dhodapkar MV, Hussein MA, Rasmussen E, et al. Clinical efficacy of high-dose dexamethasone with maintenance dexamethasone/alpha interferon in patients with primary systemic amyloidosis: results of United States Intergroup Trial Southwest Oncology Group (SWOG) S9628. Blood. 2004;104:3520-6.
37. Comenzo RL. Who knows how to treat systemic light chain amyloidosis? Oncology (Williston Park). 2011;25:626, 28-9, 32-3.
38. Cavo M, Rajkumar SV, Palumbo A, et al. International Myeloma Working Group consensus approach to the treatment of multiple myeloma patients who are candidates for autologous stem cell transplantation. Blood. 2011;117:6063-73.
39. Gertz MA, Ansell SM, Dingli D, et al. Autologous stem cell transplant in 716 patients with multiple myeloma: low treatment-related mortality, feasibility of outpatient transplant, and effect of a multidisciplinary quality initiative. Mayo Clin Proc. 2008;83:1131-8.
40. Madan S, Kumar S, Lacy MQ, et al. Pre-stem cell transplant induction therapy does not affect post-transplant survival in light chain (AL) amyloidosis. ASH Annual Meeting Abstracts. 2010;116:370.
41. Chow LQ, Bahlis N, Russell J, et al. Autologous transplantation for primary systemic AL amyloidosis is feasible outside a major amyloidosis referral centre: the Calgary BMT Program experience. Bone Marrow Transplant. 2005;36:591-6.
42. Gertz MA, Lacy MQ, Dispenzieri A, et al. Autologous stem cell transplant for immunoglobulin light chain amyloidosis: a status report. Leuk Lymphoma. 2010;51:2181-7.
43. Cibeira MT, Sanchorawala V, Seldin DC, et al. Outcome of AL amyloidosis after high-dose melphalan and autologous stem cell transplantation: long-term results in a series of 421 patients. Blood. 2011;118:4346-52.
44. Seldin DC, Choufani EB, Dember LM, et al. Tolerability and efficacy of thalidomide for the treatment of patients with light chain-associated (AL) amyloidosis. Clin Lymphoma. 2003;3:241-6.
45. Palladini G, Perfetti V, Perlini S, et al. The combination of thalidomide and intermediate-dose dexamethasone is an effective but toxic treatment for patients with primary amyloidosis (AL). Blood. 2005;105:2949-51.
46. Wechalekar AD, Goodman HJ, Lachmann HJ, et al. Safety and efficacy of risk-adapted cyclophosphamide, thalidomide, and dexamethasone in systemic AL amyloidosis. Blood. 2007;109:457-64.
47. Specter R, Sanchorawala V, Seldin DC, et al. Kidney dysfunction during lenalidomide treatment for AL amyloidosis. Nephrol Dial Transplant. 2011;26:881-6.
48. Sanchorawala V, Wright DG, Rosenzweig M, et al. Lenalidomide and dexamethasone in the treatment of AL amyloidosis: results of a phase 2 trial. Blood. 2007;109:492-6.
49. Sanchorawala V, Finn KT, Fennessey S, et al. Durable hematologic complete responses can be achieved with lenalidomide in AL amyloidosis. Blood. 2010;116:1990-1.
50. Palladini G, Russo P, Foli A, et al. Salvage therapy with lenalidomide and dexamethasone in patients with advanced AL amyloidosis refractory to melphalan, bortezomib, and thalidomide. Ann Hematol. 2012;91:89-92.
51. Moreau P, Jaccard A, Benboubker L, et al. Lenalidomide in combination with melphalan and dexamethasone in patients with newly diagnosed AL amyloidosis: a multicenter phase 1/2 dose-escalation study. Blood. 2010;116:4777-82.
52. Kumar S, Hayman SR, Buadi F. A phase II trial of lenalidomide, cyclophosphamide and dexamethasone (RCD) in patients with light chain amyloidosis [abstract 3853]. Blood. 2009;114:1482.
53. Dispenzieri A, Gertz MA Hayman SR. A pilot study of pomalidomide and dexamethasone in previously treated light chain amyloidosis patients [abstract 3854]. Blood. 2009;114:1482-3.
54. Wechalekar AD, Lachmann HJ, Offer M, et al. Efficacy of bortezomib in systemic AL amyloidosis with relapsed/refractory clonal disease. Haematologica. 2008;93:295-8.
55. Kastritis E, Anagnostopoulos A, Roussou M, et al. Treatment of light chain (AL) amyloidosis with the combination of bortezomib and dexamethasone. Haematologica. 2007;92:1351-8.
56. Reece DE, Hegenbart U, Sanchorawala V, et al. Efficacy and safety of once-weekly and twice-weekly bortezomib in patients with relapsed systemic AL amyloidosis: results of a phase 1/2 study. Blood. 2011;118:865-73.
57. Landau H, Hassoun H, Bello C, et al. Consolidation with bortezomib and dexamethasone following risk-adapted melphalan and stem cell transplant in systemic AL amyloidosis. Amyloid. 2011;18(Suppl 1):130-1.
58. Kastritis E, Wechalekar AD, Dimopoulos MA, et al. Bortezomib with or without dexamethasone in primary systemic (light chain) amyloidosis. J Clin Oncol. 2010;28:1031-7.
59. Sanchorawala V, Quillen K, Sloan JM, et al. Bortezomib and high dose melphalan conditioning for stem cell transplantation for AL amyloidosis: a pilot study. Haematologica. 2011;96:1890-2.
60. Lamm W, Willenbacher W, Lang A, et al. Efficacy of the combination of bortezomib and dexamethasone in systemic AL amyloidosis. Ann Hematol. 2011;
90:201-6.
61. Kumar SK, Dispenzieri A, Lacy MQ, et al. Changes in serum-free light chain rather than intact monoclonal immunoglobulin levels predicts outcome following therapy in primary amyloidosis. Am J Hematol. 2011;86:251-5.
62. Herrera GA, Teng J, Turbat-Herrera EA. Renal amyloidosis: current views on pathogenesis and impact on diagnosis. Contrib Nephrol. 2011;169:232-46.
63. Sikkink LA Ramirez-Alvarado M. Cytotoxicity of amyloidogenic immunoglobulin light chains in cell culture. Cell Death Dis. 2010;1:e98.
Navigating AE Management for Cellular Therapy Across Hematologic Cancers
A panel of clinical pharmacists discussed strategies for mitigating toxicities across different multiple myeloma, lymphoma, and leukemia populations.