A Rare Case of Glioblastoma With Extensive Liver Metastases
Ghulam Gous, MD, and colleagues report a case of glioblastoma with extensive liver metastases along with a review of previous reports of liver metastasis from glioblastomas and the possible mechanisms of metastasis.
Introduction
Glioblastomas (GBM) are the most common and the most aggressive malignant brain tumor originating from glial cells.1 They arise either de novo (primary glioblastoma) or from lower-grade diffuse gliomas (secondary glioblastoma), sometimes after many years. It has an annual incidence in the United States of 3 per 100,000 people, with approximately 12,500 cases per year.2 The peak age of presentation is in later adult life; median survival is about 13 months and 5-year survival is well under 5%.1-4
Bailey and Cushing initially described leptomeningeal metastases of intracranial gliomas in 1926 and stated that such tumors would not have extracranial metastases.4,5 However, Davis provided the first description of extracranial GBM metastasis in 1928.6 The recognition and thus apparent incidence of extracranial metastases from GBM has increased from a frequency of only 0.44% in 19693 to 2% at present; some of this increase may be real, and some of it may be due to longer survivals with modern therapy.7 One review article reported that extraneural metastases of GBM included spread to lung and pleura (60%), cervical lymph nodes (51%), bone (31%), and only rarely liver (20%).8 Yet more unusual examples of metastatic glioblastoma were also reported in heart, adrenal gland, kidney, diaphragm, mediastinum, and pancreas. The median time for detection of such distant spread following diagnosis of the primary brain tumor is reported as 8.5 months, and the median time from that diagnosis to death is 1.5 months.9 We report a case of GBM with extensive liver metastases along with a review of previous reports of liver metastasis from GBMs, and we discuss the possible mechanisms of metastasis.
Oncology (Williston Park). 2021;35(11):733-740.
DOI: 10.46883/ONC.2021.3511.0733
Case Presentation
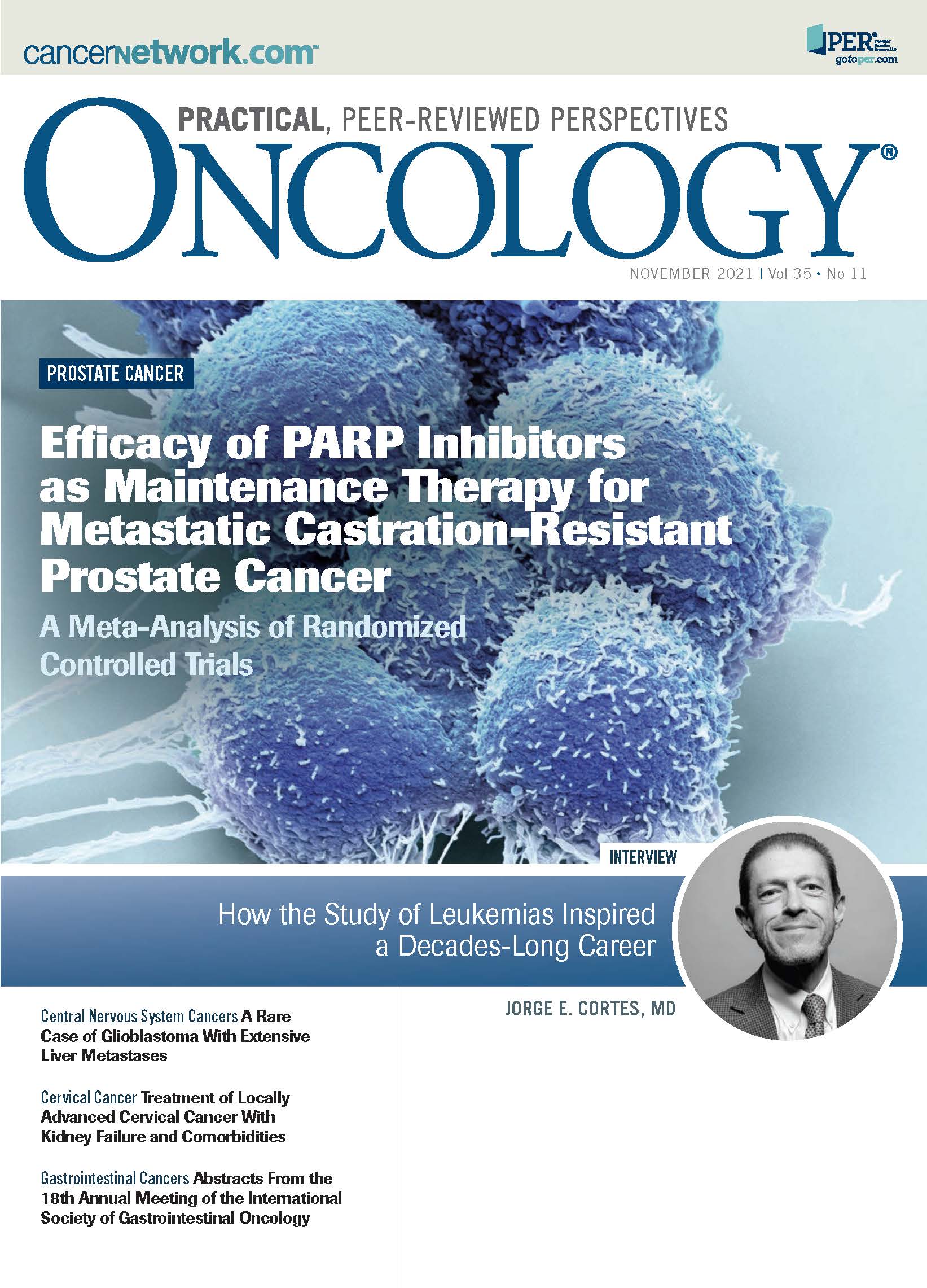
A man aged 65 years had a history of a benign lung mass (resected in 1985), papillary thyroid cancer (status post thyroidectomy performed in 2016), and a recent diagnosis of prostate cancer (Gleason grade 3+3; prostate-specific antigen [PSA] 6.25 ng/mL in 2018); he presented to an outside hospital because of progressive headache and leg weakness over the prior 2 weeks. Physical examination was normal. CT scans showed a right frontal mass with 1 cm of midline shift (Figure 1A), a 1.4-cm (greatest dimension) left lower lobe lung nodule (Figure 1B), and a 3.3-cm × 2.1-cm hypodense lesion in the left hepatic lobe (Figure 1C). He was transferred to our hospital. MRI revealed a 5.6-cm × 6.5-cm × 6.1-cm ovoid, lobulated, predominantly peripherally enhancing mass within the right frontal lobe, with multiple foci of hemorrhage (Figure 2A). The tumor was gross totally excised and was discovered to be an IDH wild-type glioblastoma that had no MGMT promoter methylation, and no mutation of ATRX. His hospital course was complicated by an acute pulmonary embolism requiring placement of an inferior vena cava filter. He was ultimately discharged to a rehabilitation facility. Subsequently, he was seen in our medical oncology clinic and scheduled for concurrent temozolomide (Temodar) and external beam radiation therapy, as per the typical Stupp regimen.10
FIGURE 1. CT Scans of Brain, Chest, and Liver at Initial Presentation
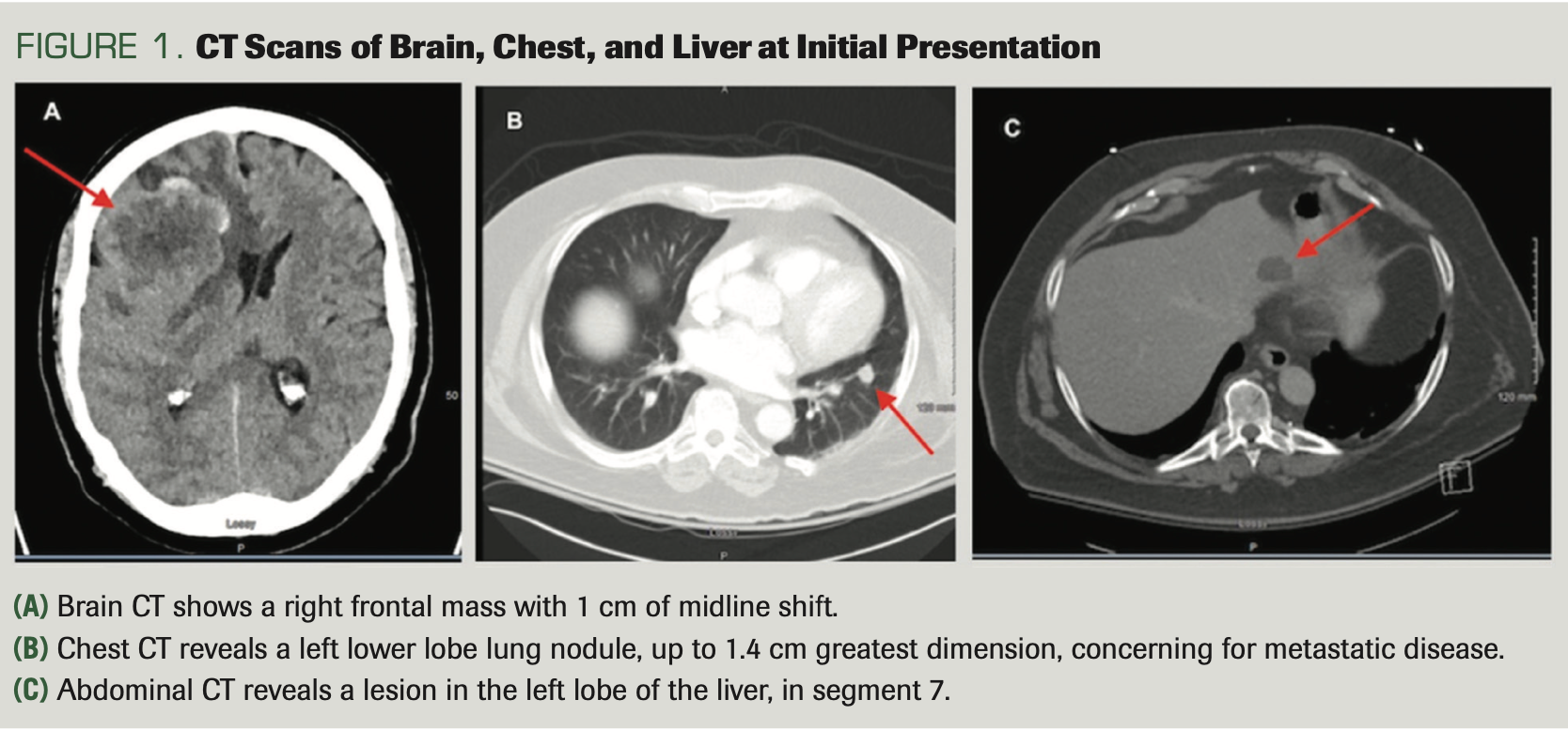
However, prior to initiating the treatment, he was readmitted for dizziness and worsening of left-sided weakness. A repeat MRI revealed a significant recurrent enhancing mass at the prior resection site affecting the underlying brain parenchyma, with approximately 1.1 cm of midline shift (Figure 2B). The recurrent tumor was resected, along with extensive debridement of subcutaneous, epidural, and intraparenchymal scar tissue. Pathologically, it was recurrent glioblastoma. It is noteworthy that the patient did not need any ventriculoperitoneal shunt (VPS) at any stage. During this surgery, the patient was found to have a stitch abscess with subcutaneous and possible bone flap involvement. Additionally, cultures showed subcutaneous tissue diphtheroids, coagulase-negative Staphylococcus, diphtheroids, Candida parapsilosis, and Cutibacterium. He was discharged on intravenous vancomycin and fluconazole for more than 4 weeks.
Unfortunately, the patient did not receive adjuvant oral temozolomide/radiation therapy in a timely fashion due to infection, and he subsequently presented with altered mental status (AMS), acute kidney injury (AKI), and septic shock. Brain MRI done outside hospital as part of the AMS work-up showed a new lesion in the left parietal region and the patient was then transferred again to our hospital. A new brain MRI confirmed additional new lesions within the right frontotemporal region and in the left parietal lobe (Figure 2C). As part of the AKI work-up, ultrasonography and MRI of his abdomen revealed innumerable presumed metastatic lesions involving all hepatic segments (Figure 3). Liver biopsy revealed a metastatic epithelioid malignancy that was histologically identical to the intracerebral glioblastoma. He died a little more than a week later.
FIGURE 2. MRI of the Brain
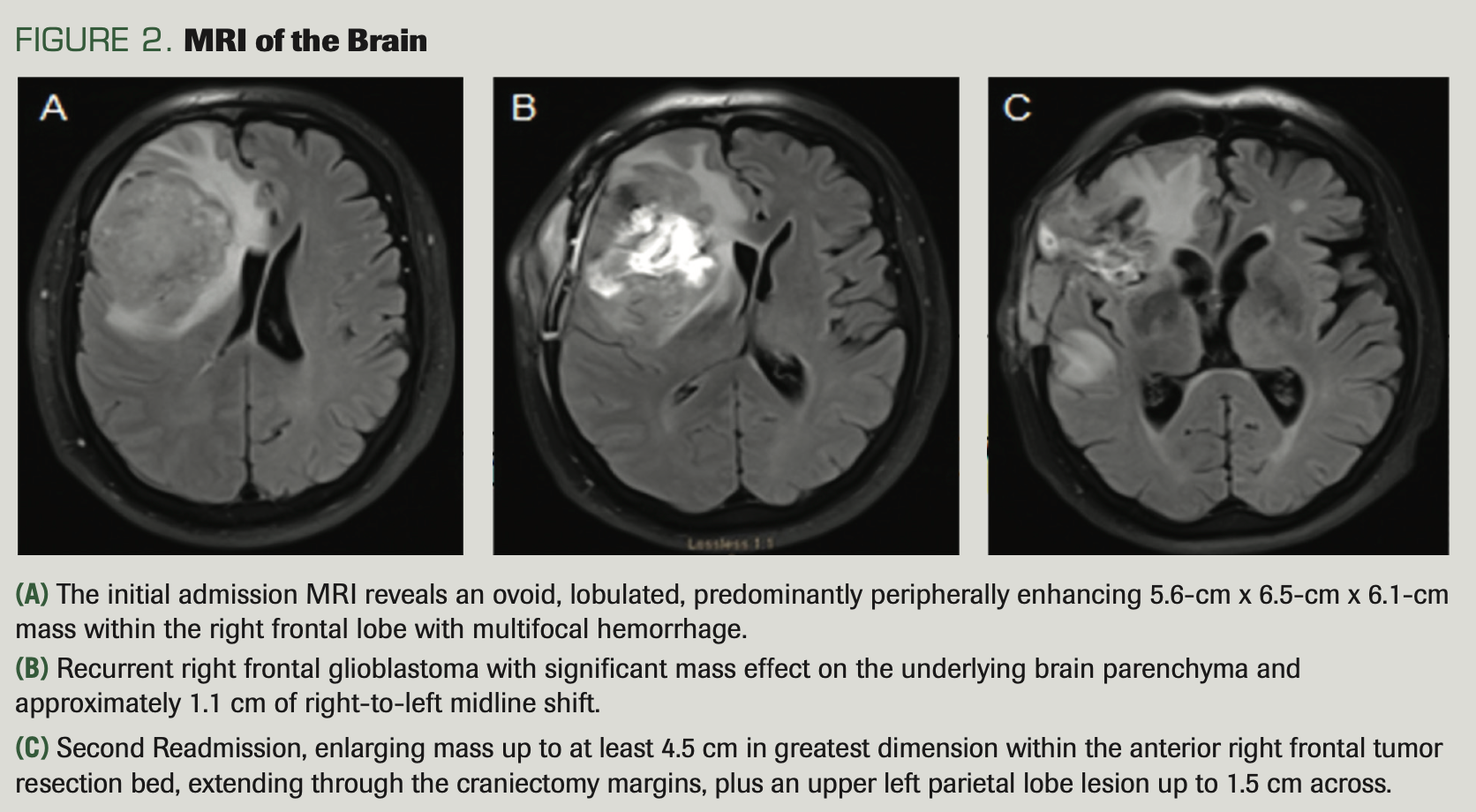
FIGURE 3. MRI Liver
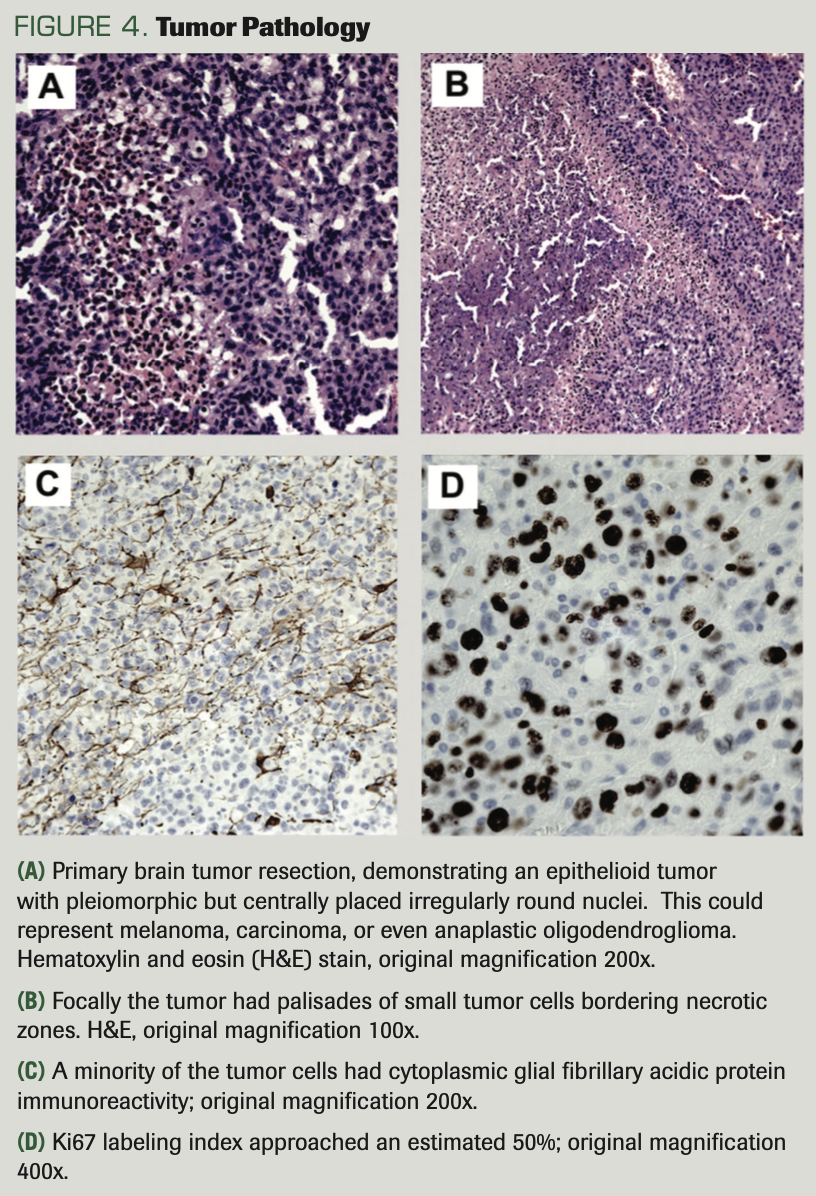
Tumor Pathology
The initial resection yielded a piece of cerebral tissue measuring 7.2 cm × 5.1 cm × 1.4 cm that was mostly replaced by tumor, with extensive necrosis. The tumor had an epithelioid growth pattern with round to polygonal cells with mostly centrally placed pleiomorphic nuclei with substantial mitotic activity (Figure 4A). In a few foci, the necrosis was bordered by a palisade of small tumor cells (Figure 4B). Initially, because there was no edge in the specimen with normal brain to assess infiltrative growth, it was thought the tumor might be metastatic, but a broad panel of immunostains established that it was not carcinoma, germ cell tumor, or melanoma: Specifically, there was no immunoreactivity for cytokeratins (cytokeratin 7, cytokeratin 20, antibody CAM5.2), thyroid transcription factor 1 (TTF1), Napsin, P40, CDX2, PSA, HMB45, or MART-1/Melan-A (antibody A103). These results tended to rule out carcinomas (cytokeratins negative)—specifically, carcinomas including pulmonary non–small cell carcinomas (TTF1, Napsin, P40), gastrointestinal primary carcinomas (CDX2), prostatic carcinoma, and melanomas (HMB45, MART-1). A germ cell origin was also considered, but immunostains for Oct3/4 and alpha-fetoprotein were both negative.
These results prompted a panel of immunostains appropriate for gliomas, which revealed extensive cytoplasmic immunopositivity for vimentin, rare tumor cells with cytoplasmic glial fibrillary acidic protein (GFAP) immunoreactivity (Figure 4C); no cells were immunopositive for synaptophysin or neurofilament protein (neurofilament protein, antibody RMDO20). There was extensive nuclear immunoreactivity for the neuronal marker Neu-N. These results favored a poorly differentiated (poor GFAP expression), high-grade glioma (glioblastoma) with aberrant neuronal (Neu-N) immunoreactivity. This was further confirmed by the demonstration of an infiltrative pattern of growth, with entrapped axons immunopositive for NFP, some still myelinated as shown with a Luxol fast blue (LFB) stain, as well as single infiltrating tumor cells in adjacent intact LFB-positive white matter. A Ki67 immunostain marked an estimated 50% of the tumor cell nuclei (Figure 4D). There was no immunoreactivity for the protein product of the IDH1 R132H mutation, whereas an immunostain for the ATRX protein marked all of the tumor cell nuclei, indicating no mutation or deletion of the ATRX gene. Further assays revealed no methylation of the MGMT promoter and no co-deletion of chromosome arms 1p and 19q (thus, with the IDH result, ruling out oligodendroglioma). The fluorescence in situ hybridization assay suggested that the tumor was tetraploid. Given the patient’s age and the lack of MGMT methylation, the IDH genes were not sequenced.
FIGURE 4. Tumor Pathology
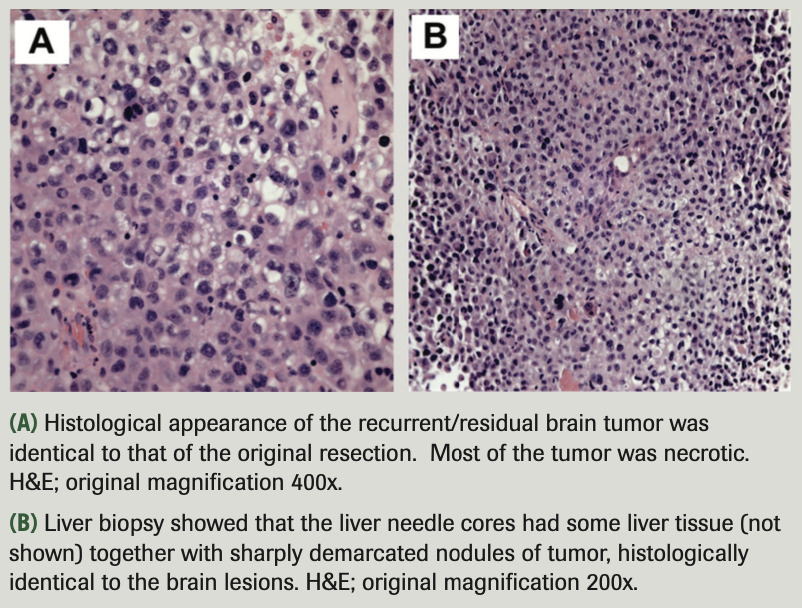
The recurrent brain tumor from the second craniotomy was histologically identical to the first (Figure 5A); like the original, it was mostly necrotic. The liver biopsy demonstrated a tumor with an identical histological appearance (Figure 5B). This tumor, like the initially resected brain tumor, had no immunoreactivity for cytokeratins (antibody cocktail AE1/AE3, cytokeratin 7, cytokeratin 20), TTF1, or CDX2. Unlike the brain lesion, this tumor lacked any GFAP immunoreactivity, but it was vimentin and Neu-N immunoreactive.
FIGURE 5. Tumor Pathology
Discussion
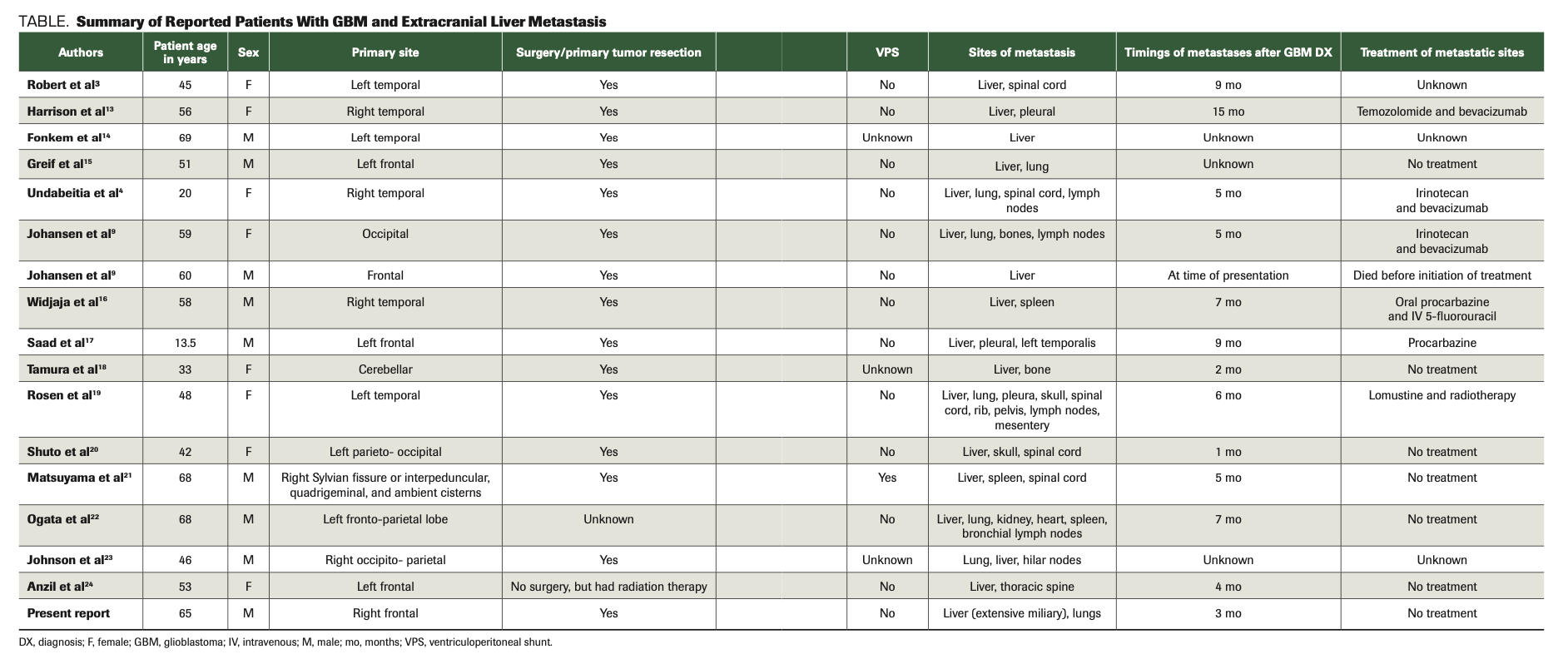
GBMs are highly aggressive brain cancers. They usually grow and infiltrate through white matter, and they then spread contiguously by infiltration into the adjacent tissues, including crossing the corpus callosum to the opposite cerebral hemisphere. Distant spread occurs within the central nervous system (CNS) via cerebrospinal fluid (CSF) pathways,11 and, in a small minority of cases, to systemic body sites by hematogenous routes. In 1969, an extensive review based on the autopsy findings of 18,000 patients with brain tumors reported only 35 well-documented cases of distant hematogenous metastatic spread that were GBM.12 These metastases involved cervical and mediastinal regional lymph nodes, lung, liver, and bone.12 Rare metastases were also reported in the heart, adrenal gland, kidney, diaphragm, mediastinum, and pancreas.8 Most of the described cases with liver metastases had a single or a few metastatic tumors; only 1 case reported 4 or more metastatic liver lesions3 (Table3,4,9,13-24). To our knowledge, our case is the first GBM case reported to have extensive miliary liver metastases.
TABLE. Summary of Reported Patients With GBM and Extracranial Liver Metastasis
Extraneural metastasis of GBM is rare for a number of reasons: The blood-brain barrier (BBB) probably constitutes a significant barrier for the invasion of tumor cells through vessel walls; the intracranial sinuses are enclosed in a dense dural membrane, making penetration by tumor cells difficult; and the intracerebral veins are thin-walled and would probably collapse from compression before they could be penetrated by an expanding tumor.25 Additionally, glioma cells do not often express fibronectin,26,27 and the lack of collagen and fibronectin within the CNS makes glioma cells have a relatively poor affinity for vascular walls, making direct vascular endothelial invasion and subsequent extracranial seeding more difficult.26,27
The dynamics of a well-described molecular mechanism for GBM extracranial metastasis are unclear. However, it has been reported that such metastatic spread is associated with seeding of cells iatrogenically, during stereotactic biopsy, craniotomy, placement of ventriculoperitoneal shunts, or radiation therapy.28-30 According to this hypothesis, medical procedures or radiation therapy (other than VPS, which causes direct seeding) destroy the local BBB, thereby facilitating metastasis.
We reviewed all of the available literature of GBM with liver metastasis from PubMed through March 2021. Based on this review, almost all of the liver metastases occurred after initial neurosurgery to remove the primary GBM. Only 1 patient had not undergone surgery prior to the development of liver tumors; instead, he had undergone radiation therapy, which is also consistent with this hypothesis. In a hypothetical patient who did not undergo any neurosurgical procedures or radiation therapy, the progression of GBM might also destroy and invade into surrounding tissues including the BBB, an artery or vein, CSF, and dural venous spaces,24 finally leading to hematogenous distant metastasis. This was the case in our patient, who had liver and lung metastases at presentation. This demonstrates that extraneural metastases can also spontaneously arise from a primary GBM of the brain, and that neither cranial surgery nor radiation therapy are prerequisites for the distal extraneural spread of glioblastomas. Lymphatic metastasis might also exist and lead to GBM extracranial metastasis.
Two recent exciting discoveries in brain physiology and anatomy were the CNS glymphatic system31 and the CNS (dural) lymphatic system in 2015.32 Based on these discoveries, it is likely that brain parenchymal CSF permeates into the glymphatic system, which is then connected with the meningeal lymphatic system. The meningeal lymphatic system drains CSF to dural lymphatic vessels. Most importantly, the dural lymphatic vessels are able to carry CSF fluid, CNS antigens, and immune cells to deep cervical lymph nodes.33 This suggests an opportunity for GBM cells to migrate and metastasize to deep cervical lymph nodes, finally circulating into blood and escaping the CNS.
Once GBM cells circulate into the peripheral blood, the explanation of how these tumor cells metastasize to liver or other extracranial organs remains elusive. The “seed and soil” hypothesis proposed that some tumor cells selectively metastasize to specific regions within a given organ, indicating either a need of the tumor cells to grow only in a similar microenvironment, or that there are surface markers on the tumor cells that specifically bind to receptors on organ- or site-specific endothelial cells.34 In a study that screened different cancers for overexpression of tissue-selective genes, it was shown that glioblastoma selectively overexpressed genes that were also overexpressed in lung cancer (26 genes) and liver cancer (18 genes).35 The results of this study suggested that tumors might prefer to metastasize to organs that harbor cells with similar overexpressed tissue-selective cancer genes, providing the rationale for organotropism. Additionally, circulating GBM cells have been shown to have a mesenchymal expression profile; some investigators have theorized that this accounts for these cells’ ability to obtain access to the bloodstream.
Muller et al first reported that 20% of patients with GBM have circulating GBM cells in the peripheral blood; such a number obviously represents more frequency than the reported incidence of extracranial metastases of GBM in 2012.33 The circulating GBM cells could be used to predict response to treatment and to ascertain the differential diagnosis between CNS GBM recurrence and radiation necrosis.33 Gene amplification of the EGFR has been observed in 40% of glioblastomas,36 and it has been observed that some circulating GBM cells have EGFR amplification,indicating that EGFR signaling might support the extracranial spread of GBM.37,38 The TGF-alpha/EGFR signaling pathway plays a key role in colon cancer hepatic metastasis.39 Clinically, the combination of the EGFR inhibitor panitumumab (Vectibix) with cetuximab (Erbitux) has been used to treat unresectable metastatic colon cancer. However, the questions of whether GBM hepatic metastasis is also associated with EGFR overexpression, and whether EGFR could be a target for metastatic GBM treatment, have not yet been investigated.
The immune system might also play a role in GBM extracranial metastasis. This notion was supported by the detection of extracranial glioblastomas in the recipients of transplanted organs from glioblastoma donors. About 12.5% to 25% of organ donors with glioblastoma might transmit the tumor to the organ recipient.33 In a review of 11 patients who received solid organ transplants donated from patients with GBM, all 3 liver transplant patients developed GBM liver metastasis with a mean survival of 7 months; all 3 kidney transplant patients had kidney metastasis, with a mean survival of 17.3 months; and 4 of the 5 lung transplant patients developed lung metastasis.40-43 It has also been shown that GBM will grow subcutaneously in an immune-deficient mouse model.
In most patients with GBM, growth and proliferation of these extracranial glioblastomas are probably suppressed by the peripheral immune system.33 However, in posttransplant patients, the immune system is iatrogenically suppressed and conceivably could not kill the circulating GBM cells. Additionally, the mTOR inhibitor(s) can also cause an abnormality of glucose metabolism, which may lead to T cell exhaustion.44 In contrast, the CNS has traditionally been thought to be immune privileged. Glioblastomas have immunosuppressive microenvironment due to expression of programmed death-ligand 1 (PD-L1) on GBMs, tumor-associated macrophages, and abnormal regulation of cytokines. This immunosuppressive microenvironment helps to evade immune attack33; therefore, checkpoint inhibitors do not work well in the CNS even if GBM cells have a moderate-to-high PD-L1 expression. However, once GBM cells circulate into the blood and lose their immunosuppressive microenvironment, whether checkpoint inhibitors would start to work and kill these single GMB cells or cell clusters is unknown.
Extracranial GBM metastasis has no well-established treatment. With limited data, options could include up-front temozolomide, bevacizumab (Avastin) with carboplatin, or docetaxel with carboplatin. Other possibilities are older regimens like cyclophosphamide, doxorubicin (Adriamycin), and etoposide. One obstacle to investigating GBM metastasis and treatment is the lack of ideal animal models. Conventional mouse models would not mimic the human BBB and immune systems. However, inspired by the development of 3-dimensional organoids cultured from patients with colorectal cancer45 and co-culturing of intestinal epithelial organoids with local immune response, some investigators have now developed cerebral organoid models.46 Recently, BBB organoids have also been developed to investigate the permeability of CNS therapeutics across the BBB.47 In the near future, third-generation DNA sequencing could detect the gene expression profile of a single circulating GBM cell in the blood and might predict the response to treatment and the location
of metastasis.
Conclusions
In summary, we report a rare case of GBM with extensive miliary liver metastasis in a patient who had 2 craniotomies and who did not receive chemotherapy and radiation therapy. The mechanism of extracranial metastasis in this particular patient is not known. However, it has been shown that iatrogenic, hematogenous, and lymphatic dissemination may all be possible. Circulating GBM cells have been detected even before surgery in many patients. These circulating GBM cells are believed to predict early recurrence in the posttreatment setting, and we believe that results of current research will afford the field with a diagnostic tool for differentiation between early recurrence and radionecrosis. The advancement of new cerebral organoids, BBB organoids, and other state-of-the-art biotechnologies will help further explore the pathogenesis of GBM tumorigenesis and metastasis, as well as support the development of novel therapeutics. Comparing molecular abnormalities within matched primary and metastatic tumors will better allow us to understand the mechanisms behind these rare distant metastatic occurrences, as will utilizing matched organoids.
ACKNOWLEDGMENTS: The authors would like to thank all members of the treatment team, the patient and their family, and the University of Missouri – Columbia hematology/oncology department.
CONFLICT OF INTEREST: The authors declare that there is no conflict of interest regarding the publication of this article.
FUNDING: None.
References
1. Louis DN, Perry A, Reifenberger G, et al. The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary. Acta Neuropathol. 2016;131(6):803-820. doi:10.1007/s00401-016-1545-1
2. Ostrom QT, Gittleman H, Liao P, et al. CBTRUS Statistical Report: primary brain and other central nervous system tumors diagnosed in the United States in 2010-2014. Neuro Oncol. 2017;19(suppl 5):v1-v88. doi:10.1093/neuonc/nox158
3. Robert Mc, Wastie MI. Glioblastoma multiforme: a rare manifestation of extensive liver and bone metastases. Biomed Imaging Interv J. 2008;4(1):e3. doi:10.2349/biij.4.1.e3
4. Undabeitia J, Castle M, Arrazola M, Pendleton C, Ruiz I, Úrculo E. Multiple extraneural metastasis of glioblastoma multiforme. An Sist Sanit Navar. 2015;38(1):157-161. doi:10.23938/ASSN.0061
5. Bailey P, Cushing H. A classification of the tumours of the glioma group on a histogenetic basis, with a correlated study of prognosis. JAMA. 1926;87(4):268. doi:10.1001/jama.1926.02680040056039
6. Davis L. Spongioblastoma multiforme of the brain. Ann Surg. 1928;87(1):8-14.
7. Piccirilli M, Brunetto GMF, Rocchi G, Giangaspero F, Salvati M. Extra central nervous system metastases from cerebral glioblastoma multiforme in elderly patients. clinico-pathological remarks on our series of seven cases and critical review of the literature. Tumori. 2008;94(1):40-51.
8. Pasquier B, Pasquier D, N’Golet A, Panh MH, Couderc P. Extraneural metastases of astrocytomas and glioblastomas: clinicopathological study of two cases and review of literature. Cancer. 1980;45(1):112-125. doi:10.1002/1097-0142(19800101)45:1<112::aid-cncr2820450121>3.0.co;2-9
9. Dinche Johansen M, Rochat P, Law I, Scheie D, Skovgaard Poulsen H, Muhic A. Presentation of two cases with early extracranial metastases from glioblastoma and review of the literature. Case Rep Oncol Med. 2016;2016:8190950. doi:10.1155/2016/8190950
10. Stupp R, Mason WP, van den Bent MJ, et al; European Organisation for Research and Treatment of Cancer Brain Tumor and Radiotherapy Groups; National Cancer Institute of Canada Clinical Trials Group. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med. 2005;352(10):987-996. doi:10.1056/NEJMoa043330
11. Onda K, Tanaka R, Takahashi H, Takeda N, Ikuta F. Cerebral glioblastoma with cerebrospinal fluid dissemination: a clinicopathological study of 14 cases examined by complete autopsy. Neurosurgery. 1989;25(4):533-540.
12. Smith DR, Hardman JM, Earle KM. Metastasizing neuroectodermal tumors of the central nervous system. J Neurosurg. 1969;31(1):50-58. doi:10.3171/jns.1969.31.1.0050
13. Harrison WT, Hulette CM, Guy C, Sporn T, Cummings T. Metastatic glioblastoma: a case report and review of the literature. J Med Surg Pathol. 2016;1(2):1000115. doi:10.4172/2472-4971.1000115
14. Fonkem E, Lun M, Wong ET. Rare phenomenon of extracranial metastasis of glioblastoma. J Clin Oncol. 2011;29(34):4594-4595. doi:10.1200/JCO.2011.39.0187
15. Greif J, Horovitz M, Marmor S. Pleuropulmonary metastasis from an intracranial glioblastoma. Lung Cancer. 1998;20(2):135-137. doi:10.1016/s0169-5002(98)00029-4
16. Widjaja A, Mix H, Gölkel C, et al. Uncommon metastasis of a glioblastoma multiforme in liver and spleen. Digestion. 2000;61(3):219-222. doi:10.1159/000007761
17. Saad AG, Sachs J, Turner CD, et al. Extracranial metastases of glioblastoma in a child: case report and review of the literature. J Pediatr Hematol Oncol. 2007;29(3):190-194. doi:10.1097/MPH.0b013e31803350a7
18. Tamura M, Kawafuchi J, Wakao T, Kumagai N. Cerebellar glioblastoma—report of a case and review of literature (author’s transl). Article in Japanese. Neurol Med Chir (Tokyo). 1979;19(6):517-522. doi:10.2176/nmc.19.517
19. Rosen J, Blau T, Grau SJ, Barbe MT, Fink GR, Galldiks N. Extracranial metastases of a cerebral glioblastoma: a case report and review of the literature. Case Rep Oncol. 2018;11(2):591-600. doi:10.1159/000492111
20. Shuto T, Fujino H, Inomori S, et al. Glioblastoma multiforme with liver metastasis—case report. Article in Japanese. No To Shinkei. 1995;47(8):772-777.
21. Matsuyama J, Mori T, Hori S, Nakano T, Yamada A. Gliosarcoma with multiple extracranial metastases. case report. Article in Japanese. Neurol Med Chir (Tokyo). 1989;29(10):938-943. doi:10.2176/nmc.29.938
22. Ogata A, Tashiro K, Abumiya T, et al. Glioblastoma multiforme with extracranial metastases without previous surgery: demonstration of extracranial metastases by peroxidase antiperoxidase staining and clinicopathological study. Article in Japanese. No To Shinkei. 1987;39(7):679-685.
23. Johnson RP, Guillan RA. Glioblastoma multiforme with remote extracranial metastases. J Kans Med Soc. 1974;75(5):169-172.
24. Anzil AP. Glioblastoma multiforme with extracranial metastases in the absence of previous craniotomy. case report. J Neurosurg. 1970;33(1):88-94. doi:10.3171/jns.1970.33.1.0088
25. Newton HB, Rosenblum MK, Walker RW. Extraneural metastases of infratentorial glioblastoma multiforme to the peritoneal cavity. Cancer. 1992;69(8):2149-2153. doi:10.1002/1097-0142(19920415)69:8<2149::aid-cncr2820690822>3.0.co;2-g
26. von Deimling A, von Ammon K, Schoenfeld D, Wiestler OD, Seizinger BR, Louis DN. Subsets of glioblastoma multiforme defined by molecular genetic analysis. Brain Pathol. 1993;3(1):19-26. doi:10.1111/j.1750-3639.1993.tb00721.x
27. Watanabe K, Tachibana O, Sata K, Yonekawa Y, Kleihues P, Ohgaki H. Overexpression of the EGF receptor and p53 mutations are mutually exclusive in the evolution of primary and secondary glioblastomas. Brain Pathol. 1996;6(3):217-223; discussion 23-24. doi:10.1111/j.1750-3639.1996.tb00848.x
28. Romero-Rojas AE, Diaz-Perez JA, Amaro D, Lozano-Castillo A, Chinchilla-Olaya SI. Glioblastoma metastasis to parotid gland and neck lymph nodes: fine-needle aspiration cytology with histopathologic correlation. Head Neck Pathol. 2013;7(4):409-415. doi:10.1007/s12105-013-0448-x
29. Fiorillo A, Maggi G, Martone A, et al. Shunt-related abdominal metastases in an infant with medulloblastoma: long-term remission by systemic chemotherapy and surgery. J Neuro-Oncol. 2001;52(3):273-276. doi:10.1023/a:1010687121450
30. Kumar R, Jain R, Tandon V. Thalamic glioblastoma with cerebrospinal fluid dissemination in the peritoneal cavity. Pediatr Neurosurg. 1999;31(5):242-245. doi:10.1159/000028870
31. Iliff JJ, Wang M, Liao Y, et al. A paravascular pathway facilitates CSF flow through the brain parenchyma and the clearance of interstitial solutes, including amyloid β. Sci Transl Med. 2012;4(147):147ra111. doi:10.1126/scitranslmed.3003748
32. Louveau A, Smirnov I, Keyes TJ, et al. Structural and functional features of central nervous system lymphatic vessels. Nature. 2015;523(7560):337-341. doi:10.1038/nature14432
33. Holdhoff M, Yovino SG, Boadu O, Grossman SA. Blood-based biomarkers for malignant gliomas. J Neurooncol. 2013;113(3):345-352. doi:10.1007/s11060-013-1144-0
34. Ramakrishna R, Rostomily R. Seed, soil, and beyond: the basic biology of brain metastasis. Surg Neurol Int. 2013;4(Suppl 4):S256-S264. doi:10.4103/2152-7806.111303
35. Bock Axelsen J, Lotem J, Sachs L, Domany E. Genes overexpressed in different human solid cancers exhibit different tissue-specific expression profiles. Proc Natl Acad Sci U S A. 2007;104(32):13122-13127. doi:10.1073/pnas.0705824104
36. Voldborg BR, Damstrup L, Spang-Thomsen M, Poulsen HS. Epidermal growth factor receptor (EGFR) and EGFR mutations, function and possible role in clinical trials. Ann Oncol. 1997;8(12):1197-1206. doi:10.1023/a:1008209720526
37. Müller C, Holtschmidt J, Auer M, et al. Hematogenous dissemination of glioblastoma multiforme. Sci Transl Med. 2014;6(247):247ra101. doi:10.1126/scitranslmed.3009095
38. Ray A, Manjila S, Hdeib AM, et al. Extracranial metastasis of gliobastoma: three illustrative cases and current review of the molecular pathology and management strategies. Mol Clin Oncol. 2015;3(3):479-486. doi:10.3892/mco.2015.494
39. Langley RR, Fidler IJ. The seed and soil hypothesis revisited—the role of tumor-stroma interactions in metastasis to different organs. Int J Cancer. 2011;128(11):2527-2535. doi:10.1002/ijc.26031
40. Val-Bernal F, Ruiz JC, Cotorruelo JG, Arias M. Glioblastoma multiforme of donor origin after renal transplantation: report of a case. Hum Pathol. 1993;24(11):1256-1259. doi:10.1016/0046-8177(93)90224-5
41. Detry O, Honoré P, Hans MF, Delbouille MH, Jacquet N, Meurisse M. Organ donors with primary central nervous system tumor. Transplantation. 2000;70(1):244-248; discussion 251-252.
42. Frank S, Müller J, Bonk C, Haroske G, Schackert HK, Schackert G. Transmission of glioblastoma multiforme through liver transplantation. Lancet. 1998;352(9121):31. doi:10.1016/S0140-6736(98)24027-X
43. Jimsheleishvili S, Alshareef AT, Papadimitriou K, et al. Extracranial glioblastoma in transplant recipients. J Cancer Res Clin Oncol. 2014;140(5):801-807. doi:10.1007/s00432-014-1625-3
44. Palmer CS, Ostrowski M, Balderson B, Christian N, Crowe SM. Glucose metabolism regulates T cell activation, differentiation, and functions. Front Immunol. 2015;6:1. doi:10.3389/fimmu.2015.00001
45. Young M, Reed KR. Organoids as a model for colorectal cancer. Curr Colorectal Cancer Rep. 2016;12(5):281-287. doi:10.1007/s11888-016-0335-4
46. Lancaster MA, Renner M, Martin C-A, et al. Cerebral organoids model human brain development and microcephaly. Nature. 2013;501(7467):373-379. doi:10.1038/nature12517
47. Bergmann S, Lawler SE, Qu Y, et al. Blood-brain-barrier organoids for investigating the permeability of CNS therapeutics. Nat Protoc. 2018;13(12):2827-2843. doi:10.1038/s41596-018-0066-x