Measure for measure: How to make practice benchmarks meaningful
MINNEAPOLIS-When it comes to taking stock of an oncology practice’s productivity, less is more. It benefits a practice to develop a few meaningful benchmarks rather than multiple overlapping, overwhelming, and meaningless measurements.
MINNEAPOLIS-When it comes to taking stock of an oncology practice’s productivity, less is more. It benefits a practice to develop a few meaningful benchmarks rather than multiple overlapping, overwhelming, and meaningless measurements.
At the 2009 National Oncology Economics Conference, two metrics experts shared their thoughts on how to make the most of productivity evaluation and, if necessary, intervention. Thomas P. Barr, MBA, of Oncology Metrics, and Teri U. Guidi, MBA, of Oncology Management Consulting Group, discussed the nuts and bolts of benchmarking for outpatient and hospital-based practices.
The conference was sponsored by the Association of Community Cancer Centers (ACCC).
Benchmarking: Not a blame game
“Be strategic,” said Mr. Barr, who is the COO of Oncology Metrics, based in Forth Worth, Tex. “Don’t measure something just because it is measurable.”
He defined a benchmark as a tool for comparing the practice or program with regional or national standards as well as with itself. The benchmark can help the practice evaluate its performance over time. He differentiated a benchmark from a gauge, which is used to monitor aspects of the practice over a shorter period. For example, revenue collected per month would be a gauge; the annual medical revenue divided by full-time equivalent (FTE) billing staff would be a benchmark.
However, benchmarks and gauges are similar in that they use objective measurable data elements, contain both a numerator and a denominator, and express the findings in quotients such as gross revenue per case or charges by type of service.
He encouraged oncology practices to develop benchmarks and use them to improve productivity and performance, to lower the cost of operations, and to provide more time for clinicians to spend on patient care. For example, a benchmark can help lower cost by allowing the practice to monitor and better control inventory. The practice can measure itself against its benchmarks annually or semiannually.
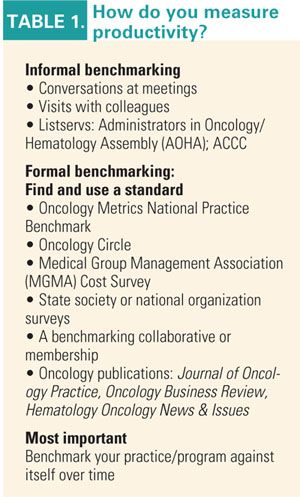
The practice can begin formal benchmarking by finding and using a standard, such as the Oncology Metrics National Practice Benchmark or those issued by oncology peer-reviewed journals. Whatever the practice’s choice, it is critical that the group measure itself against the benchmark over time.
Benchmarking “is not new or complex and isn’t about finding someone to blame,” Mr. Barr told Oncology News International. “Simple metrics and interventions can produce amazing results.” Stressing the importance of data from the practice itself, he added that “local solutions will evolve only in places where process measurements are in place to measure and support what works.”
Ms. Guidi agreed with Mr. Barr that the data need to be meaningful to the individual practice. She is the president and CEO of Oncology Management Consulting Group in Pipersville, Pa. “Most of the data are difficult for administrators to wrap their arms around and use for benchmarking.” For example, a statistic of 10 nurses per chair may not make it clear whether the statistic refers to FTE staff.
The right tools
Developing benchmarking systems based on web searches and random journal articles is no better than throwing darts, Ms. Guidi said. “Administrators need to find a resource that will give them what they need and not depend on web surfing and the random article. Find something that will give you what you need on a real-world basis” (see Table 1 on page 42).
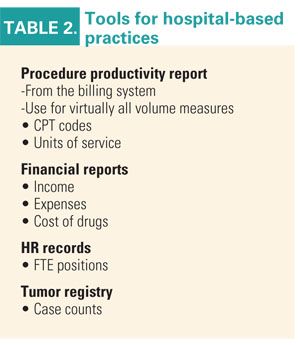
Some of the tools for developing meaningful benchmarks include procedure productivity reports (PPRs), financial reports, and human resources records, according to Ms. Guidi. The PPR will show the CPT codes for which the practice has billed in a specific period.
“Use your PPR to find the number of units billed and revenue collected for various procedures,” she said. These would include the practice’s total revenue and would typically consist of revenue from such services as evaluation and management, drug administration, and imaging.
Mr. Barr pointed out that the Oncology Metrics National Practice Benchmark groups revenue into eight categories. In addition to evaluation and management, drug administration, and imaging, the National Practice Benchmark categorizes revenue as coming from drug sales, laboratory services, radiation oncology, nonmedical revenue such as data sales and clinical research, and other revenue. It also analyzes the distribution of charges by the categories of infusions, pharmaceuticals, radiology, radiation therapy, and surgery.
Hospital challenges
Ms. Guidi noted that hospitals face a different set of circumstances than an outpatient facility. For instance, definitions for what constitutes a procedure or an FTE may differ in a hospital setting.

Importing data from hospital benchmarking reports can introduce confusion, Ms. Guidi said. For example, inpatient and outpatient records may be combined and the data may be general rather than specific to oncology. Also, the method by which the benchmark was created may not be obvious. “Ask for the most specific data you can” when working with a hospital, she said (see Table 2 on page 43).
She mentioned that The Oncology Business Institute has been founded as a way for hospital cancer centers to learn how to capture more oncology-specific data. Examples of meaningful benchmarks for an oncology practice include total gross revenue by type of cancer, department gross revenue per case, revenue for different years by category, and comparisons of different years’ number of new patients. The Oncology Circle’s benchmark analyzes the total revenue by FTE billing staff from one year to the next."