Is Neoadjuvant Chemotherapy in Ovarian Cancer an Excuse for Insufficient Surgery?
Surgical debulking of epithelial ovarian carcinoma has been a mainstay of therapy for more than 50 years-since the approach was first advocated by Meigs in 1934.[1] In 1968, Munnell[2] introduced the idea of the "maximum surgical effort”-essentially the removal of as much cancer as possible.
Surgical debulking of epithelial ovarian carcinoma has been a mainstay of therapy for more than 50 years-since the approach was first advocated by Meigs in 1934.[1] In 1968, Munnell[2] introduced the idea of the "maximum surgical effort”-essentially the removal of as much cancer as possible. Griffiths[3] subsequently attempted to quantitate this maximum effort and suggested that all cancerous areas should be reduced to 1.5 cm or less (the concept of "optimal cytoreduction”). The current consensus is that there should be no macroscopic residual tumor left after surgery, which implies the need for ultra-radical surgery.[4] A recent Cochrane analysis found one relevant nonrandomized study that analyzed data from 194 women recruited at one center.[5] The study investigators' best estimate was that the risk of death was about one-third lower for those women who had ultra-radical surgery than for those who underwent standard procedures. A recent meta-analysis of phase III studies performed by Arbeitsgemeinschaft Gynaekologische Onkologie Studiengruppe Ovarialkarzinom (AGO-Ovar) found that surgical outcome after initial debulking surgery had a tremendous impact on advanced ovarian cancer-specifically, on progression-free survival (PFS) and overall survival (OS).[6] These results fit well with a recently reported observation by the Gynecologic Oncology Group (GOG), to the effect that complete tumor resection has a significant impact, even in International Federation of Gynecology and Obstetrics (FIGO) stage IV disease.[7]
Traditionally, debulking surgery was performed prior to chemotherapy with the option for a second attempt at debulking at some time during the subsequent chemotherapy if the initial surgical debulking was suboptimal. The alternate approach is to administer neoadjuvant chemotherapy (NACT) followed by "interval debulking.” A meta-analysis of mainly nonrandomized trials suggested that the neoadjuvant approach was associated with a worse outcome, compared with primary debulking; however, a subsequent meta-analysis did not confirm this conclusion.[8,9] An obvious explanation for this discrepancy is that patients with more disease, poorer performance status, and so forth tend to be selected for a neoadjuvant approach, a priori biasing outcome.
Two randomized trials have been performed, and they settle the issue of the optimal timing of debulking.[10,11] Both studies were of women with newly diagnosed FIGO stage IIIC or IV disease and employed the same study design, using platinum-based chemotherapy-predominantly platin-taxane-and with the attempted maximal surgical debulking performed either before chemotherapy or after 3 cycles. In the European Organisation for Research and Treatment of Cancer (EORTC) study, 19% of the primary debulking patients underwent a second attempt at surgery, whereas only 90% of the interval debulking cohort went on to surgery, presumably due to early progression or deteriorated general conditions. The most striking result was that in contrast to all observations in primary surgery, increasing the complete resection rate from less than 20% to over 50% (after chemotherapy) did not improve prognosis. This is the genuine merit of the EORTC–National Cancer Institute of Canada (NCIC) study: namely, it shows that NACT is a dead-end when it comes to further improving outcomes with ovarian cancer surgery. This trial also clearly indicates that primary surgery is superior to a second intervention.
TABLE
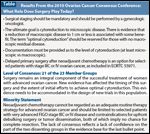
Results From the 2010 Ovarian Cancer Consensus Conference: What Role Does Surgery Play Today?
These findings were discussed at the recent Ovarian Cancer Consensus Conference (OCCC) in Vancouver organized by the Gynecological Cancer Inter-Group (GCIG).[12] GCIG currently comprises a cooperative of 23 clinical trial groups, including the most important European and American groups. The OCCC thoroughly discussed key subject areas and a set of 13 questions in a systematic manner, and the conference reached a unanimous consensus on all but one question. The one exception was the issue of the role of surgery in ovarian cancer treatment (Table). A minority (AGO Germany and AGO Austria) declined to support the statement that NACT is regarded as an adequate routine therapy strategy for advanced ovarian cancer.[13] The minority's opinion was that NACT should be limited to selected patients with very advanced FIGO stage IIIC or IV disease and contraindications for upfront debulking surgery or tumor dissemination, both of which imply no chance for complete resection. Several arguments have been raised by those who issued the minority statement. First, the primary objective of the EORTC/NCIC study was to prove non-inferiority of the neoadjuvant approach with regard to overall survival. Non-inferiority was defined as a hazard ratio (HR) < 1.25, indicating that a 25% higher mortality rate would be considered non-inferior-however, a rate increase of this magnitude is clinically meaningful. Also, the inclusion criteria for this intergroup study were rather unique and therefore substantially limit comparison with other studies and, even more importantly, with everyday clinical practice. The most important consequence of the study's unusual inclusion criteria is that they do not allow generalization of the study results to all patients with advanced ovarian cancer. The title of the write-up suggests that the study included patients with FIGO stage IIIC and IV ovarian cancer. However, this study population was further pre-selected by the requirement that patients have metastases of at least 2 cm outside the small pelvis; this inclusion criterion resulted in a study population with more advanced disease. Consequently, in this study the median tumor size for both arms was about 8 cm, and in 62 % of the patients the extra-pelvic metastases had a size of more than 10 cm. The nature of the patient selection is reflected in the low median survival times: a median of 29 months in the EORTC study, compared with other studies in advanced ovarian cancer (43 months in the AGO-Ovar-3 study, 45 months in the AGO-Ovar 5 study, 44 months in the AGO-Ovar 7 study, and 49 months in the AGO-Ovar 9 study).[6]
A wide variety of chemotherapy regimens were allowed in this EORTC-NCIC trial, and this might have contributed to the disappointing survival data. Moreover, only 72% and 85% of patients in the primary surgery and interventional debulking cohorts, respectively, received platinum and taxane–based chemotherapy. The surgical outcomes in this trial were rather heterogeneous. The observed heterogeneity makes it difficult to draw conclusions because of the potential bias with respect to the different surgical effort in different countries and inclusion bias concerning patients. The overall rate of complete resection in the whole primary surgery cohort was only 19%. Again, this is clearly lower than the rates in the other above-mentioned European studies, confirming either a selection bias or reduced surgical effort in some countries. The complete resection rate after NACT was 51%, and thus 32% higher than after primary surgery. The trial investigators stated that complete resection of all macroscopic disease was the strongest independent variable predicting OS. However, efforts to improve the rate of complete resection through better techniques and skills have only shown a benefit in the setting of primary surgery.
Currently available data do not justify changing existing statements about NACT. In contrast to improved upfront surgery, delayed surgery following NACT obviously has no potential to improve PFS or OS. Therefore, upfront surgery with a goal of macroscopic complete resection should remain the standard therapeutic approach in advanced ovarian cancer, and NACT should be limited to only very carefully selected patients with contraindications or inoperable tumor dissemination precluding successful upfront surgery. However, in many European countries no gynecologic oncology subspecialty has been developed. As a result, insufficiently qualified gynecologists or general surgeons are operating on ovarian cancer patients and may use the concept of neoadjuvant therapy as an excuse for poor surgical performance.
We and others have shown that department volume affects ovarian cancer survival.[14] An Austrian quality assurance program discovered a 20% difference in 5-year overall survival between patients treated at institutions that perform more than 24 surgeries per year and those treated at institutions that perform fewer than 24 surgeries per year. Multivariate analysis showed department size to be an independent prognostic factor (HR, 1.38 [95% confidence interval, 1.2-1.7]). Department size, however, may only be a surrogate for other factors, including physician training and specialization, and one of these factors might be the crucial variable.[15]
Junor et al[16] demonstrated that referral to a multidisciplinary team improves survival. The majority of women with ovarian cancer require a combination of surgery and chemotherapy as initial therapy and thus should not be managed by surgeons working in isolation. Earle et al[17] showed that women were more likely to receive postoperative chemotherapy when operated on by a gynecologic oncologist (79%) or a general gynecologist (76%) than when operated on by a general surgeon (62%). The UK National Institute for Clinical Excellence guidelines stipulate that when chemotherapy is used to treat ovarian cancer, the treatment should be supervised by a doctor who specializes in the treatment of ovarian cancer.[18] Unlike in the United States, health-policy organizations and insurance carriers in Europe, with the exception of some nations (eg, the United Kingdom), do not require this necessary development into greater specialization in the treatment of cancer patients. Formal training, such as that proposed by the European Society of Gynecologic Oncology, has not been implemented by the European Union or its member states, with a few exceptions. The gynecologic oncologist is a rare species and not present in Europe to the degree necessary. Promotion of NACT in ovarian cancer patients could be dangerous; it could further reduce the referral of patients to specialist centers and result in treatment by less experienced surgeons. NACT might therefore be furthering the harmful spread of oncologic dilettantism.
Financial Disclosure: The authors have no significant financial interest or other relationship with the manufacturers of any products or providers of any service mentioned in this article.
References:
REFERENCES
1. Meigs JV. Tumors of the pelvic organs. New York: Macmillan;1934.
2. Munnell EW. The charging prognosis and treatment in cancer of the ovary.
Am J Obstet Gynecol. 1968;100:790-5.
3. Griffiths CT. Surgical resection of tumor bulk in the primary treatment of
ovarian carcinoma. Nat Cancer Instit Monographs. 1975;42:101-5.
4. Chi DS, Eisenhauer EL, Zivanouc O, et al. Improved progression-free and
overall survival in advanced ovarian cancer as a result of a change in surgical
paradigm. Gynecol Oncol. 2009;114:26-31.
5. Ang C, Chan KKL, Bryant A, et al. Ultra-radical (extensive) surgery versus standard surgery for the primary cytoreduction of advanced epithelial ovarian cancer. Cochrane Database Syst Rev. 2011;4:CD007697.
6. du Bois A, Reuss A, Pujade-Lauraine E, et al. Role of surgical outcome as prognostic factor in advanced epithelial ovarian cancer: a combined exploratory analysis of 3 prospectively randomized phase 3 multicenter trials. Cancer. 2009;115:1234-44.
7. Crawford SC, Vasey PA, Paul J, et al. Does aggressive surgery only benefit patients with less advanced ovarian cancer? Results from an international comparison within the SCOTROC-1 Trial. J Clin Oncol. 2005;23:8802-11.
8. Bristow RE, Chi DS. Platinum-based neoadjuvant chemotherapy and interval surgical cytoreduction for advanced ovarian cancer: a meta-analysis. Gynecol Oncol. 2006;103:1070-6.
9. Kang S, Nam BH. Does neoadjuvant chemotherapy increase optimal cytoreduction rate in advanced ovarian cancer? Meta-analysis of 21 studies.
Ann Surg Oncol. 2009;16:2315-20.
10. Vergote I, Trope CG, Amant F, et al. Neoadjuvant chemotherapy or primary surgery in stage IIIC or IV ovarian cancer. N Engl J Med. 2010;363:10.
11. Kumar L, Hariprasad R, Kumar S, et al. Upfront surgery vs neoadjuvant
chemotherapy in advanced epithelial ovarian carcinoma (EOC): a randomized study. IGCS 13. Prague 2010 (A824).
12. Stuart GC, Kitchener H, Bacon M, et al; >participants of Fourth Ovarian Cancer Consensus Conference (OCCC). 2010 Gynecologic Cancer InterGroup (GCIG) consensus statement on clinical trials in ovarian cancer: report from the Fourth Ovarian Cancer Consensus Conference. Int J Gynecol Cancer. 2011;4:750-5.
13. du Bois A, Marth C, Pfisterer J, et al. Neoadjuvant chemotherapy cannot be regarded as adequate routine therapy strategy of advanced ovarian cancer. Int J Gynecol Cancer. 2011;6:1165-8.
14. Marth C, Hiebl S, Oberaigner W, et al. Influence of department volume on survival for ovarian cancer: results from a prospective quality assurance program of the Austrian Association for Gynecologic Oncology. Int J Gynecol Cancer. 2009;19:94-102.
15. du Bois A, Rochon J, Pfisterer J, Hoskins WJ. Variations in institutional infrastructure, physician specialization and experience, and outcome in ovarian cancer: A systematic review. Gynecol Oncol. 2009;112:422-36.
16. Junor EJ, Hole DJ, Gillis CR. Management of ovarian cancer: referral to a multidisciplinary team matters. Br J Cancer. 1994;70:363-70.
17. Earle CC, Schrag D, Neville BA, et al. Effect of surgeon specialty on processes of care and outcomes for ovarian cancer patients. J Natl Cancer Inst. 2006;98:172-80.
18. Review of the clinical effectiveness and cost effectiveness of paclitaxel for ovarian cancer. NICE Guideline Review No. 55, 2003. Available from: http://www.nice.org.uk.