Tools for Measuring and Improving the Quality of Oncology Care: The Quality Oncology Practice Initiative (QOPI®) and the QOPI Certification Program
The American Society of Clinical Oncology (ASCO) Quality Oncology Practice Initiative (QOPI®) is a voluntary program designed to assess and improve processes of care in oncology practices.
The American Society of Clinical Oncology (ASCO) Quality Oncology Practice Initiative (QOPI®) is a voluntary program designed to assess and improve processes of care in oncology practices. QOPI measures are evidenced-based and consensus-based measures that are derived from published research studies, peer-reviewed guidelines, and expert consensus. The mission of QOPI is to provide a means by which oncology practices can continually examine the care they provide, to ensure that each patient receives the best care possible. The framework of QOPI promotes a system that is:

Michael Neuss, MD
Chief Medical Officer
Vanderbilt-Ingram Cancer Center
• Designed and run by oncology practitioners.
• Relevant and valuable to all oncology practices.
• Transparent.
• Deliverable anywhere.
• Capable of measuring progress with peer comparison.
• Simple and inexpensive to implement and use.
• Dynamic and modifiable and current.
• Focused on improvement, not research.
History
QOPI began as a pilot program in 2002, with 23 practices abstracting 6,000 charts over 4 years to collect data on 37 measures.[1] In 2006, the program was made available at no charge to ASCO members in the United States; however, practices bear the cost of data collection and submission-that is, the practices collect and submit data to an ASCO system, and ASCO provides support through data collection and analysis. Over time, the number of QOPI measures has increased, and they are now arranged into modules of required core measures; disease-specific groupings for specific types of cancer; and other groupings that include symptom/toxicity management, and end-of-life care. In 2008, 193 practices abstracted more than 18,000 charts to collect data on 81 measures.[2] QOPI registration had grown to more than 700 practices by 2010, with practices located in all 50 states, Puerto Rico, and Guam. More than a quarter of registered practices (260) submitted data on 26,651 patients in the fall 2010 data collection period.[3]
How QOPI Works
ASCO provides training and a manual to guide practice staff in conducting retrospective chart reviews up to twice per year. In the fall 2010 data collection period, a limited dataset for 107 QOPI measures was available for abstraction and entry into QOPI's secure Web-based application. At the close of data collection, practice reports are provided that compare practice-specific results to aggregate data of the entire set of results and also with data from similar-type practices (eg, academic or independent/private). Reports are available within one month of the close of the data submission period.
Current QOPI measures (and associated modules) address the following:
Core measures
• Documentation of care, including confirmation of cancer diagnosis and stage.
• Chemotherapy planning and administration.
• Pain assessment and control.
Disease-specific modules
• Breast cancer management.
• Colorectal cancer management.
• Non-Hodgkin lymphoma management.
• Non–small-cell lung cancer management.
Domain-specific modules
• Care at end of life.
• Symptom and toxicity management.
As noted, examples of core documentation of care measures include having the pathology report available in the patient's medical record, documenting a treatment plan, obtaining consent for chemotherapy, and recognizing and addressing pain. Examples of measures for disease-specific modules include assessment of appropriate pathologic exams, stage-specific recommendations, and achievement of administration of antineoplastic therapy in accordance with recognized guidelines. Examples of symptom and toxicity management measures include use of antiemetics and growth factors in accordance with guidelines, and fertility preservation and counseling.
What Early QOPI Data Showed
Early data abstraction (spring 2007) revealed that while 90% of patients received recommended care for breast and colon cancer management measures, fewer than half of patients received care at the end of life that was concordant with the measures assessed (eg, hospice enrollment, palliative care referral, assessment of pain and dyspnea, etc). Results have shown that performance on certain measures varies widely among participating practices. For example, while documentation of staging within one month of the initial practice visit was done for 83% of patients, 17% of charts did not provide stage in that time period, and in one practice, 60% of charts did not provide documentation of staging.
There is no preconceived expectation in QOPI that all measures should be achievable in 100% of patients. Truly ideal practice, which accounts for patient consent and variability, may well provide perfect care with less than 100% concordance with measures. Some patients (for example, a person with blastic bone lesions and a prostate specific antigen level of 10,000 ng/mL, or an Alzheimer's patient with a rock hard breast mass, hepatomegaly, and multiple enhancing lesions on brain imaging) may not require pathologic confirmation of malignancy.
Practices can benchmark their score to that of their peers, which is extremely valuable to smaller remote practices that have no other means of assessing the care they provide. Low adherence rates for certain measures likely occur for a variety of reasons, such as slow diffusion of knowledge, disagreement with guideline recommendations, or patient factors.
Trends in More Recent QOPI Data
Review of QOPI aggregate data since 2007 offers insights into secular trends in care. Performance by QOPI practices as a group remained stable on a majority of the measures, decreased on some, and improved on others (Figure).[4] There are exceptions to the trends that are apparent in the data. For example, there is steep improvement in performance on aprepitant (Emend) administration to patients receiving highly emetogenic chemotherapy, although whether this correlated with practice learning curves or the availability of an intravenous agent is unclear. Several gaps in care identified in the QOPI group data include discussion of infertility risk and fertility preservation prior to receipt of chemotherapy, the counseling of smokers about smoking cessation, and the screening of patients with non-Hodgkin lymphoma for hepatitis B prior to initiation of rituximab (Rituxan). In addition, improvement is needed in enrolling patients in hospice, and in completing a treatment plan/summary and providing the patient with a copy. The need for practice improvement in these areas has been consistent over four years of measurement, and underscores the difference between quality measurement and quality improvement.
From Quality Measurement to Quality Improvement
Potential drivers for quality improvement include public reporting, pay for performance, increased reimbursements, and collaborative improvement networks. Of course, practitioners' desire to provide their patients with the best possible care is also critically important.
FIGURE
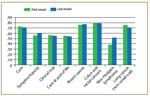
Cancer Mean Quality Scores by Domain for Initial and Most Recent (Last) Round of Participation
Collaborative improvement networks (CINs) have begun to integrate QOPI as a tool for identifying areas to target for improvements; they use the strength of the collaborative to drive change and improvement. These “collaborative improvement networks” received their name because they share the following characteristics:
• Willingness to share information, ideas, and best practices.
• Focus on the identification of gaps in care and improvement of these gaps.
• Willingness to engage experts in quality improvement.
• Focus on improvement that is based on measurable targets, data collection, and tests of change.
• Willingness to use a structured process for the exchange of ideas and experiences, and for advancing improvement.
• Ability to commit resources to enable collaborative efforts.
ASCO recently brought together six CINs to share how they use QOPI participation and reports to identify gaps in care and to engage practices in quality improvement activities. These ranged from the 6–independent practice network facilitated by the Northern New England Oncology Society, to the corporate 135-site Texas Oncology Practice. Each CIN discussed its history and funding, mission, membership selection, program design and oversight, and the role of QOPI certification in its network.
The six groups and their representatives included:
• Michigan Oncology Quality Consortium (MOQC); Jane Martin, MHSA, and Doug Blayney, MD
• NCI Community Cancer Centers Program (NCCCP); Donna Bryant
• Northern New England Oncology Society (NNECOS); Andrew Hertler, MD, FACP
• Texas Oncology; Jon Cox, DO, Deidre Watson, CTR, and Gay Lindsey, RN, NSN, OCN
• University of Pittsburgh Medical Center; Peter Ellis, MD, and Kyle Bird
In addition, three financial sponsors of these networks were invited to discuss reasons for their support of the network, how they plan to evaluate effectiveness, and their long-term vision for sponsorship of the network. Sponsors and their representatives were:
• Blue Cross Blue Shield of Michigan (BCBSM); Tom Ruane, MD
• National Cancer Institute; Steve Clauser, PhD, and Kate Castro, RN, MS, AOCN
• Advocate Health Group; Donna Siemons, RN, MBA
All participants used QOPI data collection to reveal a number of areas upon which to focus improvement efforts. The CINs used various approaches to achieve quality improvement within the collaborative; these included focusing on documentation, targeting specific measures for root-cause analysis and intervention, and encouraging practices to apply for QOPI certification by linking QOPI-certified practices with practices working toward certification.
Sponsors support QOPI for many reasons, including that they find comparative norms help physicians by increasing awareness through measurement of current performance. Most physicians believe they're doing everything the right way. Performance data can be a powerful tool for demonstrating that such a perception differs from reality, and for identifying opportunities for improvement. Facilitating this focus on quality measurement and improvement has increased awareness of evidence-based medicine, and supports physician needs.
The QOPI Certification Program
In addition to QOPI participation, oncology practices now also have the opportunity to pursue QOPI certification. Certification is an objective, measurable process that confirms that a practice meets national quality and safety standards. ASCO created the QOPI Certification Program (QCP) to enable practices to benchmark their performance against QOPI performance thresholds and to implement improved systems. Practices must meet 17 chemotherapy administration safety standards based on those jointly developed by ASCO and the Oncology Nursing Society[4] and must accurately abstract data from patients' medical records. In addition, some practices are randomly selected for an on-site review.[5] Since 2010, when oncology practice certification was first awarded, the QCP has certified 90 US practices.[6]
To date, 122 practices have applied for QOPI certification. About half of the applicants are small-sized practices comprised of fewer than seven oncologists. Practices submit materials, such as de-identified chart documentation and copies of the practice's policies and procedures, for review by QCP staff and steering group reviewers. The materials are reviewed to determine whether or not the 17 chemotherapy administration safety standards have been met. Upon initial review, 84.6% of the practices seeking certification did not meet standard 1, which requires that practices have policies that state the qualifications of staff members who write chemotherapy orders, prepare chemotherapy, and administer chemotherapy in the practice. Practices not meeting a standard are given guidance on how the standard can be met, and can revise and then resubmit the required documentation. In some instances, evidence of staff education about a policy or process is required, and practices submit documentation that the needed education has been provided. The standards most commonly not met in practice (as observed during the on-site reviews) are the standards that require practices to have policies and procedures that describe the processes for 1) obtaining patients' consent to receive chemotherapy; 2) preparing, storing, and delivering intrathecal chemotherapy; 3) managing extravasations; and 4) assessing patients' medications.
Future Directions
The QOPI and QCP programs will continue to evolve, and plans include developing outcome measures, transmitting data via electronic health records, increasing the number of QOPI-based collaborative improvement networks, and using prospective registries to collect data.[7] A prospective breast cancer registry was piloted and found to be feasible by ASCO; lessons learned from the pilot will contribute to future developments.[8] In addition, new cohorts of practices will be assessed, and additional long-term data will be collected from practices that have participated in QOPI since its inception. A long-term goal is to determine whether participation in QOPI and QCP certification will translate into higher-value oncology care with reduced costs and improved patient outcomes.[3]
References:
REFERENCES
1.Jacobson JO, Neuss MN, McNiff KK, et al. Improvement in oncology practice performance through voluntary participation in the Quality Oncology Practice Initiative. J Clin Oncol. 2008;26:1893-8.
2. Neuss MN, Jacobson JO, McNiff KK, et al. Evolution and elements of the Quality Oncology Practice Initiative measure set. Cancer Control. 2009;16:312-7.
3. Campion FX, Larson LR, Kadlubek P, et al. Advancing performance measurement in oncology. Am J Manag Care. 2011;17(5 suppl):SP32-6.
4.Jacobson JO, Polovich M, McNiff KK, et al. American Society of Clinical Oncology/Oncology Nursing Society chemotherapy administration safety standards. Oncol Nurs Forum. 2009;36:651-8.
5.McNiff KK, Bonelli KR, Jacobson JO. Quality Oncology Practice Initiative certification program: overview, measure scoring methodology, and site assessment standards. J Oncol Pract. 2009;5:270-6.
6.Certification. Available at http://qopi.asco.org/certification. Accessed August 5, 2011.
7.Gilmore T, Neuss MN, Kadlubek P, et al. Quality Oncology Practice Initiative (QOPI) certification applicants and outcomes. J Clin Oncol. 2011;29(suppl): abstract e16599.
8.Partridge AH, Norris VW, Blinder VS, et al. The ASCO Breast Cancer Registry pilot: implementation of a multisite community practice registry and treatment plan/summary program. J Clin Oncol. 2011;29(suppl): abstract e 6101).