New Delivery, Monitoring Methods for Taxol in Brain Tumors
SAN FRANCISCO-Israeli investigators have developed a new method for enhancing paclitaxel (Taxol) delivery to recurrent brain tumors and are using diffusion-weighted magnetic resonance imaging (MRI) to monitor for response.
SAN FRANCISCOIsraeli investigators have developed a new method for enhancing paclitaxel (Taxol) delivery to recurrent brain tumors and are using diffusion-weighted magnetic resonance imaging (MRI) to monitor for response.
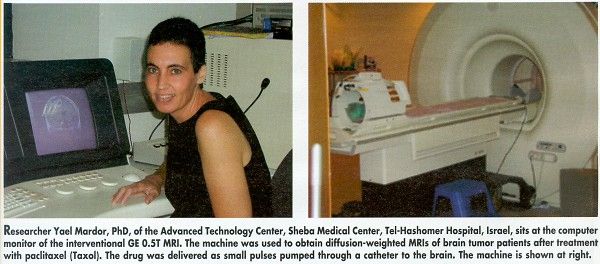
Physicist Yael Mardor, PhD, presented initial phase I/II trial results at the 37th Annual Meeting of the American Society of Clinical Oncology (ASCO abstract 217) on behalf of neurosurgeon Zvi Ram, MD, and other colleagues at Sheba Medical Center, Tel-Hashomer Hospital, Israel.
The technique uses convection to overcome the blood-brain barrier. Small pulses of paclitaxel are pumped through a catheter to the brain for several days, inducing a pressure gradient within the tumor.
By using diffusion-weighed MRIs sensitive to the speed of water molecules, the investigators were able to see immediate changes in images taken before, during, and after treatment. "The idea is that we filter out the signals from the fast water molecules and look only at the signals coming from slow water molecules," Dr. Mardor said. "This kind of image gives specific tissue characterization that is not obtained by conventional MRI."
The ASCO poster documented paclitaxel’s effect in the first three glioma patients treated with the new technique. In an MRI taken shortly after a patient received paclitaxel through a catheter, a bright spot appeared in the brain, consistent with brain swelling. In subsequent images, the spot was seen to spread. Dr. Mardor said that the spot shows the slowing down of water molecules as a result of treatment.
"Several days after the treatment began, we saw within the bright spot an appearance of a dark spot. The dark spot means fast water flow, which we think is correlated with later necrosis of this tumor," she told ONI. "And if you look at the conventional MRI, 2 weeks post-therapy, you see that the therapy actually burned a hole in the treated area, so this patient did respond to the therapy."
Dr. Ram’s technique for infusing paclitaxel enables patients to receive very high concentrations of the drug over very high volumes of the brain, Dr. Mardor said. The hope is that it will also be effective in other brain tumors that do not respond to chemotherapy because of the blood-brain barrier.
The investigators noted that while significant changes were documented in all three glioma patients, the dark area appeared at different times after treatment began, suggesting different response rates among the patients. The diffusion-weighted MRIs were correlated with clinical progress and diagnostic MR scans.
"We presume diffusion-weighed MRI it will also be useful for monitoring other types of radical treatment," Dr. Mardor said. In a separate presentation (abstract 201), she reported that it was used as a noninvasive diagnostic tool in 11 patients with various brain malignancies. These patients were treated with radiation therapy (5 patients), chemotherapy (2 patients), and radiosurgery (4 patients). Several patterns of response have been observed, and the study is ongoing, she said.