Novel Biologic Agents for Non-Hodgkin Lymphoma and Chronic Lymphocytic Leukemia-Part 2: Adoptive Cellular Immunotherapy, Small-Molecule Inhibitors, and Immunomodulation
In this review we discuss adoptive cellular immunotherapies, small-molecule inhibitors, and immunomodulatory agents. We also mention other novel therapies on the horizon.
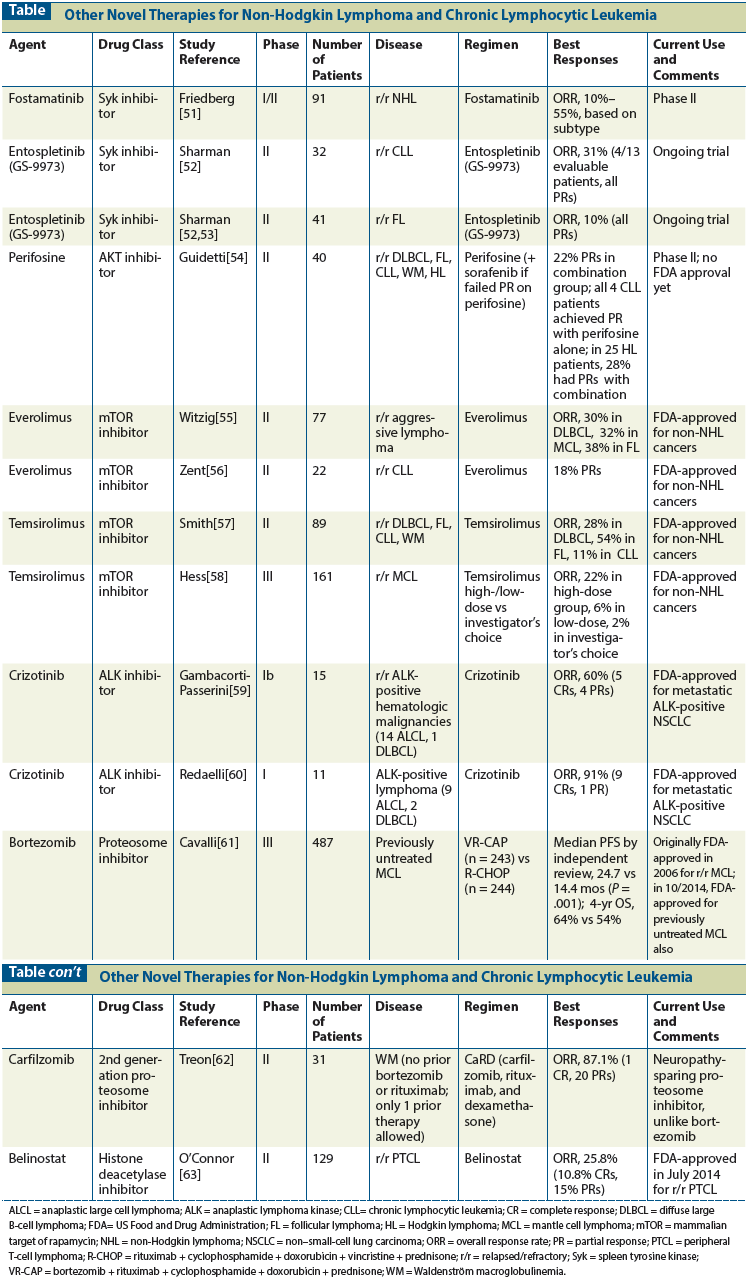
Table: Other Novel Therapies for Non-Hodgkin Lymphoma and Chronic Lymphocytic Leukemia
Globally, the incidence of non-Hodgkin lymphoma is increasing. Aggressive non-Hodgkin lymphomas like diffuse large B-cell lymphoma are treated with curative intent in the frontline setting, but indolent diseases like chronic lymphocytic leukemia/small lymphocytic lymphoma are not considered to be curable in general. Additionally, relapsed/refractory non-Hodgkin lymphomas have a poor overall outcome, with treatment response durations often decreasing with each relapse. Novel therapies are sought to improve outcomes in this patient population. In a two-part review, we describe the promising new biologic therapies that have emerged over the last 5 years, some approved by the US Food and Drug Administration and others undergoing active investigation. In Part 1, we discussed monoclonal antibodies. Here, in Part 2, we discuss adoptive cellular immunotherapies, small-molecule inhibitors, and immunomodulatory agents. We also mention other novel therapies on the horizon.
Background
Over the last several decades, the incidence of non-Hodgkin lymphoma has been increasing.[1] It is the fifth most common cancer in the United States[2] and includes a wide spectrum of lymphoid malignancies; these range from indolent diseases (such as chronic lymphocytic leukemia/small lymphocytic lymphoma, follicular lymphoma, marginal-zone lymphoma, and cutaneous T-cell lymphoma) to aggressive diseases (such as diffuse large B-cell lymphoma, mantle cell lymphoma, and peripheral T-cell lymphoma). There have been numerous therapeutic advances in the treatment of non-Hodgkin lymphoma in recent years, including new chemotherapy regimens, monoclonal antibodies, radioimmunotherapy, and targeted therapy with small-molecule inhibitors of pathways of cell survival and growth. However, patients with relapsed/refractory non-Hodgkin lymphomas still do poorly in general, and the search for novel therapeutic modalities that will yield improved and durable outcomes in such patients is ongoing.
In this two-part review, we discuss biologic therapies classified by their targets and mechanisms of action that have received US Food and Drug Administration (FDA) approval for the treatment of non-Hodgkin lymphoma in the last 5 years, as well as promising agents that are more advanced in development. In Part 1, we focused on monoclonal antibodies, while here in Part 2 we primarily review adoptive cellular immunotherapies, small-molecule inhibitors, and immunomodulatory agents.
Adoptive Cellular Immunotherapy
Chimeric antigen receptor (CAR) T cells
An attractive, powerful way to harness the cytotoxic potential of T cells in the treatment of B-cell non-Hodgkin lymphoma/chronic lymphocytic leukemia is to use genetically engineered autologous T cells that express CARs specifically targeting CD19. A CAR is a genetically engineered fusion protein comprising an antigen-recognizing extracellular moiety to redirect antigen specificity (eg, CD19), a hinge region, and a transmembrane domain linked to an intracellular CD3-zeta T-cell signaling domain (CD3ζ). In newer generations of CAR design, including the one we are using at City of Hope, costimulatory domains like CD28 and/or 4-1BB have been added to the signaling domain to enhance T-cell function.[3]
Peripheral blood mononuclear cells are first collected from patients by a single leukapheresis. T cells are then isolated in the laboratory, after which process the CAR is introduced by lentiviral transduction. Transduced cells are then expanded ex vivo, cryopreserved, and adoptively reinfused into patients after a lymphodepleting chemotherapy regimen (like cyclophosphamide, fludarabine, or a combination of both) is administered a few days before CAR T-cell infusion. Subsequent in vivo expansion and activation of the CAR T cells is then expected to lead to antitumor responses that are durable, as these modified T cells could survive in patients for a long duration, potentially indefinitely. Challenges in the development of this therapeutic modality over the decades have included the unreliable persistence of CAR T cells and the development of prolonged hypogammaglobulinemia due to B-cell aplasia in some patients.
The first major reports using CD19-CAR T cells in hematologic malignancies were of patients with chronic lymphocytic leukemia.[4,5] The University of Pennsylvania (UPenn) utilized a second-generation CAR design containing the CD3ζ/4-1BB signaling domain to make their CD19-specific CAR T-cell product (CTL019). The most recent update reported treatment of 14 patients with relapsed/refractory chronic lymphocytic leukemia.[6] Median age was 67 years (range, 51–78 years) and median number of prior therapies was four (range, 1–10). Six patients had p53 mutation and all had active disease at the time of CTL019 infusion after lymphodepleting chemotherapy. A median of 1.4 × 108 (range, 0.14–5.9 × 108) CTL019 cells were infused over days 0, 1, and 2. No infusional toxicities higher than grade 2 were observed, although six patients developed fever within the first 24 hours after infusion and were not given additional CTL019. Median follow-up was 9.4 months. The overall response rate (ORR) was 57% (21% complete responses [CRs], 36% partial responses [PRs]). Two of the PR patients progressed 4 months after CTL019 infusion, but there were no relapses among the CR patients. There did not appear to be any obvious association between cell dose and responses. All responding patients did have some degree of reversible cytokine release syndrome (CRS) corresponding to peak T-cell expansion and elevation of various cytokine levels, including interleukin 6 (IL-6) and interferon gamma. Manifestations of CRS were fever, nausea, anorexia, myalgias, hypotension, and hypoxia. Five patients required intervention, with one patient receiving corticosteroids alone, one receiving the anti–IL-6-receptor antagonist tocilizumab alone, and three receiving both corticosteroids and tocilizumab. These interventions did not appear to interfere with the persistence of CTL019 cells on subsequent serial evaluations. All patients have sustained B-cell aplasia but no unusual infectious complications.
Currently, to define an optimal CTL019 cell dose in patients with relapsed/refractory chronic lymphocytic leukemia, the UPenn group is performing a randomized phase II study of two doses (5 × 108 or 5 × 107 CTL019 cells) given as a single dose 3 to 5 days after lymphodepleting chemotherapy.[7] So far, 27 patients have been enrolled and 10 have been treated (4 at the higher dose and 6 at the lower dose). Median age was 63 years (range, 59–76 years), five patients had p53 mutation, and all patients had active disease at the time of CTL019 infusion. No significant infusional toxicities were observed. Median follow-up was 3 months. The ORR was 40% (2 CRs, 2 PRs), and none of the responders progressed. Seven patients had CRS, with two requiring tocilizumab. No association has been observed yet between dose and response or dose and toxicities. Two responders had the higher cell dose and two had the lower dose. CTL019 in vivo cell expansion and persistence were observed in all responding patients serially.
Anti-CD19 CAR T-cell therapy has proven promising in B-cell acute lymphocytic leukemia as well.[8,9] A recent phase I/II study reported CTL019 therapy in 30 children (n = 25) and adults (n = 5) with relapsed/refractory acute lymphocytic leukemia.[10] The median age in the pediatric group was 11 years (range, 5–22 years), and in the adult group it was 47 years (range, 26–60 years). A total of 27 patients (90%) achieved CR, including 2 who had relapsed after blinatumomab therapy and 15 who had undergone prior allogeneic hematopoietic stem cell transplant (HSCT). At 6 months, the recurrence-free survival rate was 67%, and overall survival (OS) was 78%. All patients experienced CRS, which was severe in 27% (treated effectively with tocilizumab). Neurologic toxicities were seen in 13 patients and were self-limiting with supportive measures. CTL019 cells were detected in the spinal fluid of 17 of 19 patients who had evaluable specimens. Prolonged persistence of CTL019 cells and B-cell aplasia was seen for up to 2 years in this study and for more than 3 years in the study of chronic lymphocytic leukemia. In July 2014, the FDA gave CTL019 a breakthrough designation for the treatment of relapsed/refractory pediatric and adult acute lymphocytic leukemia. The group at the National Cancer Institute (NCI) have also seen promising results with their CAR T-cell therapy in patients with relapsed/refractory non-Hodgkin lymphoma/chronic lymphocytic leukemia,[11-13] especially in patients who received higher-intensity conditioning/lymphodepletion regimens, although there also appeared to have been more toxicity in those patients. Among a total of 30 treated patients thus far, they have reported responses (CR + PR) in 22 of 27 evaluable patients. At the time of the latest update, 10 patients continued to have a CR 1 to 37 months after treatment.
At this time, a handful of other major cancer centers across the country, including ours, have ongoing CAR T-cell therapy clinical trials in B-cell acute lymphocytic leukemia, B-cell non-Hodgkin lymphoma, and B-cell chronic lymphocytic leukemia/small lymphocytic lymphoma. Additionally, attempts are being made to evaluate this therapy in non–CD19-related malignancies using different targets. Some pharmaceutical companies are also beginning to initiate clinical trials in collaboration with major medical centers in order to assist with more widespread commercialization of this therapeutic modality.
Small-Molecule Inhibitors
Bruton tyrosine kinase (BTK) inhibitors
B-cell receptor signaling in normal and malignant B-cells is important for cell proliferation and survival. In fact, BCR is implicated in the pathogenesis of some B-cell non-Hodgkin lymphomas, such as diffuse large B-cell lymphoma, mantle cell lymphoma, follicular lymphoma, and chronic lymphocytic leukemia/small lymphocytic lymphoma. Bruton tyrosine kinase is a member of the Tec kinase family and is a signaling small molecule early in the BCR signaling cascade, along with Syk and phosphoinositide 3-kinase delta (PI3Kδ).
Ibrutinib. This is a first-in-class, oral, selective, potent, irreversible inhibitor of BTK that covalently binds to, and modifies, the cysteine-481 residue near the active site of BTK.[14] In vitro, this inhibition proved to be cytotoxic in some non-Hodgkin lymphoma models and primary chronic lymphocytic leukemia cells.[14,15] An initial phase I study of patients with relapsed/refractory B-cell non-Hodgkin lymphoma or chronic lymphocytic leukemia using escalating doses of ibrutinib enrolled 56 patients treated over seven cohorts for a median of 5 cycles.[16] The median age was 65 years (range, 41–82 years) and patients received a median of 3 prior lines of therapy (range, 1–10). A total of 29% of patients had follicular lymphoma, 29% had chronic lymphocytic leukemia/small lymphocytic lymphoma, 16% had mantle cell lymphoma, 13% had diffuse large B-cell lymphoma, 7% had marginal zone lymphoma, and 7% had Waldenström macroglobulinemia. The maximum tolerated dose was not reached, and only two dose-limiting toxicities were reported: one grade 3 allergic hypersensitivity and one grade 2 transient neutropenia persisting for more than 7 days. Most adverse events (AEs) were grade 1 or 2 in severity and self-limited. Grade 3 and 4 events were infrequent and independent of dose. Grade 3/4 hematologic toxicities included neutropenia (12.5%), thrombocytopenia (7.2%), and anemia (7.1%). No cumulative hematologic or nonhematologic toxicities were observed in patients who received prolonged dosing of ibrutinib. The objective response rate in the 50 evaluable patients was 60%, including 16% CRs. In this study, 7 of 9 patients with mantle cell lymphoma (3 CRs), 11 of 16 patients with chronic lymphocytic leukemia/small lymphocytic lymphoma (2 CRs), 6 of 16 patients with follicular lymphoma (3 CRs), 2 of 7 patients with diffuse large B-cell lymphoma, 3 of 4 patients with Waldenström macroglobulinemia, and 1 of 4 patients with marginal zone lymphoma responded. Median progression-free survival (PFS) was 13.6 months. Once-daily dosing with 560 mg orally was recommended based on these results, although ultimately the 420-mg daily dose moved forward in chronic lymphocytic leukemia, while the 560-mg dose moved forward in non-Hodgkin lymphoma.
The 11 responding patients with chronic lymphocytic leukemia in this trial showed a rapid decrease in lymphadenopathy, with an increase in absolute lymphocytosis in the first cycle of therapy. This response suggests migration of lymphocytes from the lymph nodes into the peripheral blood, likely as a result of interference with migration and adhesion of leukemia/lymphoma cells residing in lymphatic tissues. On an intermittent dosing schedule, this lymphocytosis reversed rapidly during the off-ibrutinib period; again, this was likely due to increased tissue homing, but it recurred once ibrutinib was restarted. This lymphocytosis appears to be asymptomatic and transient, and it resolves in most patients over the first few months of therapy. It is a phenomenon that is also being observed with other kinase inhibitors, like the PI3Kδ inhibitor idelalisib,[17] and has led to revision of the chronic lymphocytic leukemia response criteria to account for this type of treatment-related redistribution lymphocytosis.[18]
In a phase II, open label, multicenter clinical trial in patients with relapsed/refractory mantle cell lymphoma, 111 patients were treated with ibrutinib at 560 mg/d orally.[19] There were two groups of patients: those who had received ≥ 2 cycles of bortezomib therapy previously and those who had received < 2 cycles or no prior bortezomib therapy. Median age of patients was 68 years (range, 40–84 years) and patients received a median of 3 prior lines of therapy (range, 1–5). The most common treatment-related AEs were mild-moderate diarrhea, fatigue, and nausea. Grade 3 or higher hematologic AEs were infrequent and included neutropenia (16%), thrombocytopenia (11%), and anemia (10%). Five patients had bleeding events, four with subdural hematomas as a result of head trauma and/or falls. All four of these patients were also on aspirin or warfarin. The ORR was 68%, with 21% CRs and 47% PRs. Prior bortezomib therapy had no effect on ORR. Median duration of response was 17.5 months, the estimated median PFS was 13.9 months, and median OS was not reached. The estimated OS was 58% at 18 months.
In summary, ibrutinib was found to show durable efficacy in these patients. Warfarin is contraindicated in future studies, but other blood thinners are allowed. Data from larger, randomized studies can help determine whether or not ibrutinib leads to an increased risk of bleeding. In the meantime, the recommendation is to hold ibrutinib 7 days before and 7 days after any major procedure, or 3 days before and 3 days after any minor procedure, to limit the risk of bleeding. Ibrutinib is metabolized primarily in the liver via the p450 cytochrome system; therefore, it is important to be aware of, and avoid, potential drug-drug interactions, especially where there is concurrent treatment with CYP3A/4 inducers/inhibitors. It must be kept in mind that some foods (eg, grapefruit) and certain supplements (eg, St. John’s wort) can also interact adversely with ibrutinib. Based on the data from this study, in November 2013 the FDA granted accelerated approval to ibrutinib for the treatment of patients with mantle cell lymphoma who have received at least one prior therapy. At the 2014 annual meeting of the American Society of Hematology, the results were updated. The median duration of response was 17.5 months. At an estimated median follow-up of 26.7 months, the median PFS for all treated patients was 13 months, and median OS was 22.5 months.
Two phase Ib/II trials showed ibrutinib yielded an impressive clinical benefit in chronic lymphocytic leukemia/small lymphocytic lymphoma patients.[20,21]
Byrd et al, in an open-label, multicenter study, enrolled 85 patients with relapsed/refractory chronic lymphocytic leukemia/small lymphocytic leukemia into two cohorts: 51 received a 420-mg daily dose and 34 received an 840-mg daily dose. The majority of these patients had high-risk and advanced-stage disease (65%), 17p13.1 deletion (33%), and 11q22.3 deletion (36%). The median age was 66 years (range 37–82 years). Median number of prior therapies was 4 (range, 1–12). Most AEs were grade 1/2 and included diarrhea, fatigue, and upper respiratory tract infection. The ORR was 71% in both groups of patients (with 2 CRs and 34 PRs in the 420-mg cohort and 24 PRs in the 840-mg cohort). An additional 20% of patients in the 420-mg cohort and 15% of patients in the 840-mg cohort had PRs with lymphocytosis. Responses were independent of high-risk features. At 26 months, the estimated PFS was 75% and the OS was 83%.
Based on the treatment outcomes of 48 patients with chronic lymphocytic leukemia in the 420-mg group of patients on this trial, the FDA granted accelerated approval to ibrutinib in February 2014 for the treatment of patients with chronic lymphocytic leukemia who have received at least one prior therapy. The efficacy results demonstrated an ORR of 58.3% as assessed by an independent review committee. No CRs were observed in this set of patients, and the response duration ranged from 5.6 to 24.2+ months (median not reached).
Subsequently, a randomized, open-label, multicenter phase III trial of 391 patients confirmed the benefit of ibrutinib in relapsed/refractory chronic lymphocytic leukemia/small lymphocytic lymphoma.[22] Patients were randomized between single-agent ibrutinib (n = 195) at 420-mg orally daily and single-agent IV ofatumumab (n = 196). The median age was 67 years (range, 30–86 years in the ibrutinib arm; and 37–88 years in the ofatumumab arm), and the median number of prior therapies was 3 in the ibrutinib arm (range, 1–12) and 2 in the ofatumumab arm (range, 1–13). Median follow-up was 9.4 months.
PFS was 88% at 6 months and the median PFS had not been reached, whereas median PFS for the ofatumumab arm was 8.1 months (P < .001). Ibrutinib also significantly improved OS compared with ofatumumab (P = .005). At 12 months, OS was 90% in the ibrutinib group vs 81% in the ofatumumab group. The ORR was significantly higher in the ibrutinib arm as well (42.6% vs 4.1% with ofatumumab; P < .001). An additional 20% patients in the ibrutinib arm had PRs with lymphocytosis. Results were independent of high-risk features.
The most common AEs were diarrhea, fatigue, pyrexia, and nausea in the ibrutinib arm; and fatigue, infusion reactions, and cough in the ofatumumab arm. Of interest, 3% patients in the ibrutinib arm developed cataracts compared with 1% in the ofatumumab arm. A total of 10 patients in the ibrutinib arm developed atrial fibrillation of any grade compared with 1 patient in the ofatumumab arm. Potential reasons for atrial fibrillation in ibrutinib-treated patients are under investigation. The rates of major hemorrhage were similar in the two arms of this study; warfarin was not allowed on study. One patient on ibrutinib developed a subdural hematoma, and mild bleeding episodes were more common in the ibrutinib arm. Further studies to explain this bleeding risk with ibrutinib are being performed.
A prospective multicenter trial of ibrutinib in patients with relapsed/refractory Waldenström macroglobulinemia enrolled 63 patients.[23] The median age was 63 years (range, 44–86 years), and patients had received a median of 2 prior therapies (range, 1–6). Mutations of MYD88 and CXCR4 were determined by sequencing in most patients. Mutation of MYD88 L265P is present in > 90% of Waldenström macroglobulinemia patients and enhances malignant cell growth via BTK signaling. In vitro, ibrutinib induces apoptosis in these cells.[24] CXCR4 WHIM (warts, hypogammaglobulinemia, immunodeficiency, myelokathexis) syndrome–like mutations lead to ibrutinib resistance in Waldenström macroglobulinemia cells.[25] These mutations are present in one-third of patients with Waldenström macroglobulinemia and induce BTK activity while conferring resistance to ibrutinib. In this prospective study in Waldenström macroglobulinemia, 93% of 43 tested patients harbored the MYD88 L265P mutation, while 25% of 40 tested patients had the WHIM syndrome–like CXCR4 mutation. All patients received 420 mg/d of ibrutinib for 2 years or until disease progression. The ORR was 57.1% (36 PRs) and was not impacted by MYD88 L265P mutations. However, the ORR was 77% in patients with wild-type CXCR4 and 30% for those with WHIM-like CXCR4 mutations (P = .018). Although ibrutinib is quite active in Waldenström macroglobulinemia, it appears that patients with WHIM-like CXCR4 mutations may not respond as well to it. In January 2015, the FDA expanded the approval of ibrutinib to include treatment of Waldenström macroglobulinemia patients. This is the first agent to ever receive FDA approval specifically for the treatment of Waldenström macroglobulinemia.
Other BTK inhibitors. Agents such as CC-292 and ONO-4059 are now being studied in early-phase chronic lymphocytic leukemia/non-Hodgkin lymphoma clinical trials. Both bind the cysteine 481 residue in BTK covalently like ibrutinib and appear to generate good responses and are safe and well tolerated.[26-28]
PI3K delta inhibitors
Idelalisib. Signaling through the BCR is mediated in part by the activation of PI3Kδ. This isoform is highly expressed in lymphoid cells and is the most important isoform in chronic lymphocytic leukemia. Idelalisib is a first-in-class, potent, oral, selective small-molecule inhibitor of PI3Kδ. In preclinical studies, idelalisib blocked PI3Kδ-AKT signaling and promoted apoptosis.[17,29] Phase I and II studies in hematologic malignancies have shown idelalisib to have an acceptable safety profile and promising antitumor activity in patients with relapsed/refractory indolent non-Hodgkin lymphoma and chronic lymphocytic leukemia/small lymphocytic lymphoma.[30-32]
A phase III, randomized, double blind, placebo-controlled trial of combination therapy with idelalisib and rituximab vs placebo and rituximab in 220 medically unfit patients with relapsed/refractory chronic lymphocytic leukemia was recently published.[33] Idelalisib was administered at a dosage of 150 mg orally twice a day. There were 110 patients in each arm. Patients in the placebo group who experienced disease progression could enroll in an extension study to receive idelalisib. Patients in the idelalisib group who had disease progression could receive a higher dose of idelalisib of 300 mg orally twice a day. The median age of patients was 71 years (range, 48–90 years in the idelalisib + rituximab arm; and 47–92 years in the placebo + rituximab arm). Median number of prior therapies was 3 (range, 1–12 in the idelalisib + rituximab arm, 1–9 in the placebo + rituximab arm) and the median Cumulative Illness Rating Scale score was 8. A total of 40% of patients had at least moderate renal dysfunction (creatinine clearance < 60 mL/min) and 35% had poor bone marrow function (grade 3 or higher anemia, thrombocytopenia, or neutropenia). More than 80% of patients had unmutated IgHV, and more than 40% had 17p deletion or TP53 mutations. The median PFS was 5.5 months for the placebo group and was not reached in the idelalisib group (P < .001). Patients in the idelalisib group had a significantly improved ORR (all PRs) compared with the placebo group (81% vs 13%; P < .001), and the OS rates at 12 months were 92% vs 80%, respectively (P = .02). Treatment effect was equally favorable in patients with high-risk features such as 17p deletion or TP53 mutations and unmutated IgHV status. Most AEs were grade 1 or 2. In the idelalisib arm, grade 3 or higher diarrhea was reported in four patients and grade 3 or higher rash in two patients. There was no grade 3 or higher diarrhea or rash in the placebo group. Common laboratory abnormalities included anemia, neutropenia, thrombocytopenia, and transaminitis. Grade 3 or higher transaminitis was reported in six patients (5%) in the idelalisib arm, with onset at 8–16 weeks. Serious AEs occurred in 40% of patients in the idelalisib group and in 35% of those in the placebo group; the most common AEs were pneumonia, pyrexia, and febrile neutropenia. Severe diarrhea is a late-onset AE with idelalisib, and since the study was halted early for efficacy, this may still occur in some patients; its prevalence will need to be evaluated with future updates. In July 2014, based on these data, the FDA approved idelalisib for the treatment of relapsed chronic lymphocytic leukemia, in combination with rituximab, where rituximab alone would be considered appropriate therapy due to a patient’s other comorbidities.
A phase II, open label, multicenter trial of idelalisib in 125 patients with relapsed indolent non-Hodgkin lymphoma was also published at the same time as the above study.[34] The median age of patients was 64 years (range, 33–87 years) and patients had received a median of 4 prior therapies (range, 2–12). In the study group, 58% of patients had follicular lymphoma, 22% had small lymphocytic lymphoma, 12% had marginal zone lymphoma, and 8% had lymphoplasmacytic lymphoma/Waldenström macroglobulinemia. Median follow-up was 9.7 months. The ORR was 57% (6% CRs, 50% PRs). Median time to response was 1.9 months, median duration of response was 12.5 months, and median PFS was 11 months. Response rates were similar in all subtypes of indolent non-Hodgkin lymphoma. Median OS was 20.3 months, and the 1-year OS was estimated to be 80%. The most common grade 3 or higher AEs were neutropenia (27%), transaminitis (13%, occurring at a median of 6.3 weeks after initiation of treatment; range 4–11 weeks after starting treatment), diarrhea (13%), and pneumonia (7%). The most common serious AEs included pyrexia (10%), pneumonia and diarrhea (7% each), colitis (4%), dehydration and febrile neutropenia (3% each), and acute renal failure and pneumonitis (2% each). Grade 3 or higher diarrhea, colitis, or both developed in 16% of patients at a median of 6 months after initiation of treatment (range, 1–13 months). A total of 22% deaths were reported, primarily related to disease progression. No cumulative toxicities with idelalisib were reported. Based on this study, the FDA granted accelerated approval to idelalisib in July 2014 for the treatment of patients with relapsed follicular lymphoma or small lymphocytic lymphoma who have received at least 2 prior systemic therapies.
Duvelisib (IPI-145). This is another PI3K inhibitor now being studied in early clinical trials. It is a potent inhibitor of the delta and gamma isoforms of PI3K. In a phase I study, in 32 patients with indolent non-Hodgkin lymphoma, the ORR was 65%, including 25% CRs.[35] Overall, the safety profile was acceptable, but a 41% rate of transaminitis and 25% rate of diarrhea was observed. The ORR in 49 evaluable patients with relapsed/refractory chronic lymphocytic leukemia was 55%, including 1 CR and 26 PRs.[36] The safety profile was acceptable. Clinical activity in patients with relapsed/refractory T-cell non-Hodgkin lymphoma has also been reported in a phase I study.[37] The ORR was 42%, with 2 CRs and 11 PRs among 33 patients. Transaminitis was the most common AE (36%). Registration/randomized trials in indolent non-Hodgkin lymphoma and chronic lymphocytic leukemia are ongoing.
TGR-1202. This selective PI3Kδ inhibitor is also under investigation in early-phase studies. It may have less hepatotoxicity than other PI3Kδ inhibitors due to significant structural differences. In a phase I study, in 23 evaluable patients, 10 were treated at ≥ 800-mg once-daily dosing.[38] Of these, four of six patients with chronic lymphocytic leukemia (67%) achieved nodal PR, and one of three patients (33%) with Hodgkin lymphoma achieved a PR. Nodal reductions occurred rapidly in patients with chronic lymphocytic leukemia and were accompanied by marked lymphocytosis. Combination studies are now underway.
B-cell chronic lymphocytic leukemia/lymphoma-2 (BCL-2) family inhibitors
BCL-2 family proteins are key apoptotic regulators and play a dominant role in normal and malignant lymphoid cells. These agents comprise pro-survival and pro-apoptotic proteins; in chronic lymphocytic leukemia/non-Hodgkin lymphoma, their balance is shifted to pro-survival, thereby allowing the malignant cells to evade apoptosis.
Navitoclax (ABT-263). The first-generation BCL-2 pathway inhibitor navitoclax (previously known as ABT-263) led to BH3-mimetic effects that shifted the balance towards apoptosis.In a phase I study, it yielded ORRs of 35% (all PRs) in heavily pretreated patients with chronic lymphocytic leukemia[39] and 21.7% in patients with relapsed/refractory non-Hodgkin lymphoma.[40] However, thrombocytopenia was a major dose-limiting side effect of navitoclax, due to the drug’s inhibition of Bcl-XL on platelets.
ABT-199. This agent is a potent second-generation BCL-2 pathway inhibitor that is highly selective for BCL-2, thereby causing less thrombocytopenia as a side effect. It also functions as a BH3 mimetic to enhance apoptosis. The main toxicity in early-phase studies has been tumor lysis syndrome (TLS), related to the potency of this drug; the dose-escalation scheme has been modified to prevent and manage this side effect.[41] In the ongoing phase I study of patients with high-risk relapsed/refractory chronic lymphocytic leukemia, there is now a cohort-expansion study to assess the safety of ABT-199. In this cohort, there is a lead-in phase of 5 weeks in which treatment with ABT-199 is initiated at 20 mg/d orally and increased weekly to 50 mg, 100 mg, 200 mg, and finally, 400 mg daily.[42]
If there is a high risk of TLS based on the level of absolute lymphocytosis and the degree of bulky lymphadenopathy, then the initial dose escalations of the lead-in phase are done in the hospital so that aggressive tumor lysis prophylaxis and monitoring can be performed. A total of 93 patients were enrolled, with a median age of 66 years. The median number of prior therapies was 4 (range, 1–11). The most common grade 3 or higher AEs were neutropenia (36%), anemia (10%), TLS (8%, including 1 grade 5 event), thrombocytopenia (7%), hyperglycemia (7%), and febrile neutropenia and hypokalemia (6% each). In 70 efficacy-evaluable patients, the ORR was 76% (20% CRs, 56% PRs); some minimal residual disease–negative cases have also been reported. Median duration of responses was 20.5 months.
In relapsed/refractory non-Hodgkin lymphoma, a phase I study of ABT-199 therapy is ongoing.[43] ABT-199 was given on week 1 day 7 followed by continuous, once-daily dosing from week 1 day 1 until progressive disease or unacceptable toxicity. A 2- to 3-week lead-in period with stepwise dose titration was implemented. A total of 44 patients were enrolled: 15 (35%) with mantle cell lymphoma, 11 (26%) with follicular lymphoma, 10 (23%) with diffuse large B-cell lymphoma, 4 (9%) with Waldenström macroglobulinemia, 2 (5%) with marginal zone lymphoma, 1 (2%) with primary mediastinal B-cell lymphoma, and 1 (2%) with multiple myeloma. The most common grade 3 or higher AEs were anemia (14%), neutropenia (11%), and thrombocytopenia (9%). Grade 3 laboratory evidence of TLS was seen after the initial dose in one patient with bulky mantle cell lymphoma (elevations in phosphate and potassium only) and one patient with diffuse large B-cell lymphoma (elevations in phosphate and uric acid only). In the 40 efficacy-evaluable patients, the ORR was 48%, including 3 CRs and 16 PRs, most notably in patients with mantle cell lymphoma and Waldenström macroglobulinemia. Responses were seen across a wide range of doses, but all responses in diffuse large B-cell lymphoma and follicular lymphoma patients were at doses > 600 mg.
Studies of combination therapies in this setting are underway and registration trials are being planned for this extremely promising agent. A phase II study of single-agent ABT-199 in 17p deleted relapsed/refractory chronic lymphocytic leukemia is ongoing, and the trial is being amended to add a cohort of previously untreated 17p-deleted chronic lymphocytic leukemia patients.
Immunomodulation
Lenalidomide
Mantle cell lymphoma accounts for 3% to 6% of cases of non-Hodgkin lymphoma.[44] It manifests aggressive clinical activity in most patients, especially in the relapsed/refractory setting, at which point most patients are chemoresistant. Newer treatment modalities are being sought to improve survival. Lenalidomide is an immunomodulatory agent initially studied in multiple myeloma and myelodysplastic syndromes. Its mechanism of action has recently been linked to the protein cereblon, a member of the ubiquitin-proteosome pathway.[45] Preclinical studies have shown it has antitumor activity in lymphomas as well. Phase II studies have shown clinical activity of lenalidomide in patients with non-Hodgkin lymphoma, with higher (35% to 53%) and more durable (13.7 to 16.3 months) responses in mantle cell lymphoma patients compared with other subtypes.[46-49]
The MCL-001 (EMERGE) lenalidomide study was another phase II, multicenter trial in patients with mantle cell lymphoma who had failed prior chemoimmunotherapy and bortezomib.[50] Lenalidomide was administered to 134 patients at 25 mg/d orally on days 1 through 21 every 28 days until disease progression or intolerance. The median age was 67 years (range, 43–83 years), and the median number of prior therapies was 4 (range, 2–10). The ORR was 28% (7.5% CR/unconfirmed CR, 20% PRs), with a median time to response of 2.2 months. Median duration of response was 16.6 months, median PFS was 4 months, and median OS was 19 months. The most common grade 3 or higher toxicities were neutropenia (43%), thrombocytopenia (28%), anemia (11%), pneumonia (8%), and fatigue (7%). Based on these data, in June 2013 the FDA approved lenalidomide for patients with mantle cell lymphoma whose disease has relapsed or progressed after two prior therapies, one of which included bortezomib.
Other Novel Therapies
Rapid advances are also being made in the development of other small-molecule inhibitors and targeted agents. The Table summarizes some of the available data on these novel therapies. Further studies are ongoing.
Conclusion
A vast number of promising novel agents are now being studied in clinical trials, as monotherapy and in combination therapy, in order to improve outcomes in patients with relapsed/refractory non-Hodgkin lymphoma. The most promising novel therapies-some of which are being studied further in the frontline setting as well-include novel monoclonal antibodies, antibody-drug conjugates, CAR T cells, small-molecule inhibitors, and immunomodulators. In addition, more novel agents are in the pipeline. It remains to be seen how these will be prioritized for therapy in the coming years as they receive FDA approval. In the meantime, patients with non-Hodgkin lymphoma and chronic lymphocytic leukemia now have tremendous treatment options both off and on clinical trials. For example, patients with more indolent diseases may be able to avoid standard chemotherapy altogether and opt to be treated only with targeted therapies like small molecule inhibitors and monoclonal antibodies. For the more aggressive lymphoid malignancies, combinations of novel biologic agents with more standard chemoimmunotherapy are being studied and promise improved outcomes; in the relapsed/refractory setting, this approach may ultimately serve as a bridge to allogeneic HSCT. CAR T-cell therapy is attempting to provide even more durable responses than the other novel systemic therapies. Potential limitations may be development of resistance mechanisms as well as prohibitive costs. However, the fact that multiple useful novel therapeutic options are now available for patients with non-Hodgkin lymphoma and chronic lymphocytic leukemia makes this an exiciting time in the treatment of these diseases.
Financial Disclosure:Dr. Siddiqi is a speaker for Janssen, Pharmacyclics, and Seattle Genetics. Dr. Rosen has no significant financial interest or other relationship with the manufacturers of any products or providers of any service mentioned in this article.
References:
1. Chao MP. Treatment challenges in the management of relapsed or refractory non-Hodgkin’s lymphoma-novel and emerging therapies. Cancer Manag Res. 2013;5:251-69.
2. Zelenetz AD, Abramson JS, Advani RH, et al. NCCN Clinical Practice Guidelines in Oncology: non-Hodgkin’s lymphomas. J Natl Compr Canc Netw. 2010;8:288-334.
3. Carpenito C, Milone MC, Hassan R, et al. Control of large, established tumor xenografts with genetically retargeted human T cells containing CD28 and CD137 domains. Proc Natl Acad Sci U S A. 2009;106:3360-5.
4. Kalos M, Levine BL, Porter DL, et al. T cells with chimeric antigen receptors have potent antitumor effects and can establish memory in patients with advanced leukemia. Sci Transl Med. 2011;3:95ra73.
5. Porter DL, Levine BL, Kalos M, et al. Chimeric antigen receptor-modified T cells in chronic lymphoid leukemia. N Engl J Med. 2011;365:725-33.
6. Porter DL. Chimeric antigen receptor modified T cells directed against CD19 (CTL019 cells) have long-term persistence and induce durable responses in relapsed, refractory CLL Blood. 2013;122:4162.
7. Porter DL. Randomized, phase II dose optimization study of chimeric antigen receptor modified T cells directed against CD19 (CTL019) in patients with relapsed, refractory CLL. Blood. 2014;124:1982.
8. Brentjens RJ, Davila ML, Riviere I, et al. CD19-targeted T cells rapidly induce molecular remissions in adults with chemotherapy-refractory acute lymphoblastic leukemia. Sci Transl Med. 2013;5:177ra38.
9. Grupp SA, Kalos M, Barrett D, et al. Chimeric antigen receptor-modified T cells for acute lymphoid leukemia. N Engl J Med. 2013;368:1509-18.
10. Maude SL, Frey N, Shaw PA, et al. Chimeric antigen receptor T cells for sustained remissions in leukemia. N Engl J Med. 2014;371:1507-17.
11. Kochenderfer JN, Dudley ME, Feldman SA, et al. B-cell depletion and remissions of malignancy along with cytokine-associated toxicity in a clinical trial of anti-CD19 chimeric-antigen-receptor-transduced T cells. Blood. 2012; 119: 2709-20.
12. Kochenderfer JN, Dudley ME, Kassim KH, et al. Chemotherapy-refractory diffuse large B-cell lymphoma and indolent B-cell malignancies can be effectively treated with autologous T cells expressing an anti-CD19 chimeric antigen receptor. Clin Oncol. 2014;33:540-9.
13. Kochenderfer JN, Dudley ME, Kassim SH, et al. Chemotherapy-refractory diffuse large B-cell lymphoma and indolent B-cell malignancies can be effectively treated with autologous T cells expressing an anti-CD19 chimeric antigen receptor. J Clin Oncol. 2015;33:540-9.
14. Honigberg LA, Smith AM, Sirisawad M, et al. The Bruton tyrosine kinase inhibitor PCI-32765 blocks B-cell activation and is efficacious in models of autoimmune disease and B-cell malignancy. Proc Natl Acad Sci USA. 2010;107:13075-80.
15. Ponader S, Chen SS, Buggy JJ, et al. The Bruton tyrosine kinase inhibitor PCI-32765 thwarts chronic lymphocytic leukemia cell survival and tissue homing in vitro and in vivo. Blood. 2012;119:1182-9.
16. Advani RH, Buggy JJ, Sharman JP, et al. Bruton tyrosine kinase inhibitor ibrutinib (PCI-32765) has significant activity in patients with relapsed/refractory B-cell malignancies. J Clin Oncol. 2013;31:88-94.
17. Hoellenriegel J, Meadows SA, Sivina M, et al. The phosphoinositide 3’-kinase delta inhibitor, CAL-101, inhibits B-cell receptor signaling and chemokine networks in chronic lymphocytic leukemia. Blood. 2011;118:3603-12.
18. Cheson BD, Byrd JC, Rai KR, et al. Novel targeted agents and the need to refine clinical end points in chronic lymphocytic leukemia. J Clin Oncol. 2012;30:2820-2.
19. Wang ML, Rule S, Martin P, et al. Targeting BTK with ibrutinib in relapsed or refractory mantle-cell lymphoma. N Engl J Med. 2013;369:507-16.
20. Byrd JC, Furman RR, Coutre SE, et al. Targeting BTK with ibrutinib in relapsed chronic lymphocytic leukemia. N Engl J Med. 2013;369:32-42.
21. O’Brien S, Furman RR, Coutre SE, et al. Ibrutinib as initial therapy for elderly patients with chronic lymphocytic leukaemia or small lymphocytic lymphoma: an open-label, multicentre, phase 1b/2 trial. Lancet Oncol. 2014;15:48-58.
22. Byrd JC, Brown JR, O’Brien S, et al. Ibrutinib versus ofatumumab in previously treated chronic lymphoid leukemia. N Engl J Med. 2014;371:213-23.
23. Treon SP. A prospective multicenter study of the Bruton’s tyrosine kinase inhibitor ibrutinib in patients with relapsed or refractory Waldenstrom’s macroglobulinemia. Blood. 2013;122:251.
24. Yang G, Zhou Y, Liu X, et al. A mutation in MYD88 (L265P) supports the survival of lymphoplasmacytic cells by activation of Bruton tyrosine kinase in Waldenstrom macroglobulinemia. Blood. 2013;122:1222-32.
25. Cao Y, Hunter ZR, Liu X, et al. CXCR4 WHIM-like frameshift and nonsense mutations promote ibrutinib resistance but do not supplant MYD88 -directed survival signalling in Waldenstrom macroglobulinaemia cells. Br J Haematol. 2015;168:701-7.
26. Brown JR. Phase 1 study of single agent CC-292, a highly selective Bruton’s tyrosine kinase (BTK) inhibitor, in relapsed/refractory chronic lymphocytic leukemia (CLL). Blood. 2013;122:1630.
27. Rule S. A phase I study of the oral Btk inhibitor ONO-4059 in patients with relapsed/refractory B-cell lymphoma. Blood. 2013;122:4397.
28. Salles GA. A phase I study of the oral Btk inhibitor ONO-4059 in patients with relapsed/refractory and high risk chronic lymphocytic leukaemia (CLL). Blood. 2013;122:676.
29. Lannutti BJ, Meadows SA, Herman SE, et al. CAL-101, a p110delta selective phosphatidylinositol-3-kinase inhibitor for the treatment of B-cell malignancies, inhibits PI3K signaling and cellular viability. Blood. 2011;117:591-4.
30. Flinn IW, Kahl BS, Leonard JP, et al. Idelalisib, a selective inhibitor of phosphatidylinositol 3-kinase-delta, as therapy for previously treated indolent non-Hodgkin lymphoma. Blood. 2014;123:3406-13.
31. Brown JR, Byrd JC, Coutre SE, et al. Idelalisib, an inhibitor of phosphatidylinositol 3-kinase p110delta, for relapsed/refractory chronic lymphocytic leukemia. Blood. 2014;123:3390-7.
32. Kahl BS, Spurgeon SE, Furman RR, et al. A phase 1 study of the PI3Kdelta inhibitor idelalisib in patients with relapsed/refractory mantle cell lymphoma (MCL). Blood. 2014;123:3398-405.
33. Furman RR, Sharman JP, Coutre SE, et al. Idelalisib and rituximab in relapsed chronic lymphocytic leukemia. N Engl J Med. 2014;370:997-1007.
34. Gopal AK, Kahl BS, de Vos S, et al. PI3Kdelta inhibition by idelalisib in patients with relapsed indolent lymphoma. N Engl J Med. 2014;370:1008-18.
35. Flinn I. A phase 1 evaluation of duvelisib (IPI-145), a PI3K-δγ inhibitor, in patients with relapsed/refractory iNHL. Blood 2014;124:802.
36. O’Brien S. Duvelisib (IPI-145), a PI3K-δ,γ inhibitor, is clinically active in patients with relapsed/refractory chronic lymphocytic leukemia. Blood. 2014;124:3334.
37. Horowitz SM. Duvelisib (IPI-145), a phosphoinositide-3-kinase-δγ inhibitor, shows activity in patients with relapsed/refractory T-cell lymphoma. Blood. 2014;124:803.
38. Burris HA. TGR-1202, a novel once daily PI3K delta inhibitor, demonstrates promising clinical activity with a favorable safety profile in patients with relapsed or refractory hematologic malignancies. Haematologica. 2014;99:P250.
39. Roberts AW, Seymour JF, Brown JR, et al. Substantial susceptibility of chronic lymphocytic leukemia to BCL2 inhibition: results of a phase I study of navitoclax in patients with relapsed or refractory disease. J Clin Oncol. 2012;30:488-96.
40. Wilson WH, O’Connor OA, Czuczman MS, et al. Navitoclax, a targeted high-affinity inhibitor of BCL-2, in lymphoid malignancies: a phase 1 dose-escalation study of safety, pharmacokinetics, pharmacodynamics, and antitumour activity. Lancet Oncol. 2010;11:1149-59.
41. Seymour JF. Reduction of tumor lysis syndrome (TLS) risk in chronic lymphocytic leukemia (CLL) patients treated with ABT-199 (GDC-0199): results of modifications to dosing schedule and TLS prophylaxis. Haematologica. 2014;2014:abstr P868.
42. Seymour JF. ABT-199 (GDC-0199) in relapsed/refractory chronic lymphocytic leukemia and small lymphocytic lymphoma: high response rates among patients with high risk disease features including unmutated IGHV. Haematologica. 2014;99:abstr S702.
43. Davids MS. Phase I study of ABT-199 (GDC-0199) in patients with relapsed/refractory (R/R) non-Hodgkin lymphoma (NHL): responses observed in diffuse large B-cell (DLBCL) and follicular lymphoma (FL) at higher cohort doses. J Clin Oncol. 2014;32:abst 8522.
44. Zhou Y, Wang H, Fang W, et al. Incidence trends of mantle cell lymphoma in the United States between 1992 and 2004. Cancer. 2008;113:791-8.
45. Chamberlain PP, Lopez-Girona A, Miller K, et al. Structure of the human Cereblon-DDB1-lenalidomide complex reveals basis for responsiveness to thalidomide analogs. Nat Struct Mol Biol. 2014;21:803-9.
46. Wiernik PH, Lossos IS, Tuscano JM, et al. Lenalidomide monotherapy in relapsed or refractory aggressive non-Hodgkin’s lymphoma. J Clin Oncol. 2008;26:4952-7.
47. Witzig TE, Vose JM, Zinzani PL, et al. An international phase II trial of single-agent lenalidomide for relapsed or refractory aggressive B-cell non-Hodgkin’s lymphoma. Ann Oncol. 2011;22:1622-7.
48. Habermann TM, Lossos IS, Justice G, et al. Lenalidomide oral monotherapy produces a high response rate in patients with relapsed or refractory mantle cell lymphoma. Br J Haematol. 2009;145:344-9.
49. Zinzani PL, Vose JM, Czuczman MS, et al. Long-term follow-up of lenalidomide in relapsed/refractory mantle cell lymphoma: subset analysis of the NHL-003 study. Ann Oncol. 2013;24:2892-7.
50. Goy A, Sinha R, Williams ME, et al. Single-agent lenalidomide in patients with mantle-cell lymphoma who relapsed or progressed after or were refractory to bortezomib: phase II MCL-001 (EMERGE) study. J Clin Oncol. 2013;31:3688-95.
51. Friedberg JW, Sharman J, Sweetenham J, et al. Inhibition of Syk with fostamatinib disodium has significant clinical activity in non-Hodgkin lymphoma and chronic lymphocytic leukemia. Blood. 2010;115:2578-85.
52. Sharman J. Phase 2 Trial of GS-9973, a selective Syk Inhibitor, in chronic lymphocytic leukemia (CLL) and non-Hodgkin lymphoma (NHL). Blood. 2013;122:1634.
53. Sharman J. Phase 2 trial of entospletinib (GS-9973), a selective SYK inhibitor, in follicular lymphoma (FL). Blood. 2014;124:4419.
54. Guidetti A, Carlo-Stella C, Locatelli SL, et al. Phase II study of perifosine and sorafenib dual-targeted therapy in patients with relapsed or refractory lymphoproliferative diseases. Clin Cancer Res. 2014;20:5641-51.
55. Witzig TE, Reeder CB, LaPlant BR, et al. A phase II trial of the oral mTOR inhibitor everolimus in relapsed aggressive lymphoma. Leukemia. 2011;25:341-7.
56. Zent CS, LaPlant BR, Johnston PB, et al. The treatment of recurrent/refractory chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL) with everolimus results in clinical responses and mobilization of CLL cells into the circulation. Cancer. 2010;116:2201-7.
57. Smith SM, van Besien K, Karrison T, et al. Temsirolimus has activity in non-mantle cell non-Hodgkin’s lymphoma subtypes: the University of Chicago phase II consortium. J Clin Oncol. 2010;28:4740-6.
58. Hess G, Herbrecht R, Romaguera J, et al. Phase III study to evaluate temsirolimus compared with investigator’s choice therapy for the treatment of relapsed or refractory mantle cell lymphoma. J Clin Oncol. 2009;27:3822-9.
59. Gambacorti-Passerini C. Safety and clinical activity of crizotinib in patients with ALK-rearranged hematologic malignancies. Blood. 2013;122:4342.
60. Redaelli S. High response rates to crizotinib in advanced, chemoresistant ALK+ lymphoma patients. Blood. 2013;122:368.
61. Cavalli F. Randomized phase 3 study of rituximab, cyclophosphamide, doxorubicin, and prednisone plus vincristine (R-CHOP) or bortezomib (VR-CAP) in newly diagnosed mantle cell lymphoma (MCL) patients (pts) ineligible for bone marrow transplantation (BMT). J Clin Oncol. 2014;32:abstr 8500.
62. Treon SP, Tripsas CK, Meid K, et al. Carfilzomib, rituximab, and dexamethasone (CaRD) treatment offers a neuropathy-sparing approach for treating Waldenstrom’s macroglobulinemia. Blood. 2014;124:503-10.
63. O’Connor OA. Belinostat, a novel pan-histone deacetylase inhibitor (HDACi), in relapsed or refractory peripheral T-cell lymphoma (R/R PTCL): results from the BELIEF trial. J Clin Oncol. 2013;31:abstr 8507.