Post-treatment pain remains clinically significant in breast cancer patients
Many women continue to experience pain and sensory disturbance up to three years after breast cancer treatment, according to Danish researchers, who found that younger women in particular reported persistent pain. They called for further strategies for improving pain management after breast surgery.
Many women continue to experience pain and sensory disturbance up to three years after breast cancer treatment, according to Danish researchers, who found that younger women in particular reported persistent pain. They called for further strategies for improving pain management after breast surgery.
Lead author Rune Grtner, MD, and colleagues examined the prevalence, associated factors, and severity of chronic pain and sensory disturbances (see Fact box) after breast cancer treatment, including surgery, radiotherapy, and chemotherapy. They used data from a national database run by the Danish Breast Cancer Cooperative Group (DBCG).

Dr. Grtner and coauthors Henrik Kehlet, MD, PhD, and Niels Kroman, MD, DMSc, are from the University of Copenhagen. Other coauthors are from the DBCG. Marianne Ewertz, MD, DMSc, from the department of oncology at Odense University Hospital in Denmark, also contributed to this report.
Survey yields high response rate
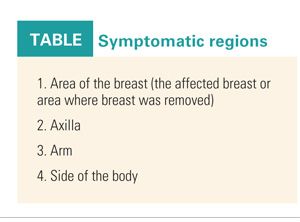
Between 2005 and 2006, 5,119 Danish women (aged 18-70) underwent surgery for unilateral primary breast cancer. Of these, 3,754 were included in the current study. They were sent a questionnaire in early 2008, and 87% returned the surveys by June. The women were asked to address four regions where they might experience symptoms (see Table), the severity of pain, and the frequency of the symptoms. The mean time from surgery to the returned questionnaire was 26 months (JAMA 302:1985-1992, 2009).
All of the women in the study received treatment based on the DBCG 2004 treatment protocol. Procedures included mastectomy and breast-conserving surgery (BCS) with either sentinel lymph node dissection or axillary lymph node dissection (ALND). All patients who had BCS also received radiotherapy to residual breast tissue (48 Gy in 24 fractions).
Node-positive patients who underwent mastectomy received radiation therapy to the anterior thoracic wall (48 Gy in 24 fractions). On the basis of their estrogen-receptor status and histopathology, patients underwent antiestrogen treatment and standard chemotherapy with cyclophosphamide (Cytoxan), epirubicin (Ellence), and 5-fluorouracil.
Light to moderate pain persists
Of the respondents, 47% reported pain in one area. Of these 1,543 patients, the majority described light pain (48%). Pain in the breast area was reported most frequently (86% of the women), followed by pain in the axilla (63%). The mean pain score in the four areas varied from 3.5 to 4.0 (0 = no pain; 10 = worst pain). To alleviate the pain, 28% reported taking analgesics.
The authors found a significant association with age and pain, with younger age linked to a higher risk. This was especially true in women, aged 18-39, who had undergone BCS (odds ratio [OR] = 3.62; P < .001). While younger age did not correlate with severity of pain, it was a factor in persistent pain and sensory disturbance.
There was no association between chronic pain and chemotherapy. However, they pointed out that these results applied to the standard DBCG chemotherapy regimen and may not be applicable to taxane-based regimens. Also, very few women in the study received aromatase inhibitors. Other notable results:
• Women who reported pain after mastectomy had a higher risk of moderate to severe pain.
• ALND was associated with an increased risk of pain.
• Adjuvant radiotherapy was associated with an increased risk of pain.
• Adjuvant chemotherapy had no association with adjusted OR for pain.
• Type of breast surgery was not related to pain in the axilla.
The authors concluded that chronic pain after surgery and adjuvant therapy “may predominantly be characterized as a neuropathic pain state and is probably related to intraoperative injury of the intercostal-brachial nerve.” They suggested several options for reducing the risk of pain, including a nerve-sparing technique; extensive neurophysiologic exams; pharmacologic intervention; and a possible link between postsurgical pain with other pain symptoms, such as headache. It is possible that some women have preoperative pain hypersensitivity because of psychosocial or genetic factors, they said.
Dr. Kehlet told Oncology News International that the results of their study have not influenced the way post-treatment pain is managed at his institution. “[Our] protocol for pain management for persistent pain follows usual guidelines for neuropathic pain management, but based on our study we will have an increased focus on how to improve and prevent chronic pain in these patients,” he said. Dr. Kehlet is from the section for surgical pathophysiology at the University of Copenhagen. He said the group will continue with their research, looking at pain-gene analyses, evaluation of nerve-sparing techniques, specific effects of taxanes, and pharmacologic as well as operative prophylaxis. They will continue with patient observation to see whether there is a decrease in pain over time.
Dr. Laronga, along with co-commentator Loretta S. Loftus, MD, MBA, called these study results “compelling.” They said that “patients at high risk for the development of postsurgical pain syndrome should be identified, should have therapy initiated early, and the effects of early intervention should be assessed” (JAMA 302:2034-2035, 200

9).
Dr. Loftus is a senior member at the Don and Erika Wallace Comprehensive Breast Program, H. Lee Moffitt Cancer Center & Research Institute in Tampa, Fla. Dr. Laronga is an associate member.
The strengths of this study included the large patient population and the standardization of treatment principles across all of the breast cancer facilities in Denmark. However, the relative homogeneity of the Danish population may make it difficult to generalize these results to other countries with more varied patients, procedures, socioeconomic conditions, and healthcare systems.
Nevertheless, “the most valuable finding...may well be identification of predictors associated with highest risk for development of pain, and these predictors have not been emphasized to date,” the commentators wrote.
They suggested that further research should include data on the effect of systemic adjuvant chemotherapy and endocrine-based therapies on pain outcomes.
Also, pain management requires a multidisciplinary approach that includes evaluation by cancer care specialists as well as psychiatrists, social workers, and experts in rehabilitation medicine.