Postoperative RT Boosts Survival in N2 Lung Ca Patients
Postoperative radiotherapy, added to adjuvant cisplatin-based chemotherapy, resulted in a near-doubling of median survival in patients with completely resected non-small-cell lung cancer (NSCLC), compared with chemotherapy alone—but only in the presence of mediastinal lymph node involvement (N2 disease).
PHILADELPHIAPostoperative radiotherapy, added to adjuvant cisplatin-based chemotherapy, resulted in a near-doubling of median survival in patients with completely resected non-small-cell lung cancer (NSCLC), compared with chemotherapy alonebut only in the presence of mediastinal lymph node involvement (N2 disease). Radiation had a deleterious effect on survival in chemotherapy-treated patients with N1 or node-negative disease, Jean-Yves Douillard, MD, PhD, reported at the 48th Annual Meeting of the American Society for Therapeutic Radiology and Oncology (ASTRO) (plenary 3).
Postoperative radiation also improved survival in N1 and N2 patients who did not receive adjuvant chemotherapy, although to a lesser extent than the striking benefits in patients with N2 disease who received chemotherapy. "Therefore, there is room for possible adjuvant radiation in N1 and N2 patients who cannot receive cisplatin-based adjuvant chemotherapy because of comorbidities," said Dr. Douillard, professor and head of medical oncology, Centre Rene Gauducheau, St. Herblain, France.
Dr. Douillard described a retrospective analysis of outcomes in the ANITA (Adjuvant Navelbine International Trialist Association) randomized trial of vinorelbine (Navelbine)/cisplatin chemotherapy. He was careful to point out that because this was a secondary analysis of nonrandomized treatment, the results are only descriptive and require replication. A European clinical trial of postoperative radiation in N2 disease is in the planning stages.
The primary result of the ANITA trial, reported in 2005, was an 8.6% overall increase in 5-year survival in patients with completely resected stage IB to IIIA NSCLC who received vinorelbine/cisplatin by random assignment vs a group only under observation. The ANITA study protocol neither required nor randomly assigned radiation therapy. Instead, it was recommended for patients with node-positive disease and provided at the discretion of each participating center, with the center committing to provide radiation or not for all patients before any were enrolled. The recommended dose was 45 to 60 Gy (2 Gy per fraction, 5 fractions per week) using a high-energy linear accelerator.
Of 840 clinical trial participants, 232 (27.6%) received postoperative radiation. It was used in only 8% of patients with node-negative disease, typically those with chest wall invasion. One-third of patients with N1 disease and about half with N2 disease received radiotherapy.
Although radiation therapy had a somewhat deleterious effect in the cohort as a whole, striking differences emerged when subgroups were analyzed according to nodal status and chemotherapy. In patients with N2 disease who received chemotherapy, median survival was 23.8 months; adding adjuvant radiation increased median survival to 47.4 months. In patients with N2 disease who did not receive chemotherapy, median survival was very poor, only 12.7 months, with surgery alone, but increased to 22.7 months with radiation, Dr. Douillard said.
In patients with N1 disease who received chemotherapy, median survival was 93.6 months. Adding radiation decreased median survival to 46.6 months a "clear deleterious effect," Dr. Douillard said. In N1 patients in the observation arm, median survival was 25.9 months without radiation and 50.2 months with radiation.
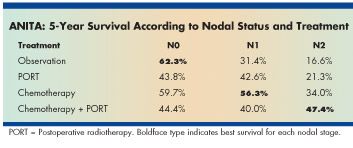
Five-year overall survival rates show the same trends, Dr. Douillard said (see Table). In patients with node-negative disease, survival was optimal with surgery alone (62.3%). In N1 disease, the best results occurred with chemotherapy alone (56.3%). In N2 disease, "surgery alone has a very poor outcome, with only 16% 5-year survival," Dr Douillard said. "The addition of radiation to surgery improves survival a little bit. Chemotherapy doubles 5-year survival. But the best results, with four cycles of vinorelbine/cisplatin chemotherapy followed by radiation, is 47.4% 5-year survival, which is quite good for patients with stage IIIA lung cancer," he said.