Recap: Experts at Mount Sinai Grapple With Best Practices in Multiple Myeloma
A panel of experts from Mount Sinai examines representative patient cases and reviews treatments in multiple myeloma.
At an Around the Practice® program hosted by CancerNetwork®, experts from Mount Sinai discussed a few emblematic patient cases in multiple myeloma, using them to illustrate the state of the disease more generally. The panel was led by Sundar Jagannath, MBBS, director of the Center of Excellence for Multiple Myeloma and professor of medicine at the Tisch Cancer Institute.
Panelists included Adriana Rossi, MD, assistant professor of medicine, and co-director of the CAR T and Stem Cell Transplant program at the Center of Excellence for Multiple Myeloma; Shambavi Richard, MD, associate professor of medicine at the Center of Excellence for Multiple Myeloma; and Joshua Richter, MD, associate professor of medicine at the Tisch Cancer Institute in the Division of Hematology and director of Multiple Myeloma at the Blavatnik Family Chelsea Medical Center.
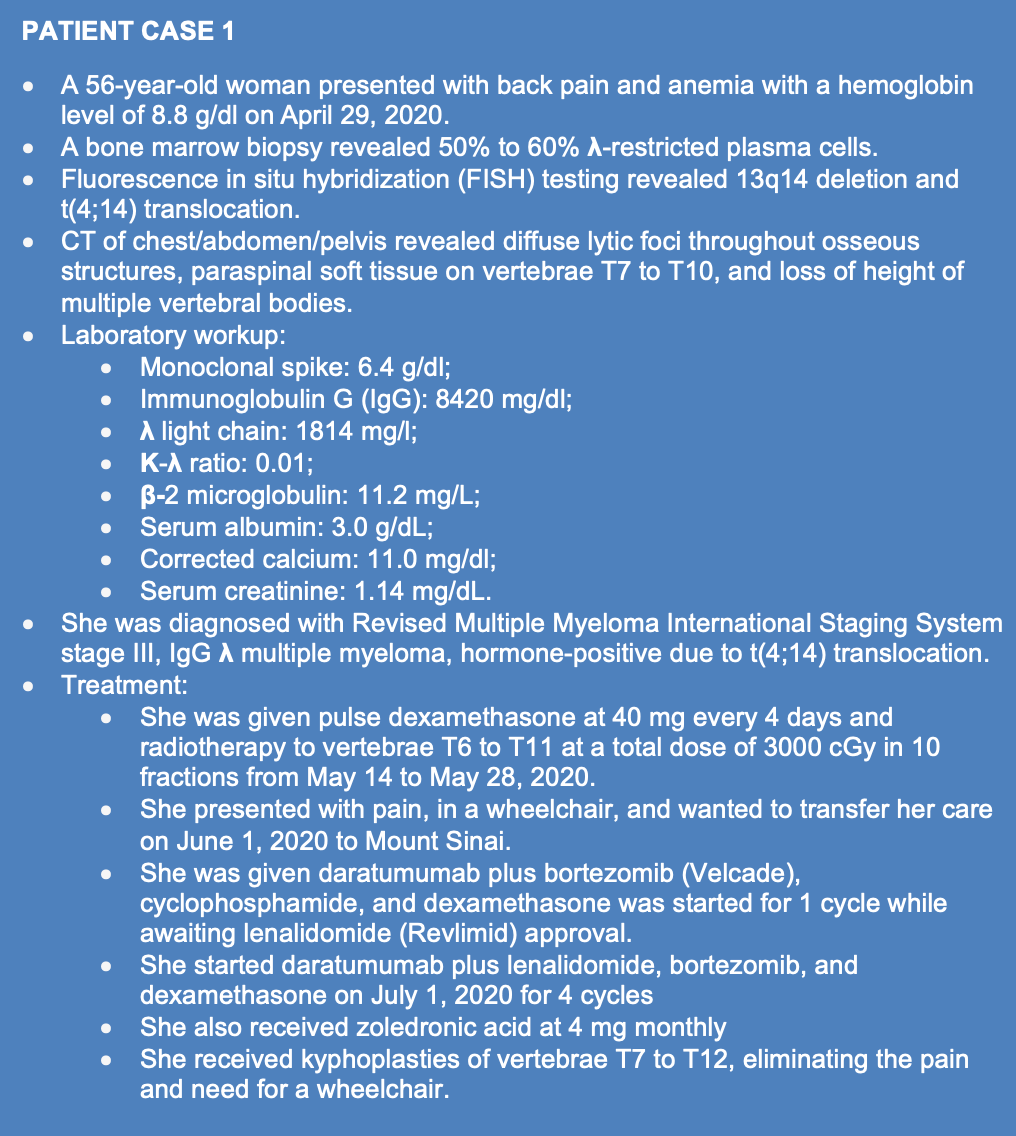
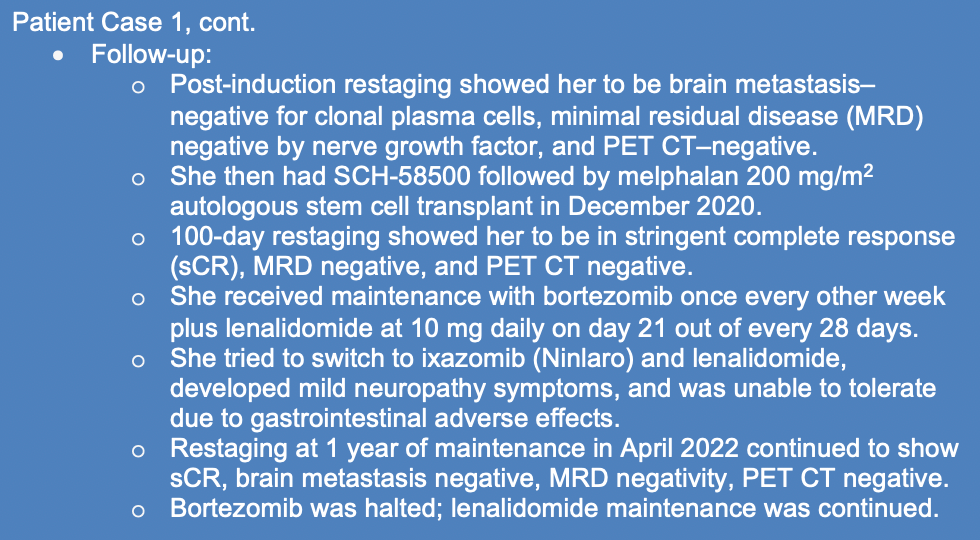
PATIENT CASE 1.


Jagannath: What were the key takeaways of the phase 3 DETERMINATION study [NCT01208662]?1
Richard: DETERMINATION [examined] a transplant vs non-transplant approach for the triplet induction therapy of lenalidomide [Revlimid], bortezomib [Velcade], and dexamethasone [RVd]. Patients in the transplant arm had 3 cycles of RVd and went on to stem cell harvest, and then the transplant was followed by 2 cycles of RVd consolidation and lenalidomide maintenance. Patients in the non-transplant arm had the 3 cycles of RVd and then [stem cell] harvest as well, and then went back on RVd treatment, receiving 5 cycles of consolidation. Then, they went on to lenalidomide maintenance. All patients received maintenance indefinitely until either progression or intolerance of the treatment.
The study’s analysis was [recently] updated, and at a median follow-up of 76 months, they had a median progression-free survival [PFS] of 67.6 months for the transplant arm as opposed to 46.2 months for the non-transplant arm. This translated to a hazard ratio of 0.45. The response rates were also considerably better for the transplant arm. Minimal residual disease [MRD]–negativity was seen in 52% of the transplant arm vs 37% of the non-transplant arm. Overall survival [OS], however, was not any different [between the arms], around 80% at about 5 years. DETERMINATION offered insight into the power of continuing lenalidomide maintenance to progression.
This compares very nicely with the phase 3 IFM 2009 study [NCT01191060].2 In that study, the design was the same [as DETERMINATION], except patients received lenalidomide maintenance for just 1 year. The median PFS was about 47 months for the transplanted arm vs about 35 months for the non-transplant arm.
[Through this comparison, we can see that] the continuation of lenalidomide to progression [in DETERMINATION] significantly improved PFS. Neither of these studies showed a difference in OS.
Jagannath: Do you administer lenalidomide continuously, without breaks?
Richard: I do find the tolerance for lenalidomide is a little better when patients get the week’s break. Of course, this question hasn’t ever been studied [directly], and many of the trials have used continuous maintenance. In general, I’ve tended to use a 3-weeks-on and 1-week-off schedule, and the patients have been able to stay on lenalidomide for long periods of time.
Jagannath: What were the results of the phase 2 GRIFFIN [NCT02874742] and phase 2 MASTER [NCT03224507] studies?3,4
Rossi: In GRIFFIN, patients received RVd induction therapy followed by transplant, consolidation, and maintenance lenalidomide. Daratumumab [Darzalex] was added to the regimen throughout all stages, and so the comparator arm was daratumumab-RVd [D-RVd] induction, transplant, D-RVd consolidation, and then daratumumab in the maintenance setting.
It was very encouraging to see the response rates deepen with time in the more mature data, and [the survival curves] continue to separate. [Additionally], those patients who sustained their MRD-negative status for 6 months all seem to have retained it through 12 months. That’s a very encouraging argument in favor of treating with daratumumab in all phases.
Richter: Data from the MASTER trial were presented recently by Luciano Costa, MD. In MASTER, patients received a quadruplet therapy as opposed to the D-RVd many clinicians administer. Patients received daratumumab plus carfilzomib [Kyprolis], lenalidomide, and dexamethasone [D-KRd], with carfilzomib as a substitute for bortezomib. Patients received 4 induction cycles, autologous stem cell transplant [ASCT], post-transplant consolidation with D-KRd, and, finally, lenalidomide maintenance.
At various time points, they assessed patients for MRD status, and those unable to maintain MRD negativity could stop therapy. [Patients were classified] into 3 categories: those with no high-risk cytogenetic abnormalities, those with 1 abnormality, and those with 2 or more.
Some interesting patterns emerged. One was that all groups seemed to improve their response over time. Those with 2 or more high-risk cytogenetics didn’t experience the same levels of MRD negativity [as the others], and those with 0 or 1 high-risk cytogenetic abnormalities, many of whom continued in remission.
Those with 2 or more high-risk cytogenetic abnormalities who halted therapy, even if they achieved MRD negativity, relapsed at a much higher rate. As such, MRD negativity is an important factor in clinical practice, but we also need to go a step further and examine the underlying disease.
Jagannath:What does the future of ASCT look like? Should it still be used in clinical practice?
Richard: Transplants are still a very important tool for treating newly diagnosed myeloma. They will remain the cornerstone of treatment until we have evidence that other modalities are more advantageous.
We have seen now, in both DETERMINATION and IFM 2009, that [ASCT makes] a clear difference regarding PFS. Granted, we haven’t seen OS data, which is the gold standard when evaluating the benefits of a therapy, but [patients with] myeloma now have a median OS of almost 10 years. There are also some novel treatments which are great at salvaging patients upon relapse. It’s therefore very difficult to associate an [additional] OS benefit [with ASCT specifically], but we shouldn’t underestimate the importance of the PFS benefit.
There are other trials, too; the phase 2 FORTE study [NCT02203643] clearly showed that KRd plus transplant is superior to KRd [without transplant].5 Again, this is a difference in PFS, corroborating the results from the other 2 studies.
However, we haven’t ever had a study comparing transplant and the new quadruplet therapies. If that’s going to be the standard of care, then we’ll have to reassess efficacy. The jury’s still out on that one. As of now, I still believe in transplants.
Jagannath: Would you recommend this to all patients? Would you try to talk a patient into transplant if they were hesitant?
Richard: I don’t believe in trying to talk patients into these therapies. They all carry some risks. There are issues only the patient understands, issues of logistics and personal preference. There’s always a dialogue [between patient and clinician]. Myeloma transplants are elective therapies because we have so many other great options [at our disposal].
If they ask me what they should do, I recommend the transplant. That’s it. I don’t push any further.
Rossi: I don’t think every patient needs a transplant. MASTER and other studies may eventually give us time points at which MRD negativity can be used for decision-making [on this question], but we’re not there yet. It’s still a strong part of our armamentarium.
If I were to administer a triplet therapy, it would be based on the FORTE data [favoring] the KRd. I don’t think I’ve used an RVd regimen at all this year.
When I do administer RVd, I tend to use it with daratumumab as a quadruplet therapy.
Jagannath: Should a patient’s response to induction therapy sway a clinician’s approach to treating with ASCT?
Richter: I try to take a uniform approach. I like to see at least a partial response [PR] to induction therapy, but PRs can mean different things for different patients. A PR could occur in someone who started with a monoclonal spike of 1 which reduces to 0.4. That’s a very different [case] than someone who started with a monoclonal spike of 6 which reduces to 2.7.
Therefore, I try to get my patients debulked, but upfront therapy is like a meal. There’s the appetizer, main course, and dessert; the induction is the appetizer, the transplant is the main course, and the maintenance is the dessert. I don’t want my patients to fill up on the bread and appetizer so much that they don’t reach the main course. I still believe in main courses—in transplants.
Having said that, if residual disease remains after the transplant, there are still things you can do to improve the response, though many of these aren’t as popular in the United States. Both MASTER and the phase 3 HOVON-65/GMMG-HD4 trial examined post-transplant consolidation.6
After transplant, I categorize [tumor] cells into 3 groups: those that you killed, those that you could never kill, and those that are ‘stunned,’ so to speak. If you hit these cells again at the right time [post-transplant], you can achieve a deeper remission and squeeze a better response out of the treatment.
Jagannath: I take a completely different approach because I’ve been conducting transplants since 1989. There was even a time when we tried using purified stem cells.
When I use D-RVd, I administer the treatment for at least 6 cycles. Most of these patients are in a CR, or are MRD negative because their collected stem cells contain very few tumor cells. I continue [for 6 cycles] rather than stopping after 3 or 4 because clinical trials are performed this way, but there’s no rationale [for this] when there’s a response. Why can’t you achieve the maximum response, and then stop lenalidomide at 4 cycles? [In that case], having stopped lenalidomide, I would continue to give bortezomib and dexamethasone plus daratumumab, as well as bortezomib, cyclophosphamide, and dexamethasone, or carfilzomib and dexamethasone [Kd] plus daratumumab to ensure a continuing, deeper response. Once I can collect data monthly, I collect stem cells.
The objective is to get the maximum value out of the treatment plan. Otherwise, you have to plan post-transplant consolidation.
Richard: The evidence for consolidation has always been highly debated. There’s no absolute standard. I don’t tend to use consolidation; I try to maximize my induction.
[However], I might use it in a couple specific situations. I might use it for a high-risk patient who’s still MRD-positive post-transplant. We all know the predictive power of achieving MRD negativity, especially post-transplant, so I might try a few cycles of consolidation or intensification to achieve that prior to maintenance.
Notably, the phase 3 StaMINA trial [BMT CTN 07LT; NCT02322320] examined patients who had a single transplant, and randomized them to proceed to either maintenance, a tandem transplant and then maintenance, or 4 cycles of RVd, consolidation, and then maintenance.7 At the 3-year mark, there wasn’t much of a difference in PFS, overall survival, or [otherwise]. However, after extended follow-up, especially when teasing out the high-risk patients, the tandem transplant was best, followed by the consolidation-and-then-maintenance group. Those who proceeded directly to maintenance [had the worst outcomes].
[As such], there’s probably room for consolidation someplace, but I wouldn’t use it for every patient. If I have a standard-risk patient who easily achieved MRD negativity post-transplant, [for example], I wouldn’t use consolidation.
PATIENT CASE 2.
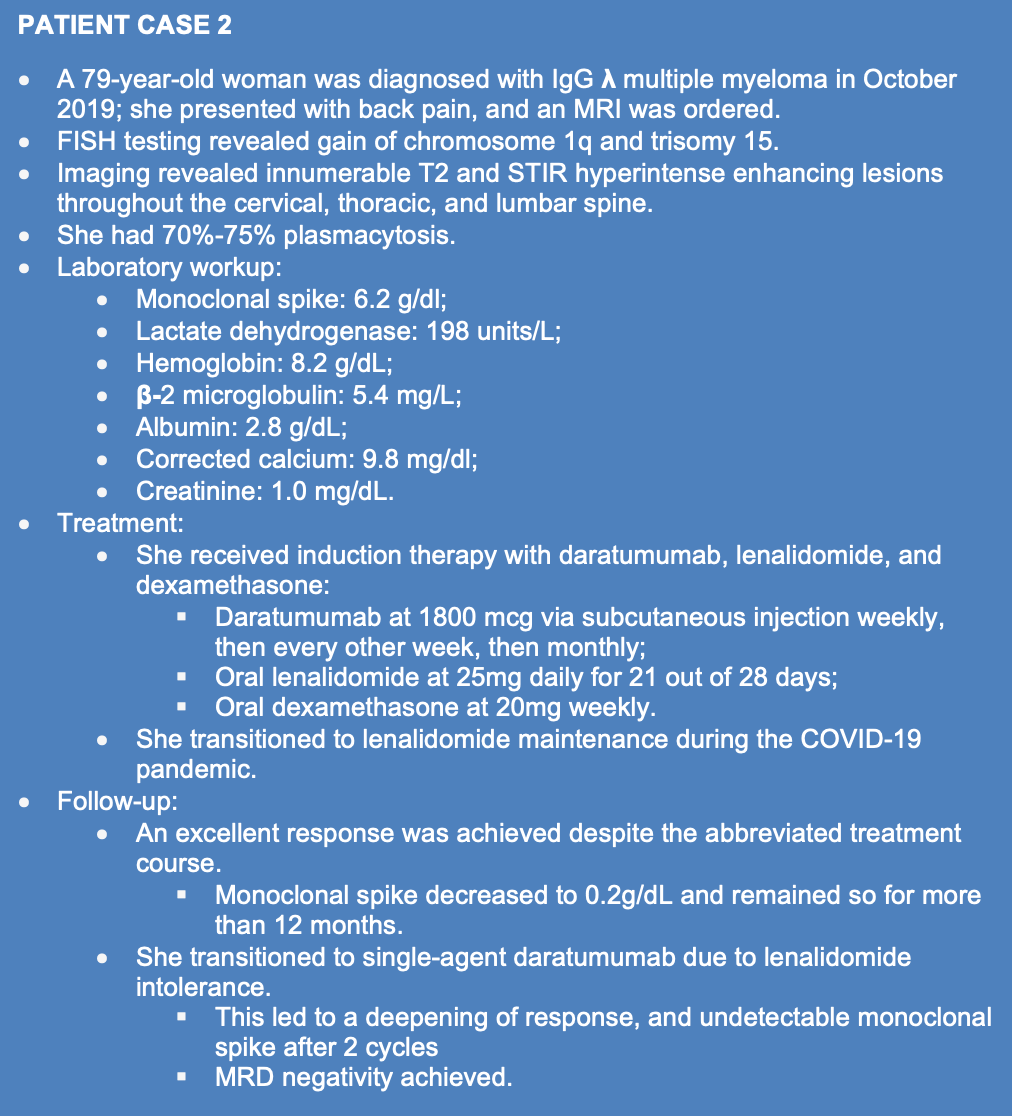

Jagannath:How do you decide between quadruplet therapy, triplet therapy, or a 2-drug combination in transplant-ineligible patients aged 75 years old or older?
Rossi: Age is just a number. I have frail patients who are very young, and I treat them very cautiously.
This patient is robust, even at age 79, but she has a long-standing history of diabetes. For her, concerns about neuropathy would preclude me from using up front bortezomib. For many patients, especially those with higher-risk features or more aggressive disease, I could tolerate starting with a quadruplet, [but] I don’t commit to it long term. It’s [often effective] to start a quadruplet, get through 1 or 2 cycles, and then either reduce the dosage or drop a drug entirely from the combination for tolerability.
Jagannath: In older patients, do you check bone marrow for MRD every year, or at fixed intervals, as is the standard in transplant-eligible or younger patients?
Rossi: I offer [regular checks] to those patients, [but] I don’t talk them into anything. When they appreciate what it could mean, that it could translate to being off therapy, [they often agree].
During the COVID-19 pandemic, [instead of] relying strictly on the evidence, [we were] doing what we could and learning lessons from our experience. This patient didn’t have an interim biopsy. Other than her diagnostic biopsy, her first biopsy was for MRD negativity once she attained the CR. But yes, I’ll offer it to her next year, if she’s still with me.
Jagannath: Can you tell me about the phase 3 MAIA study [NCT02252172] in this patient population?8
Rossi: MAIA is the basis for this patient’s treatment. MAIA examined what was considered a standard of care—lenalidomide and dexamethasone—with or without upfront daratumumab in transplant-ineligible patients. Unsurprisingly, the triplet performed better than the doublet, not only in terms of overall response but also in terms of MRD negativity.
Jagannath:How would you compare MAIA to the phase 3 SWOG-S0777 [NCT00644228] trial?9
Rossi: Our 2 primary triplets [in this disease] are remarkably similar in terms of PFS and other outcomes.
Bortezomib, [the drug examined in SWOG-S0777], is difficult, often causing neuropathy. We’re not able to treat peripheral neuropathy very well, so that’s a large consideration.
We have much data on proteosome inhibitors in [patients with] high-risk cytogenetics. As data mature, the daratumumab data will be very similar; either triplet will get you a similar response. It’s mostly [a matter of] mitigating toxicity and finding a regimen these patients can sustain.
Jagannath: How do you select doublet vs triplet [therapy] for older patients?
Richter: We don’t use classical chemotherapy. In the age of novel therapies, I give most of my patients the triplet, and I’d rather give them a dose-adjusted triplet as opposed to a full-dose doublet. In this context, lenalidomide plus dexamethasone became the standard [in the United Kingdom], and bortezomib, melphalan [Evomela], and prednisone became the standard [elsewhere] after some of the older trials, like the phase 3 VISTA study [NCT00111319].10 The phase 3 ALCYONE trial [NCT02195479] examined daratumumab plus bortezomib, melphalan, and prednisone.11
[Clinicians in] Europe usually give quadruplet [therapy] to patients who are older and transplant-ineligible older. [If it’s] properly dose adjusted, I’d rather give 15 mg of lenalidomide and 12 mg or 20 mg of dexamethasone alone with daratumumab or bortezomib, rather than 25 mg and 40 mg, respectively. That’s because of the multiple subclones of myeloma. You can pick off more with multiple mechanisms of action; you can achieve a deeper remission and better outcomes.
In terms of treatment selection, we have to consider frailty. One of my old professors used to say: if we walk into the room and the patient has the eye of the tiger, we give them a full regimen. If they don’t have the eye of the tiger, we don’t. There are some wonderful people doing research into this, such as our colleague Larysa J. Sanchez, MD, who’s examining formal assessments of frailty [including] the European Organization for the Research and Treatment of Cancer Quality of Life Questionnaire [EORTC QLQ-C30], in addition to tests you can perform in the clinic like the 4-minute walk test.
Jagannath:In this older-patient population, what are your objectives?
Richard: Older patients differ greatly from younger patients. Toxicity management is very important. Older [patients] feel the toxic effects [more] and cannot weather toxicities as well. In addition to the goal of achieving their best response—ideally, MRD negativity—we have to keep an eye on toxicity.
[However, disease reduction is still paramount]. It’s especially important in older patients for 2 reasons. Firstly, they don’t do as well [as younger patients] with disease, and you have to intensify treatment to eliminate the disease [as quickly as possible]. They [also] don’t do well when they relapse; there’s a high attrition rate. Not every older patient is going to reach the second-line novel therapy that works so well for younger patients. [Therefore], I aim for the deepest response possible, ideally MRD negativity, [in the first line].
Jagannath: In older patients, do you follow the same principle [as you do in younger patients]? Do you use maintenance therapy indefinitely, if possible?
Richard: In the MAIA trial, the goal was to give daratumumab, lenalidomide, and dexamethasone [DRd] until progression. That [included] a hefty dose of lenalidomide for someone who’s 85 years old. I don’t know if many 85-year-olds could tolerate 25 mg of lenalidomide.
Overall, if we want to mimic the results from MAIA in our clinic, treating to progression is something we have to consider. [However], we may have to adjust the dosage as we go; it depends. It has to be tailored to the patient because not every older patient is the same. How well they tolerate treatment will be demonstrated as we go along with the regimen.
My rule of thumb is to continue to progression. Having said that, if a patient is not tolerating the regimen well, experiences a great response, and needs a little break, nothing is off the table.
Jagannath:How do you define high-risk disease in older patients, and how do you tailor therapy for high-risk patients?
Rossi: There are 2 ways of thinking about this. Cytogenetic testing is a very helpful tool but doesn’t give us the whole story. The most useful data is the patient’s [individual] response to therapy. The patient [outlined in Case 2] had substandard treatment, didn’t receive all the planned therapy, and still managed to have a very good response. That’s why I thought she was an appropriate [candidate] for single-agent maintenance.
But for those with high-risk disease, whether it’s defined by cytogenetics, lack of response, or early relapse, I’d probably continue [treatment] at lower doses—maybe with a less intensive schedule, but [still] a combination. If [their frontline treatment was] DRd, this would consist of continuing the daratumumab and lenalidomide. If it was RVd, [it would consist of] continuing with a lower dose of the bortezomib.
Jagannath: Would age change your choice of therapy?
Rossi: I try to look beyond age. We just had an 82-year-old, whom I’m taking to chimeric antigen receptor [CAR]–T cell therapy, and another who’s 72 years old, whom I didn’t feel would tolerate that therapy. [The crucial factor] is fitness, [not age]. If a patient is frail, I lean toward a triplet therapy and a more robust dose regardless of age. If I think they can tolerate the first cycle of a quadruplet therapy, I usually start with the quad and peel back as needed.
Jagannath: How long would you continue treatment on that quadruplet regimen?
Rossi: [I’d continue until] best response or tolerability. Most patients don’t get beyond 4 cycles before I’m comfortable peeling away [by] either [removing] a drug or [reducing] the frequency of therapy.
Jagannath: Given you often only have one chance with older patients, you wouldn’t follow the quad to the 1-year mark or until a deep response?
Rossi: [The important thing is] toxicity in older patients—their quality of life.
Jagannath: What if the patient didn’t have much toxicity?
Rossi: Without toxicity, you can keep going to the best response or intolerable toxicity, but most of my older patients hit a quality-of-life barrier. It’s easier to give [prolonged treatment] to younger, fitter patients, who tend to tolerate it for longer.
Jagannath: In an 85-year-old patient, what would your choice of therapy be?
Richter: One big difference between the designs of the SWOG-S0777 and MAIA trials is that in S0777, the triplet [therapy] was halted, and the patients proceeded onto lenalidomide. In MAIA, the triplet therapy was given continually. Giving [patients] more robust therapy for longer durations improves outcomes.
[However], I temper this with a great phase 3 study [NCT02215980] published by Alessandra Larocca, MD, PhD, and colleagues [examining the efficacy and safety of dose reductions in elderly and unfit patients with newly diagnosed multiple myeloma].12 As opposed to giving lenalidomide and dexamethasone [Rd] continuously, they gave patients Rd followed by lenalidomide maintenance. This was 9 months of full-dose Rd, and then patients dropped the dexamethasone and went onto lenalidomide maintenance.
Even before that study, when we used to give lenalidomide and daratumumab, we would give it 4 days on, 4 days off. I like to give DRd, and then, perhaps after 9 months, continue the regimen [with a reduced] lenalidomide dose.
References
- Richardson PG, Jacobus SJ, Weller E, et al. Lenalidomide, bortezomib, and dexamethasone (RVd) ± autologous stem cell transplantation (ASCT) and R maintenance to progression for newly diagnosed multiple myeloma (NDMM): the phase 3 DETERMINATION trial. J Clin Oncol. 2022;40(17 suppl):LBA4. doi:10.1200/JCO.2022.40.17_suppl.LBA4
- Attal M, Lauwer-Cances V, Hulin C, et al. Lenalidomide, bortezomib, and dexamethasone with transplantation for myeloma. N Engl J Med. 2022;376:1311-1320 doi:10.1056/NEJMoa1611750
- Voorhees PM, Kaufman JL, Laubach J, et al. Daratumumab, lenalidomide, bortezomib, and dexamethasone for transplant-eligible newly diagnosed multiple myeloma: the GRIFFIN trial. Blood. 2020;136(suppl 8):936-945. doi:10.1182/blood.2020005288
- Costa LJ, Chhabra S, Medvedova E, et al. Daratumumab, carfilzomib, lenalidomide, and dexamethasone with minimal residual disease response-adapted therapy in newly diagnosed multiple myeloma. J Clin Oncol. 2022;40(25):2901-2912. doi:10.1200/JCO.21.01935
- Gay F, Musto P, Rota-Scalabrini D, et al. Carfilzomib with cyclophosphamide and dexamethasone or lenalidomide and dexamethasone plus autologous transplantation or carfilzomib plus lenalidomide and dexamethasone, followed by maintenance with carfilzomib plus lenalidomide or lenalidomide alone for patients with newly diagnosed multiple myeloma (FORTE): a randomised, open-label, phase 2 trial. Lancet Oncol. 2021;22(12):1705-1720. doi:10.1016/S1470-2045(21)00535-0
- Goldschmidt H, Lokhorst HM, Mai EK, et al. Bortezomib before and after high-dose therapy in myeloma: long-term results from the phase III HOVON-65/GMMG-HD4 trial. Leukemia. 2018;32(2):383-390. doi:10.1038/leu.2017.211
- Hari P, Pasquini MC, Stadtmauer EA, et al. Long-term follow-up of BMT CTN 0702 (STaMINA) of postautologous hematopoietic cell transplantation (autoHCT) strategies in the upfront treatment of multiple myeloma (MM). J Clin Oncol. 2020;38(15 suppl):8506. doi:10.1200/JCO.2020.38.15_suppl.8506
- Ruan J, Leonard JP, Chen GZ, et al. Daratumumab plus lenalidomide and dexamethasone (D-Rd) versus lenalidomide and dexamethasone (Rd) alone in transplant-ineligible patients with newly diagnosed multiple myeloma (NDMM): updated analysis of the phase 3 MAIA study. Blood. 2022;140(suppl 1):10150-10153. doi:10.1182/blood-2022-163335
- Durie BGM, Hoering A, Sexton R, et al. Longer term follow-up of the randomized phase III trial SWOG S0777: bortezomib, lenalidomide and dexamethasone vs. lenalidomide and dexamethasone in patients (pts) with previously untreated multiple myeloma without an intent for immediate autologous stem cell transplant (ASCT). Blood Cancer J. 2020;10(5):53. doi:10.1038/s41408-020-0311-8
- San Miguel JF, Schlag R, Khuageva NK, et al; VISTA Trial Investigators. Bortezomib plus melphalan and prednisone for initial treatment of multiple myeloma. N Engl J Med. 2008;359(9):906-917. doi:10.1056/NEJMoa0801479
- Mateos MV, Cavo M, Blade J, et al. Overall survival with daratumumab, bortezomib, melphalan, and prednisone in newly diagnosed multiple myeloma (ALCYONE): a randomised, open-label, phase 3 trial. Lancet. 2020;395(10218):132-141. doi:10.1016/S0140-6736(19)32956-3
- Larocca A, Bonello F, Gaidano G, et al. Dose/schedule-adjusted Rd-R vs continuous Rd for elderly, intermediate-fit patients with newly diagnosed multiple myeloma. Blood. 2021;137(22):3027-3036. doi:10.1182/blood.2020009507
EP: 1.Patient Case 1: A 54-Year-Old Woman With Transplant-Eligible NDMM
EP: 2.Induction Regimens in Transplant-Eligible NDMM: Clinical Trial Data
EP: 3.What is the Role of Transplant in Newly Diagnosed Multiple Myeloma?
EP: 4.Post-Transplant Therapy in NDMM: Consolidation and Maintenance Therapy
EP: 5.Patient Case 2: A 79-Year-Old Woman With Transplant-Ineligible NDMM
EP: 6.Induction Therapy Options for Patients With Transplant-Ineligible NDMM
EP: 7.Transplant-Ineligible NDMM: Optimizing Selection and Duration of Therapy
EP: 8.Treating High-Risk Transplant-Ineligible Newly Diagnosed Multiple Myeloma
EP: 9.Patient Case 3: A 65-Year-Old Woman With Relapsed Multiple Myeloma
EP: 10.Practical Factors in Selecting Therapy for Relapsed/Refractory MM
EP: 11.Future Directions: Novel Targeted Therapies in Multiple Myeloma
EP: 12.Multiple Myeloma Management: Addressing Disparities in Care
EP: 13.Recap: Experts at Mount Sinai Grapple With Best Practices in Multiple Myeloma
Navigating AE Management for Cellular Therapy Across Hematologic Cancers
A panel of clinical pharmacists discussed strategies for mitigating toxicities across different multiple myeloma, lymphoma, and leukemia populations.