Strategies for Overcoming Disparities for Patients With Hematologic Malignancies and for Improving Enrollment on Clinical Trials
A multitude of factors contributes to cancer disparities. Addressing these disparities among racial/ethnic minority populations with blood cancers requires multilevel models of the interactions between relevant factors and the performance of translational research that uses knowledge of cancer biology to develop and test the feasibility of interventions that can impact human endpoints. To be effective, efforts should be made to advance these research findings to applications that can transform clinical practice and health care delivery. We reviewed the literature to define a framework for overcoming disparities for patients with hematologic malignancies and to improve patient enrollment in clinical trials.
Williams is a hematology/oncology fellow at The University of Texas MD Anderson Cancer Center.

McNeill is chair of the Department of Health Disparities Research at The University of Texas MD Anderson Cancer Center.

Hildebrandt is an associate professor at The University of Texas MD Anderson Cancer Center.

is a clinical research coordinator at the Emory University School of Medicine.

Flowers is chair of the Department of Lymphoma/Myeloma at The University of Texas MD Anderson Cancer Center.

Background
A multitude of factors contribute to cancer disparities, including, but not limited to, differences in diet, lifestyle, environmental exposures, cultural beliefs, genetic and biological factors related to ancestry, socioeconomic status (SES), and access to health care. More investigation is needed in evaluating these factors in less common cancers and hematological malignancies. Addressing disparities in cancer incidence, prevalence, burden of disease, mortality, and survivorship that have been documented among racial/ethnic minority populations with blood cancers will require multilevel models of the interactions between relevant factors and performance of translational research that uses knowledge of cancer biology to develop and test the feasibility of interventions that can impact human end points. Such work must address a wide range of research areas, including prevention, early detection, diagnosis, treatment, epidemiology, cancer control, treatment, and survivorship. To be effective, efforts should be made to advance these research findings to applications that can transform clinical practice and health care delivery. We reviewed the literature to define a framework for overcoming disparities for patients with hematologic malignancies and to improve patient enrollment on clinical trials.
A Patient Example
A 47-year-old African man moved from Kenya to the United States to find work, having to leave his family behind. In the months after moving, he developed progressive fatigue, general malaise, and right upper quadrant abdominal pain that prompted a visit to the county hospital’s emergency department. His work-up revealed an initial CD4 count of 6 and an HIV viral load nearing 1 million copies, while his CT scan showed more than 20 subcentimeter lesions within the liver. Unfortunately, because of lack of insurance, it took approximately 1 month to establish an interventional radiology appointment, and yet another month to finally biopsy one of the liver lesions. The results of the biopsy revealed diffuse large B-cell lymphoma (DLBCL), germinal center B-cell–like type without BCL-2, BCL-6, or MYC rearrangements. He was started on treatment 2 weeks after the diagnosis. Given that his lymphoma was related to underlying HIV, he was given aggressive chemotherapy in the form of dose-adjusted rituximab (Rituxan), etoposide, prednisone, vincristine, cyclophosphamide, and doxorubicin.1 This treatment typically involves inpatient admission every 3 weeks, but given limited hospital bed availability in the chemotherapy unit and difficulty with patient transportation to his scheduled appointments, there were multiple delays and reduced adherence to this timeline. Despite displaying both clinical and radiological evidence of improvement, the patient inexplicably stopped coming to his lab and clinic appointments. By the time cycle 4 was due of his planned 6 cycles, he was no longer reachable via telephone or letter. The reason for his decision to stop treatment remains unclear.
This patient’s situation highlights multiple disparities in health care delivery and cancer care that exist within a resource-limited setting. First, we see that patients without insurance often experience a delay in diagnosis. The delay in biopsy led to significant anxiety and frustration for the patient, even before starting treatment. Next, we see how the lack of beds in the chemotherapy ward of an underresourced hospital negatively impacted timely administration of chemotherapy. Coupled with the lack of social support, financial constraints, and the emotional burden of his underlying malignancy in a system with limited resources, the timeliness of delivering potentially curative therapy and the outcome for this patient were challenged. His opportunities to participate in observational studies and therapeutic clinical trials were also limited.
Disparities in Hematologic Malignancies
The National Cancer Institute (NCI) defines cancer disparities as differences in cancer measures (including incidence, prevalence, number of cancer cases, cancer-related deaths, and cancer-associated health complications) across population groups. Observed differences in cancer outcomes are often described in medically underserved populations, including racial and ethnic minorities and individuals with lower SES and lower health literacy.2 The Minority Health and Health Disparities Research and Education Act declared that a population experiences a health disparity “if there is a significant disparity in the overall rate of disease incidence, prevalence, morbidity, mortality, or survival rates in the population as compared with the health status of the general population.”3 Our review will focus on defining, summarizing, and suggesting strategies to overcome these disparities in patients with hematologic malignancies, with a specific focus on clinical research.
According to the American Cancer Society (ACS), there will be an estimated 1,806,590 newly diagnosed cancer cases and an estimated 606,520 cancer deaths in the United States in 2020. Of these new cancer diagnoses, approximately 178,522 will be in patients with hematologic malignancies, including lymphoma (~85,270 new cases; 20,910 deaths), multiple myeloma (~32,270 new cases; 12,830 deaths), and all forms of leukemia (~60,530 new cases; 23,000 deaths).4 Despite these numbers, data regarding racial differences in patients with hematologic malignancies are more limited than in those with solid tumors. To address this, Kirtane et al5 published a review examining the racial and ethnic disparities in incidence, survival, and outcomes across patients with various hematologic malignancies, as described below.
An analysis of 39,000 patients in the Surveillance, Epidemiology, and End Results (SEER) database from 1999 to 2008 showed that black and Hispanic patients with acute myeloid leukemia (AML) had increased risk of death by 12% and 6%, respectively, compared with non-Hispanic whites. This observation occurred despite the higher prevalence of favorable cytogenetics and younger age at diagnosis among the minority groups.6 Another analysis of the SEER database for patients with multiple myeloma revealed that novel myeloma therapies disproportionately benefited white patients of higher SES.7 After the introduction of these novel therapies, white patients had double the observed survival improvements compared with black patients. For example, controlling for sociodemographic factors, black patients with multiple myeloma in the United States were 21% less likely to be treated with bortezomib, an effective agent used during that treatment era.8
Disparities in incidence, age at diagnosis, and survival rates have also been identified for Hodgkin lymphoma (HL) and non-Hodgkin lymphoma (NHL) subtypes.5,9-13 In one study, patients with HL in the lowest SES category had a 64% increased risk of death related to HL compared with those in the highest SES category.14 Among adolescent and young-adult patients with NHL, blacks and Asian/Pacific Islanders were more likely to be given a diagnosis at a later stage than other groups.15 For patients with DLBCL diagnosed between 1992 and 2005, racial differences in survival varied according to stage.16 For stage I disease, non-Hispanic whites had the best 5-year survival rate (67%), whereas blacks had the worst (60%). Asian/Pacific Islanders had the worst survival rate for stage IV disease (35%), and non-Hispanic whites had the best survival rate (41%). In other studies, black patients received a diagnosis at a mean age more than 10 years younger than whites, and they more commonly had advanced-stage disease.17 Furthermore, these patients were less likely to be insured, less commonly received standard-of-care therapy, and experienced worse overall survival (OS).15-17
Across leukemias, multiple myeloma, and lymphomas, there are also racial disparities seen in hematopoietic cell transplantation (HCT). Given that HCT requires numerous resources to be both safe and effective, HCT can be associated with disparities in access and outcomes for minority populations. Analysis of the California Cancer Registry found that black and Hispanic patients with AML had a decreased likelihood of stem cell transplantation compared with white patients (odds ratio [OR], 0.64; 95% CI, 0.46-0.87; vs OR, 0.74; 95% CI, 0.62-0.89, respectively).9,18 SEER-Medicare data revealed that age-adjusted relative rates of autologous HCT for patients with myeloma were significantly higher in non-Hispanic whites than in blacks, Hispanics, and Asians.10,19 In another myeloma study, black patients were found to be 49% less likely to receive stem cell transplantation than white patients.11
Ancestry and Disparities
With the established differences in incidence, clinical features, and outcomes by race for many hematologic malignancies, there is increased interest in understanding the role of genetic factors and genetic ancestry in influencing differences among populations. Genome-wide association studies (GWAS) have identified common germline genetic variations associated with susceptibility to lymphomas, leukemias, and multiple myeloma, primarily in populations of European descent.12-38 GWAS studies in other population groups are slowly emerging and are enabling investigation into shared and unique genetic risk factors. For example, analysis of GWAS data from African Americans identified stronger loci for several of the established susceptibility regions for multiple myeloma, while failing to replicate several of the other regions identified in populations of European descent.35,39 Similarly, studies of DLBCL susceptibility loci in Asian populations have found shared and race-specific associations.36-41 However, larger genetic studies are needed in more diverse populations to continue to identify the genetic basis of disparities. Currently, there is a lack of genome-wide genetic studies in Hispanics for adult hematologic malignancies, leaving a gap in our understanding of this rapidly growing patient population.
A small number of analyses based on genetic ancestry of patients, instead of self-reported ancestry, have been conducted to better define the role of genetics and disparities. In an analysis of survival following allogenic stem cell transplant, increased African ancestry in the recipient increased risk of overall mortality by more than 2-fold (HR, 2.26; 95% CI, 1.28-3.96) and increased by 3.3-fold (HR, 3.09; 95% CI, 1.7-5.64) for increased levels of African ancestry in the donor. These increased risks were independent of clinical variables, and most striking, independent of self-reported race/ethnicity.38,42 Multiple myeloma is the most frequent hematologic malignancy diagnosed in blacks. In genetic ancestry analyses, specific subtypes—(11;14), t(14;16), and t(14;20)—were more frequent in individuals with higher degrees of African ancestry, while other cytogenetic abnormalities, such as trisomies and monosomy 13/13q deletion, were less prevalent.39,43 For DLBCL, analysis has shown that recurrent somatic mutations in known driver genes (ATM, MGA, SETD2, TET2, DNMT3A, and MLL3) were more common in patients with African ancestry, and that the spectrum of mutations differed from that in patients of European ancestry.40 Together, these studies provide evidence that many of the observed disparities in incidence, clinical features, and outcomes among hematologic malignancies may have a genetic underpinning. Future research in this area will be necessary to fully elucidate these relationships.
Disparities by Insurance Status
Understanding how genetic factors influence cancer outcomes among different patient populations is one basis for health disparities research. Other key components for evaluation include residence, education level, SES, and insurance status. The National Cancer Database (NCDB) is a national oncology database across more than 1500 facilities accredited by the Commission on Cancer that includes information on more than 70% of newly diagnosed cancer cases. This database helps record patient-specific factors important in disparities research. Studies utilizing the NCDB have shown that patients without insurance commonly experience a delay from symptom onset to diagnosis.41 This delay affects the nearly 27.5 million Americans (8.5%) who were uninsured as of 2018. While the Affordable Care Act established in January 2014 has significantly improved the percentage of insured Americans, Hispanics and blacks continue to be the most likely to be uninsured (18% and 10%, respectively); for non-Hispanic whites, the rate is 5%.4 Without insurance, minority patients often lack access to optimal health care, leading to delayed diagnosis, delayed treatment initiation, and disparities in OS.
In 2014, the ACS published a study linking lack of insurance with inferior survival rate among patients with DLBCL. Using the NCDB, authors analyzed approximately 4000 patients with DLBCL in 2004, categorized into those with private insurance, Medicaid, or no insurance. Of note, many of the patients involved in this study enrolled in Medicaid after their diagnosis of DLBCL. Approximately 80% of the full cohort had private insurance (higher than the general insurance rate among Americans at that time), 10% were uninsured, and 10% had Medicaid insurance. The uninsured and Medicaid patients were, on average, younger, more likely to be members of a racial/ethnic minority, receive a diagnosis at an advanced stage, and less likely to receive standard-of-care chemoimmunotherapy. After controlling for sociodemographic factors but not adjusting for prognostic factors or specific treatment, this study found that uninsured patients and Medicaid-insured patients with DLBCL had a lower survival rate compared with those with private insurance (HR, 1.39, vs HR, 1.48, respectively). The OS rates at 5 years’ follow-up for privately insured, Medicaid‐insured, and uninsured patients were 75%, 64%, and 66%, respectively. The authors postulated that uninsured patients had inferior OS rates because of more advanced-stage disease at diagnosis, less use of standard-of-care chemoimmunotherapy, and scarce enrollment on clinical trials.41 The association between insurance status and OS in other lymphoma subtypes has been studied as well. Utilizing the NCDB for patients with follicular lymphoma (FL) and Burkitt lymphoma, those without insurance or with Medicare or Medicaid had significantly worse OS rates when compared with patients with private insurance.42,43 Even worse, a large national cohort study published in 2012 showed that uninsured patients with DLBCL were less likely to receive any treatment at all.44
Disparities in Rural and Lower-SES Patients
Authors of past studies have argued that patients’ zip codes may supersede their genetic codes when it comes to access to quality health care.45 To test this concept as it relates to lymphoma outcomes, Ritter et al investigated the influence of a patient’s residence and household income on OS. Using the NCBD, the authors examined 83,000 patients with DLBCL and 43,000 patients with FL based on geographic population density (rural, urban, or metropolitan). Rural was defined as a county with a population less than 2500; urban, a county with a population of at least 2500 that does not meet criteria for a metropolitan area based on the United States Department of Agriculture Office of Management and Budget parameters; and metropolitan, a county with at least 1 densely settled urban area with a population of at least 50,000. In the Ritter study, 1.7% of patients lived in rural areas, 13.1% in urban areas, and 85.2% in metropolitan areas (population percentages that reflect the general population).
When controlling for other patient demographic information, there was a significant decrease in OS for both rural and urban populations compared with metropolitan populations with DLBCL (HR, 1.09, vs HR, 1.08, respectively) and FL (HR, 1.2 vs HR, 1.11). Both urban and rural patients were less likely to have private insurance and were more likely to fall into the low SES class. Furthermore, those with household income less than $38,000 had an inferior survival rate (HR, 1.22).46 The results highlight that although patients from rural populations comprise a significant percentage (approximately 14.9%) of the United States, they may often face more obstacles to ideal health care than their metropolitan area–based counterparts.47
Barriers to Minority Enrollment on Clinical Trials
Clinical trials are key components of cancer research and continually enhance treatment options for patients across all tumor types. However, fewer than 5% of adult patients with cancer in the United States are estimated to enroll on cancer clinical trials, while about 70% of Americans are willing to participate.48,49 In an analysis by the ACS Cancer Action Network and Unger et al, the overall trial participation rates average 15.9% at academic centers and 7% at community centers.50 Unfortunately, in both kinds of settings and across most studies, African Americans, Hispanics, and patients older than 65 years were underrepresented on clinical trials, as were patients from urban/rural communities, who had limited access to them.
Many reasons have been proposed for this situation, including both structural (absence of available clinical trials based on tumor type and stage) and clinical (patient eligibility) barriers.50 The largest obstacles to enrollment on trial for rural patients seem to be both the physical distance and the lack of communication between large centers and small clinics, ultimately leading to unfamiliarity with clinical trial opportunities. This indicates a need to examine and address recruitment barriers by catchment area. Two examples of assessing disparities in patients with hematological malignancies for a catchment are described below.
Sample Catchment Area Results on Cancer Disparities for Applying Strategies Locally
While documentation of cancer disparities has mostly occurred at the national level, successful implementation of strategies to overcome disparities are likely to be more successful when they are customized to the local environment. This requires an assessment of disparities in a local cancer catchment area. We provide 2 examples that can be replicated to address disparities that exist for hematological and other cancers.
Georgia
An estimated 50,000 residents of the state of Georgia receive a new cancer diagnosis annually, and more than 16,000 Georgians succumb to cancer each year; the leading causes of these deaths are lung, breast, colon, and pancreatic cancers. Georgia residents experience disparities in cancer incidence and cancer outcomes for several malignancies as compared with national outcomes. In addition, disparities in outcomes also exist within the state, both among specific ethnic and racial groups, and based on factors related to geography and socioeconomic status. A 2019 Emory University study analyzed all NHL cases diagnosed in Georgia from 2001 to 2015 using the Surveillance, Epidemiology, and End Results (SEER) database, to better classify racial disparities found among patients with NHL in the state.51 Results indicated that the age-adjusted incidence rate for NHL in Georgia increased 1.03% per year for all patients.
However, African American patients had a higher annual percent change (APC) in NHL incidence when compared with whites (APC, 1.72 vs 0.84, respectively). This results also revealed racial disparities when analyzing different characteristics of disease presentation within DLBCL and FL subtypes. African American patients with DLBCL or FL received a diagnosis at a younger age and were more likely to present with B symptoms when compared with white patients with DLBCL or FL. Furthermore, African American patients with DLBCL were more likely to present with advanced-stage disease. Not only did African American patients with DLBCL and FL have differing characteristics at baseline, but 5-year relative survival rate was worse in African American patients with DLBCL when compared with white patientds with DLBCL (58.8% vs 62.3%, respectively). This study acknowledged the racial disparities in patients with NHL at the state level in Georgia both in incidence rate and in disease presentation, and in 5-year relative survival within NHL subtypes. This analysis and others have also examined the distributions of new lymphoma diagnoses across the state of Georgia to identify targeted regions for interventions and to characterize rural areas where outreach is needed.
A qualitative study based in rural Georgia gathered information on lymphoma survivors who sought treatment at a university research hospital.52 The overall goal of the study was to understand barriers to participation in university hospital–based clinical research among these patients living in rural Georgia. Individual, semistructured telephone interviews identified the main barriers to accessing such research opportunities as being distance to larger clinics, transportation difficulties, and less time with their clinician at university clinics. The use of patient portals to enhance communication between providers and patients was suggested as the potentially most significant contributor to better understanding of research opportunities. These authors also piloted an epidemiological questionnaire based on the findings of the InterLymph DLBCL Subtype Study to examine the behavioral and lifestyle characteristics among 50 African-American and 50 white patients with DLBCL in Georgia using a resource-constrained recruitment protocol that involved a single initial mailing. The questionnaire was composed of 30 items organized into 4 domains: (1) lifestyle and habits, (2) medical history, (3) family history, and (4) demographic background. Response rates differed significantly between African American patients (24%) and white/other race patients (48%) with DLBCL (P = .013). Overall, lifestyle, occupation, and medical histories were similar among African Americans and whites who returned the questionnaire. However, 75% of the African American individuals in this study were given a diagnosis of DLBCL before age 60 years, compared with 38% of the white population (P = .024). Approaches like this, which utilize geospatial analyses of disparities in cancer incidence to inform the sample selection and enrich the study with patients from high-incidence regions, provide examples of future strategies that will enhance efforts to customize strategies to local populations.
Texas
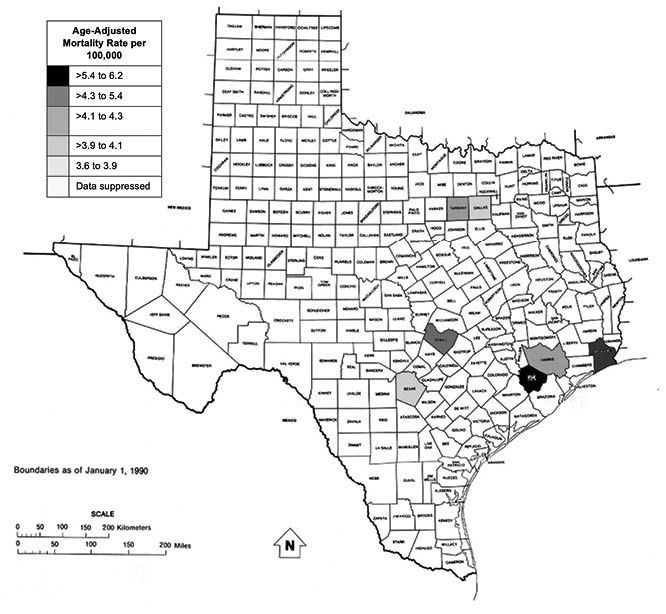
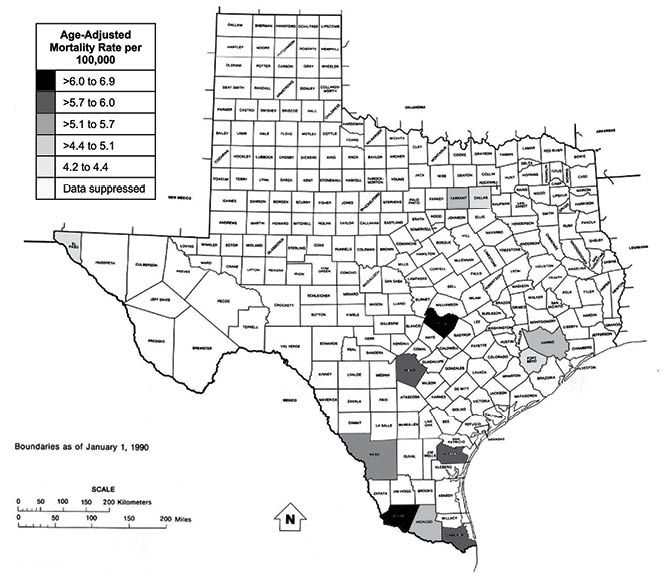
Utilizing data gathered and analyzed from statecancerprofiles.cancer.gov, we generated maps representing the age-adjusted NHL mortality rates per 100,000 in Hispanics and African Americans by county in Texas. The highest rates of mortality for NHL in African American patients were found in Fort Bend and Jefferson counties, with age-adjusted mortality rates of 6.2 (95% CI, 3.9-9.3) and 5.4 (95% CI, 3.4-8.2), respectively (Figure 1). The overall age-adjusted mortality rate is 3.9 (95% CI, 3.6-4.3) in African American patients with NHL for the entire state of Texas. The highest rates of mortality for NHL in Hispanic patients were found in Travis and Starr counties, with age-adjusted mortality rates of 6.9 (95% CI, 4.9-9.3) and 6.4 (95% CI, 3.7-10.3), respectively (Figure 2). Overall, Texas has an age-adjusted mortality rate of 5.0 (95% CI, 4.8-5.3) for Hispanic patients with NHL. Only 12 of 254 counties for Hispanic patients and 7 counties for African American patients had reported age-adjusted mortality rates. Because ofthe majority of counties having fewer than 3 average annual NHL deaths, rates for those counties were suppressed to ensure patient confidentiality and rate stability.
Figure 1. Age-Adjusted Mortality Rates for NHL in African American Patients by County. *Data generated from https://statecancerprofiles.cancer.gov/ NHL, non-Hodgkin lymphoma.
In 2016, the Texas Cancer Registry data documented 5172 newly diagnosed cases of lymphoma within the state of Texas: 61% non-Hispanic white, 26% Hispanic, 9% African American, 3% Asian. Women constitute 45% of all patients with lymphoma in Texas. These data can be utilized to identify how institutional populations and clinical trial enrollment compared with local population demographics for a cancer catchment area. Future approaches can assess the factors that mediate these disparities and determine strategies to overcome them: specifically, an increased focus on clinical trial awareness, education, and care coordination. Identifying these disparities can aid in defining institutional changes that will ultimately result in improved participation across all clinical trials.
Figure 2. Age-Adjusted Mortality Rates for NHL in Hispanic Patients by County. *Data generated from https://statecancerprofiles.cancer.gov/ NHL, non-Hodgkin lymphoma.
Research Strategies to Address Cancer Disparities
Proposed strategies to address cancer disparities involve accurately defining patient factors that increase one’s risk of poor outcome. Specifically, many studies do not have standardized definitions or categories of race versus ethnicity. Both the NCI and SEER database have recoded their definition of race to include the following categories: white, black, American Indian/Alaskan Native, Asian, or Pacific Islander. Ethnicity is defined as Hispanic or non-Hispanic, but in many studies, a person is identified as Hispanic without identification of his or her race. Notably, the SEER race codes have changed over the years. Prior to 2005, terms like all other races, unknown, or other were used, which can complicate the way we analyze data.53 Similarly, issues exist with correctly quantifying SES or identifying those with low health literacy. Once we apply standard definitions of race and ethnicity, as well as of other sociodemographic factors, we can use these measures in cancer registries and research protocols to create better representations of the populations in need. Additionally, once clear definitions are established, we can further clarify etiologies to explain these disparities, including individual, biologic, and operational factors.
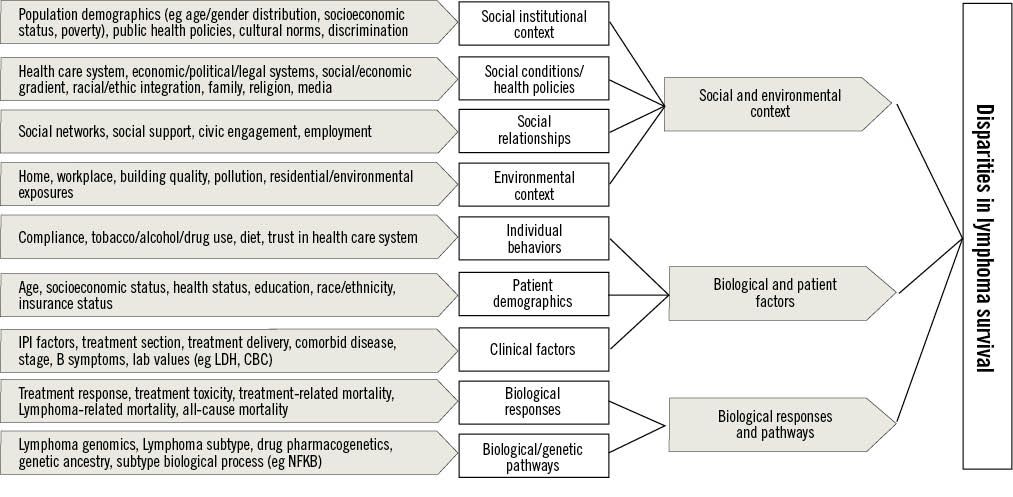
The information that was gathered utilizing the strategies above can be shared with stakeholders to inform real-world health policy and to encourage increased funding. These findings constitute possible mechanisms that may account for the racial disparities in DLBCL survival, which will require substantially divergent approaches to overcome. These studies have informed a multilevel model for understanding disparities in outcomes for lymphoma (Figure 3), which can be extended to other cancers in our catchment area. However, having a direct impact on the outcomes for the population of patients with hematologic cancers in our catchment area will first require an examination of knowledge gaps and behavioral factors that may influence outcomes within local communities, and then performance of geospatial analyses that characterize the cancer recurrence risk and mortality across various regions of the state.
Figure 3. Social, Biologic, and Environmental Factors That Contribute to Disparities in Lymphoma Survival CBC, complete blood count; LDH, lacic acid dehydrogenase; NFKB, nuclear factor kappa-B
Strategies for Improving Minority Enrollment on Clinical Trials
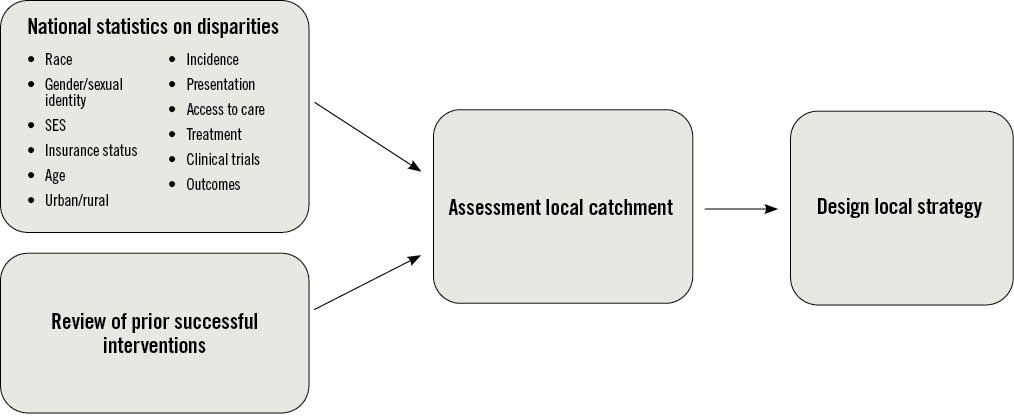
Biological, environmental, and social/institutional factors ultimately lead to cancer care disparities. As Figure 3 highlights, lymphoma-specific outcomes can be influenced by various institutional factors (eg, population demographics, health care system, economic/legal systems, public health policies), environmental factors (eg, residential exposure), individual factors (eg, age, socioeconomic status, health status, education, race/ethnicity, health literacy), and biological factors (eg, treatment response, genetic ancestry). Understanding that these themes can be applied broadly across hematologic malignancies, we developed a stepwise approach to design a clinical trial ideally without health disparities (Figure 4). The first step in addressing cancer disparities involves the establishment of national statistics on disparities, as well as an in-depth review of prior successful interventions. These data are then analyzed at a local level to assess whether enrollment on trials is proportionate to the number of patients observed in the catchment area. Ongoing awareness of past national disparity levels, along with an active assessment of current enrollees, will lead to a strategy that increases minority enrollment on clinical trials.
Figure 4. Proposed Framework to Design a Clinical Trial Without Health Disparities
There have been other published strategies across US cancer centers that aim to analyze these factors and optimize the recruitment process for minorities in cancer research. For instance, Regnante and colleagues conducted qualitative research in the form of interviews with multiple US cancer centers that are actively involved in increasing accrual rates for racial and ethnic minorities.54 From 2016 to 2018, the percentage of minority participation accrued in cancer clinic trials for all 8 cancer centers included in the study ranged from 10% to 40%. The results of this study led to the identification of 5 broad themes to increase participation in clinical trials: commitment from center leadership, investigator training and mentoring, community engagement, patient engagement, and operational practices.
The first theme, the need for commitment from cancer center leaders to ensure inclusion of minorities in clinical research, involves a primary emphasis on identifying any discrepancy within one’s institution and using that information to engage with providers. Efforts must be made to establish a diverse faculty, create broad outreach programs for both staff and patients, and form an active presence in the community to create an informed population. Next, an investment must be made in educating the workforce, including trainees, ancillary staff, and physicians, with the goal of cultural competency across the system and a better understanding of the issues that need to be addressed. Once hospital staff are informed, the focus can shift to engagement and education of the community. This entails forming partnerships with community clinics to create a system for inclusion of all potentially appropriate patients in clinical research. Patient-specific information must be adapted and tailored toward the needs of the community in a manner that is both culturally and linguistically understandable. All these best practices must work together to remove any potential barriers and create a system that allows for equal access on clinical trials.
While the need to actively recognize these barriers still exists, some strategies are currently in place and others are emerging to address these issues. Historically, many clinical trials have had strict criteria that can inadvertently exclude those minorities or individuals with lower SES. For example, trials may have exclusion criteria of comorbidities (such as diabetes and hypertension) that are more prevalent in African American patients, or have requirements for reading consents in English, which can exclude patients who are not fluent or face barriers in the translation of medical terminology. However, organizations such as the Communities Working Group are striving to adjust certain aspects of the clinical trial design, including inclusion/exclusion criteria that can ameliorate this issue. Furthermore, the National Institutes of Health (NIH) Revitalization Act of 1993 requires the NIH to establish guidelines for inclusion of women and minorities in clinical research,55 with the goal of ensuring that these subgroups are proportionately represented.
Unique strategies to address health disparities have developed amid the climate of coronavirus disease 2019 (COVID-19). The pandemic has created both challenges and innovations in the way health care is delivered universally. More clinics are connecting to patients and colleagues via video conferencing, telephone visits, remote monitoring, and electronic consults than ever before. According to the American Hospital Association, in 2017, 76% of US hospitals used telehealth in some capacity, typically only as an exception to the traditional in-person patient-physician visit.56 However, the use of telehealth has dramatically increased in response to COVID-19.57 These systemwide changes are due to the need to preserve health care access when in-person visits are not possible. This concept can be applied to vulnerable populations like the underserved and elderly patients in the post-COVID-19 era who will continue to have difficulty attending in-person visits. The accelerated implementation of telehealth due to COVID-19 ideally can reduce access barriers to cancer expertise in the future. In turn, this will provide opportunities to increase awareness of clinical trial options, facilitate care in home environments, and enhance appointment adherence for underserved patient populations.
We have aimed in this review to identify a variety of factors that contribute to survival rate among patients with hematologic malignancies, highlighting possible reasons why patients without insurance, those who live in rural/urban communities, and those with lower individual-level SES tend to have inferior survival. Recognition of these factors, however, is only the first step: Institutions and health care leaders must work to educate both their staff and the surrounding communities in a proactive manner to remove these barriers. Using our proposed framework, we hope to disseminate a comprehensive method to address these factors at a local level, with the goal of overcoming disparities nationally and of transforming our cancer health care delivery systems to improve outcomes for all patients.
Financial Disclosure: The authors have no significant financial interest in or other relationship with the manufacturer of any product or provider of any service mentioned in this article.
References:
- Sparano, Joseph A, et al. “Rituximab plus Concurrent Infusional EPOCH Chemotherapy Is Highly Effective in HIV-Associated B-Cell Non-Hodgkin Lymphoma.” Blood, American Society of Hematology, 15 Apr. 2010, ww.ncbi.nlm.nih.gov/pmc/articles/PMC2858478/.
- “Cancer Disparities.” National Cancer Institute, www.cancer.gov/about-cancer/understanding/disparities.
- “Center for the Elimination of Minority Health Disparities.” Center for the Elimination of Minority Health Disparities - Health Disparity - University at Albany-SUNY, www.albany.edu/cemhd/9142.php.
- Cancer Facts & Figures 2020. www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2020/cancer-facts-and-figures-2020.pdf.
- Kirtane K, Lee SJ. Racial and ethnic disparities in hematologic malignancies. Blood. 2017;130(15):1699-705.
- Patel MI, Ma Y, Mitchell BS, Rhoads KF. Understanding disparities in leukemia: a national study. Cancer Causes Control. 2012;23(11):1831-1837
- Fiala MA, Keller J, Stockerl-Goldstein KE, Tomasson MH, Vij R, Wildes TM. Treatment advances for multiple myeloma have disproportionally benefited patients who are young, white, and have higher socioeconomic status [abstract]. Blood. 2014;124(21). Abstract 555.
- Fiala MA, Wildes TM. Racial disparities in treatment use for multiple myeloma. Cancer. 2017;123(9):1590-1596
- Keegan TH, Clarke CA, Chang ET, Shema SJ, Glaser SL. Disparities in survival after Hodgkin lymphoma: a population-based study. Cancer Causes Control. 2009;20(10):1881-1892
- Kent EE, Morris RA, Largent JA, Ziogas A, Sender LS, Anton-Culver H Socioeconomic impacts on survival differ by race/ethnicity among adolescents and young adults with non-Hodgkin's lymphoma. J Cancer Epidemiol 2010;2010:824691.
- Li Y, Wang Y, Wang Z, Yi D, Ma S. Racial differences in three major NHL subtypes: descriptive epidemiology. Cancer Epidemiol. 2015;39(1):8-13.
- Shenoy PJ, Malik N, Nooka A, et al. Racial differences in the presentation and outcomes of diffuse large B-cell lymphoma in the United States. Cancer. 2010.
- Patel MI, Ma Y, Mitchell B, Rhoads KF. How do differences in treatment impact racial and ethnic disparities in acute myeloid leukemia? Cancer Epidemiol Biomarkers Prev. 2015;24(2):344-349
- Costa LJ, Huang JX, Hari PN. Disparities in utilization of autologous hematopoietic cell transplantation for treatment of multiple myeloma. Biol Blood Marrow Transplant. 2015;21(4):701-6.
- Fiala MA, Wildes TM. Racial disparities in treatment use for multiple myeloma. Cancer. 2017;123(9):1590-1596
- Swaminathan B, Thorleifsson G, Joud M, et al. Variants in ELL2 influencing immunoglobulin levels associate with multiple myeloma. Nature communications. 2015;6:7213.
- Went M, Sud A, Forsti A, et al. Identification of multiple risk loci and regulatory mechanisms influencing susceptibility to multiple myeloma. Nature communications. 2018;9(1):3707.
- Broderick P, Chubb D, Johnson DC, et al. Common variation at 3p22.1 and 7p15.3 influences multiple myeloma risk. Nature genetics. 2011;44(1):58-61.
- Erickson SW, Raj VR, Stephens OW, et al. Genome-wide scan identifies variant in 2q12.3 associated with risk for multiple myeloma. Blood. 2014;124(12):2001-3.
- Urayama KY, Jarrett RF, Hjalgrim H, et al. Genome-wide association study of classical Hodgkin lymphoma and Epstein-Barr virus status-defined subgroups. Journal of the National Cancer Institute. 2012;104(3):240-53.
- Enciso-Mora V, Broderick P, Ma Y, et al. A genome-wide association study of Hodgkin's lymphoma identifies new susceptibility loci at 2p16.1 (REL), 8q24.21 and 10p14 (GATA3). Nature genetics. 2010;42(12):1126-30.
- Frampton M, da Silva Filho MI, Broderick P, et al. Variation at 3p24.1 and 6q23.3 influences the risk of Hodgkin's lymphoma. Nature communications. 2013;4:2549.
- Vijayakrishnan J, Qian M, Studd JB, et al. Identification of four novel associations for B-cell acute lymphoblastic leukaemia risk. Nature communications. 2019;10(1):5348.
- Kim DH, Lee ST, Won HH, et al. A genome-wide association study identifies novel loci associated with susceptibility to chronic myeloid leukemia. Blood. 2011;117(25):6906-11.
- Law PJ, Berndt SI, Speedy HE, et al. Genome-wide association analysis implicates dysregulation of immunity genes in chronic lymphocytic leukaemia. Nature communications. 2017;8:14175.
- Berndt SI, Skibola CF, Joseph V, et al. Genome-wide association study identifies multiple risk loci for chronic lymphocytic leukemia. Nature genetics. 2013;45(8):868-76.
- Speedy HE, Di Bernardo MC, Sava GP, et al. A genome-wide association study identifies multiple susceptibility loci for chronic lymphocytic leukemia. Nature genetics. 2014;46(1):56-60.
- Slager SL, Skibola CF, Di Bernardo MC, et al. Common variation at 6p21.31 (BAK1) influences the risk of chronic lymphocytic leukemia. Blood. 2012;120(4):843-6.
- Chubb D, Weinhold N, Broderick P, et al. Common variation at 3q26.2, 6p21.33, 17p11.2 and 22q13.1 influences multiple myeloma risk. Nature genetics. 2013;45(10):1221-5.
- Mitchell JS, Li N, Weinhold N, et al. Genome-wide association study identifies multiple susceptibility loci for multiple myeloma. Nature communications. 2016;7:12050.
- Cerhan JR, Berndt SI, Vijai J, et al. Genome-wide association study identifies multiple susceptibility loci for diffuse large B cell lymphoma. Nature genetics. 2014;46(11):1233-8.
- Skibola CF, Berndt SI, Vijai J, et al. Genome-wide Association Study Identifies Five Susceptibility Loci for Follicular Lymphoma outside the HLA Region. American journal of human genetics. 2014;95(4):462-71.
- Conde L, Halperin E, Akers NK, et al. Genome-wide association study of follicular lymphoma identifies a risk locus at 6p21.32. Nature genetics. 2010;42(8):661-4.
- Slager SL, Rabe KG, Achenbach SJ, et al. Genome-wide association study identifies a novel susceptibility locus at 6p21.3 among familial CLL. Blood.117(6):1911-6.
- Du Z, Weinhold N, Song GC, et al. A meta-analysis of genome-wide association studies of multiple myeloma among men and women of African ancestry. Blood Adv. 2020;4(1):181-90.
- Tan DE, Foo JN, Bei JX, et al. Genome-wide association study of B cell non-Hodgkin lymphoma identifies 3q27 as a susceptibility locus in the Chinese population. Nature genetics. 2013;45(7):804-7.
- Bassig BA, Cerhan JR, Au WY, et al. Genetic susceptibility to diffuse large B-cell lymphoma in a pooled study of three Eastern Asian populations. European journal of haematology. 2015;95(5):442-8
- Madbouly A, Wang T, Haagenson M, et al. Investigating the Association of Genetic Admixture and Donor/Recipient Genetic Disparity with Transplant Outcomes. Biol Blood Marrow Transplant. 2017;23(6):1029-37.
- Baughn LB, Pearce K, Larson D, et al. Differences in genomic abnormalities among African individuals with monoclonal gammopathies using calculated ancestry. Blood Cancer J. 2018;8(10):96.
- Lee, MJ; Koff, JL; Switchenko, JM; Jhaney, CI; Harkins, A; Patel, SP; Dave, SS; and Flowers, CR. Genome-Defined African Ancestry is Associated with Distinct Mutations and Worse Survival in Diffuse Large B-Cell Lymphoma, Cancer, In press.
- Han, Xuesong, et al. “Insurance Status Is Related to Diffuse Large B‐Cell Lymphoma Survival.” American Cancer Society Journals, John Wiley & Sons, Ltd, 28 Jan. 2014, acsjournals.onlinelibrary.wiley.com/doi/full/10.1002/cncr.28549.
- Goldstein JS, Nastoupil LJ, Han X, Jemal A, Ward E, Flowers CR. Disparities in survival by insurance status in follicular lymphoma. Blood 2018;132:1159-1166.
- Jordan S. Goldstein, Jeffrey M. Switchenko, Madhusmita Behera, Christopher R. Flowers & Jean L. Koff (2019) Insurance status impacts overall survival in Burkitt lymphoma, Leukemia & Lymphoma, 60:13, 3225-3234, DOI: 10.1080/10428194.2019.1623884
- Flowers CR, Fedewa SA, Chen AY, Nastoupil LJ, Lipscomb J, Brawley OW, Ward EM.Disparities in the early adoption of chemoimmunotherapy for diffuse large B-cell lymphoma in the United States. Cancer Epidemiol Biomarkers Prev. 2012 Sep;21(9):1520-30.
- Garth N. Graham Breastfeeding Medicine. Oct 2016. 396-397. http://doi.org/10.1089/bfm.2016.0113
- Ritter AJ, Goldstein JS, Ayers AA, Flowers CR. Rural and urban patients with diffuse large B-cell and follicular lymphoma experience reduced overall survival: a National Cancer DataBase study. Leuk Lymphoma 2019;60:1656-1667.
- Parker T. USDA ERS—rural-urban continuum codes. Available at: https://www.ers.usda.gov/data-products/rural-urban-continuum-codes/
- Murthy VH, Krumholz HM, Gross CP. Participation in cancer clinical trials: race-, sex-, and age-based disparities. JAMA. 2004 Jun 9;291(22):2720–6
- Tejeda HA, Green SB, Trimble EL, Ford L, High JL, Ungerleider RS, Friedman MA, Brawley OW. Representation of African-Americans, Hispanics, and whites in National Cancer Institute cancer treatment trials. J Natl Cancer Inst. 1996 Jun 19;88(12):812–6.
- Joseph M Unger, Riha Vaidya, Dawn L Hershman, Lori M Minasian, Mark E Fleury, Systematic Review and Meta-Analysis of the Magnitude of Structural, Clinical, and Physician and Patient Barriers to Cancer Clinical Trial Participation, JNCI: Journal of the National Cancer Institute, Volume 111, Issue 3, March 2019, Pages 245–255, https://doi.org/10.1093/jnci/djy221
- Ayers AA, Lyu L, Dance K, Ward KC, Flowers CR, Koff JL, McCullough LE. Characterizing Lymphoma Incidence and Disparities for a Cancer Center Catchment Region. Clin Lymphoma Myeloma Leuk. 2019 Nov;19(11):699-708.e5.
- Chen, Lillian, et al. “Priorities for Rural Lymphoma Survivors: A Qualitative Study.” Clinical Lymphoma Myeloma and Leukemia, Elsevier, 19 Oct. 2019, www.sciencedirect.com/science/article/pii/S215226501931986X.
- “Race Recode Changes - SEER Documentation.” SEER, seer.cancer.gov/seerstat/variables/seer/race_ethnicity/.
- Jeanne M. Regnante, Nicole A. Richie, Lola Fashoyin-Aje, Michelle Vichnin, Marvella Ford, Upal Basu Roy, Kenneth Turner, Laura Lee Hall, Evelyn Gonzalez, Nestor Esnaola, Luther T. Clark, Homer C. AdamsIII, Olatunji B. Alese, Keerthi Gogineni, Lorna McNeill, Daniel Petereit, Ify Sargeant, Julie Dang, Coleman Obasaju, Quita Highsmith, Simon Craddock Lee, Spencer C. Hoover, Erin L. Williams, and Moon S. ChenJr. US Cancer Centers of Excellence Strategies for Increased Inclusion of Racial and Ethnic Minorities in Clinical Trials. Journal of Oncology Practice 2019 15:4, e289-e299
- “NIH Policy and Guidelines on The Inclusion of Women and Minorities as Subjects in Clinical Research.” National Institutes of Health, U.S. Department of Health and Human Services, grants.nih.gov/policy/inclusion/women-and-minorities/guidelines.htm.
- “Fact Sheet: Telehealth: AHA.” American Hospital Association, www.aha.org/factsheet/telehealth.
- A Mehrotra, K Ray, DM Brockmeyer, ML Barnett, JA Bender. Rapidly Converting to “Virtual Practices”: Outpatient Care in the Era of Covid-19.NEJM Catalyst2020; 1 https://catalyst.nejm.org/doi/abs/10.1056/CAT.20.0091
Late Hepatic Recurrence From Granulosa Cell Tumor: A Case Report
Granulosa cell tumors exhibit late recurrence and rare hepatic metastasis, emphasizing the need for lifelong surveillance in affected patients.