Systemic Approaches for Multifocal Bronchioloalveolar Carcinoma: Is There an Appropriate Target?
Bronchioloalveolar carcinoma (BAC) is a subset of pulmonary adenocarcinoma characterized by distinct and unique pathological, molecular, radiographic, and clinical features. While the incidence of pure BAC is rare, comprising only 1% to 4% of non–small-cell lung cancer (NSCLC), mixed subtypes (including BAC with focal invasion and adenocarcinoma with BAC features) represent as much as 20% of adenocarcinomas-and that figure may be increasing. Despite the longstanding recognition of this entity, there is no established treatment paradigm for patients with multifocal BAC, resulting in competing approaches and treatment controversies. Current options for multifocal BAC include both surgery and systemic therapies. Unfortunately, prospective data on systemic approaches are limited by study design and small patient numbers; there are only seven phase II studies involving four therapies. This article evaluates key characteristics of BAC, including the current understanding of histopathology and tumor biology. In addition, it comprehensively reviews the systemic phase II studies in an attempt to clarify the therapeutic challenges in this disease. It also includes the first proposed treatment paradigm that integrates both EGFR mutational status and the sub-histologies, mucinous and nonmucinous BAC.
Bronchioloalveolar carcinoma (BAC) is a subset of pulmonary adenocarcinoma characterized by distinct and unique pathological, molecular, radiographic, and clinical features. While the incidence of pure BAC is rare, comprising only 1% to 4% of non–small-cell lung cancer (NSCLC), mixed subtypes (including BAC with focal invasion and adenocarcinoma with BAC features) represent as much as 20% of adenocarcinomas-and that figure may be increasing. Despite the longstanding recognition of this entity, there is no established treatment paradigm for patients with multifocal BAC, resulting in competing approaches and treatment controversies. Current options for multifocal BAC include both surgery and systemic therapies. Unfortunately, prospective data on systemic approaches are limited by study design and small patient numbers; there are only seven phase II studies involving four therapies. This article evaluates key characteristics of BAC, including the current understanding of histopathology and tumor biology. In addition, it comprehensively reviews the systemic phase II studies in an attempt to clarify the therapeutic challenges in this disease. It also includes the first proposed treatment paradigm that integrates both EGFR mutational status and the sub-histologies, mucinous and nonmucinous BAC.
Bronchioloalveolar carcinoma (BAC) is a subset of pulmonary adenocarcinoma characterized by distinct and unique pathological, molecular, radiographic, and clinical features. BAC was initially described by Malassez in 1876.[1] The term “bronchioloalveolar carcinoma” was coined by Liebow in 1960 and identifies a well-differentiated tumor (adenocarcinoma) with neoplastic cells that spreads along alveoli without stromal reaction or invasion, and with preservation of alveolar architecture.[2] Although the pathological assessment of this tumor is still evolving, the current (1999) definition of BAC by the World Health Organization (WHO) is restricted to lesions with a pure bronchioloalveolar growth pattern in which there is no evidence of invasion of stroma, pleura, or lymphatic spaces.[3] The clinical applicability of this definition remains in question, considering that BAC most often presents as admixed adenocarcinoma, with the clinical course of these tumors often differing from that of both pure BAC and adenocarcinoma. The incidence of pure BAC is rare, comprising only 1% to 4% of non–small-cell lung cancer (NSCLC); however, these mixed subtypes, including BAC with focal invasion and adenocarcinoma with BAC features, represent as much as 20% of adenocarcinomas-and their frequency may be increasing.[4]
As BAC becomes a more recognized entity within the pathological continuum of adenocarcinoma, several controversies have emerged regarding the appropriate management of these tumors, especially those that represent multifocal or unresectable disease. First, while BAC features may be prognostic of improved survival, it remains unclear whether the percentage of BAC admixed within a tumor is prognostic of outcome or predictive of therapy efficacy. For example, should those adenocarcinomas with greater BAC features be more conservatively managed than those with less BAC? Second, there is an increasing awareness that two subtypes of BAC lesions exist: mucinous and nonmucinous.[5] Whether this pathological distinction is clinically relevant and whether it should guide management decisions remain unclear; these questions will be addressed in the discussion section of this review. Finally, it has been demonstrated consistently that patients with advanced-stage BAC have a disproportionately high response to the epidermal growth factor receptor (EGFR) tyrosine kinase inhibitors (TKIs) erlotinib and gefitinib. Recent phase III data in patients with advanced NSCLC have demonstrated the EGFR mutation to be a reliable predictor of response to TKIs in the front-line setting.[8] However, whether response to TKIs in BAC is exclusively mediated by the EGFR mutation that is more frequently found in this subtype of tumor has yet to be prospectively evaluated. In this review, we attempt to evaluate these controversies as we discuss the key characteristics and current management of multifocal/unresectable BAC.
Histopathology of BAC
The definition of BAC has evolved significantly over the years. In 1960, when Averill Liebow gave the tumor its current name, BAC was defined as a subtype of adenocarcinoma with four features: well-differentiated cytology, an origin distal to recognizable bronchi, a proclivity for lymphatic and aerogenous spread, and a tendency to grow across intact alveolar septa.[2] Liebow asserted, however, that this last feature was probably “imaginary,” implying that despite seemingly preserved architecture, invasion was a likely feature. In 1999, a major shift occurred in the WHO classification: BAC was redefined as a neoplasm that demonstrated pure lepidic growth with a lack of invasion of stroma, blood vessels, or pleura.[3] The modification essentially restricted BAC to carcinoma in situ and was maintained in the 2004 revision of the criteria.[5] Currently, tumors that are predominantly BAC and that have areas of invasion are classified as “mixed subtype adenocarcinomas.”
FIGURE 1
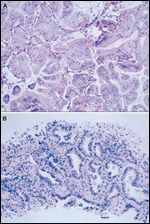
Histopathology of Mucinous vs Nonmucinous Bronchioloalveolar Carcinomas (BACs) (Hematoxylin and Eosin Stain, High-Power Magnification)
The WHO decision to reclassify BAC as a distinct pathological entity was largely based on seminal work by Noguchi and colleagues, who examined 236 cases of small (less than 2 cm), surgically resected peripheral adenocarcinomas with mediastinal and pulmonary hilar lymph node dissection.[9] Samples were separated into groups by histology, and patients were monitored longitudinally for survival. In patients with Noguchi type A histology (localized bronchioloalveolar carcinoma [LBAC]) and type B histology (LBAC with foci of alveolar collapse), 0% showed lymph node metastasis, and survival was 100% at 5 years. However, among patients with Noguchi type C histology (LBAC with active fibroblastic proliferation), 28% had lymph node metastasis, and 5-year survival was 75%. Furthermore, patients with poorly differentiated adenocarcinoma (Noguchi type D histology) had a 52% 5-year survival rate. These results demonstrated that BAC had a distinct clinical course differing from that of adenocarcinoma and suggesting that this type of tumor warranted its own classification.
Two major subtypes of BAC are recognized by the WHO-mucinous BAC and nonmucinous BAC-along with a third category that represents a combination of the two (Figure 1).[5] Increasing evidence suggests that the major subtypes represent biologically distinct entities and underscores the necessity of distinguishing between the two in pathology specimens.[10]
The nonmucinous variant is the clinically predominant subtype, occurring in 40% to 60% of cases.[11] Nonmucinous BAC tumors tend to present grossly as solitary peripheral nodules and are histologically composed of cuboidal or columnar cells with eosinophilic or clear cytoplasm, with or without vacuolization.[12,13] Nonmucinous BAC is recognized as comprising two cell types: Clara cells, with apical snouts and PAS+ granules; and type 2 pneumocytes, often with eosinophilic nuclear inclusions. No clinical or prognostic difference has been ascribed to a predominance of either cell type.[13] Immunohistochemically, the nonmucinous variant of BAC exhibits a pattern similar to that of conventional adenocarcinoma, with cytokeratin 7 (CK7) and thyroid transcription factor 1 (TTF1) positivity and cytokeratin 20 (CK20) negativity.[5] BAC with nonmucinous histology is more often dependent on EGFR pathway mutations and is consequently more sensitive to EGFR-targeted therapy.[10]
Mucinous BAC occurs in anywhere from 25% to 50% of patients.[11,13] In contrast to nonmucinous tumors, mucinous BAC more commonly presents with extensive disease, manifested as multiple nodules or diffuse consolidation (pneumonic pattern). Because of the more advanced stage at diagnosis, overall prognosis is poorer. Histologically, cells are tall and columnar with basal nuclei and abundant mucin.[12,13] The tumor is thought to arise from metaplastic goblet cells. In mucinous BAC, immunohistochemistry (IHC) results tend to be more variable: CK7 is usually positive, as in nonmucinous BAC; however, CK20 is positive, and TTF1 is usually negative-or weak and patchy if positive. K-ras mutations are more commonly detected in mucinous BAC, likely accounting for the relative insensitivity of this subclass to EGFR-based treatments.[14]
In patients with mixed subtype adenocarcinoma, the exact contribution of a bronchioloalveolar component to prognosis has been the subject of debate. In the only Western study to address this question, Ebright and colleagues reported no significant difference in survival between groups with pure BAC, BAC with focal invasion, and adenocarcinoma with BAC features.[15] The study did include patients with pure BAC who had multifocal disease and pneumonic-type presentations; these patients had poorer expected outcomes. In contrast to the Ebright data, multiple previous Japanese studies have provided evidence-in addition to that of Noguchi’s work-to support a favorable prognosis for specimens with large proportions of BAC and minimal invasion.[16-19] Terasaki and colleagues grouped specimens according to increasing proportions of BAC and reported that groups with either pure BAC or BAC with minimal areas of invasion were less likely to have pleural invasion or metastatic spread to lymph nodes or vasculature.[20] These studies suggest that tumors with higher proportions of BAC may be prognostically more favorable.
In light of the possible differences in clinical behavior between BAC with minimal invasion and tumors with larger invasive components, some authors have proposed that a category called “minimally invasive adenocarcinoma” be established in future classifications.[21] Sakurai and colleagues demonstrated that the prognosis of BAC with stromal invasion limited to the area of tumor growth or the periphery of the tumor scar was equal to that seen in pure BAC.[18] Similarly, Yim and colleagues reported that the prognosis of patients with BAC and invasion of less than 5 mm was equivalent to that of patients with BAC and no evidence of invasion.[19] In 2004, however, a consensus definition of “minimally invasive” BAC was not recommended by the WHO panel on the basis of lack of sufficient evidence.[22] As further data become available, it is possible that this category may be formally separated, considering its increased incidence and clinical relevance.
Tumor Biology
FIGURE 2
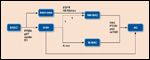
Proposed Model of Tumorigenesis and Acquired Mutations
Recent investigations into the molecular biology of BAC have focused on its potential role as an intermediate stage in the development of lung adenocarcinoma (Figure 2).[4] In this model, stepwise mutations drive the transformation of the malignant clone through a series of histologies, from adenomatous hyperplasia (AAH), to BAC, and finally invasive adenocarcinoma. The initial insult is thought to occur in the stem cell compartment in response to lung damage, and progenitor cells known as bronchioloalveolar stem cells, or BASCs, are recruited. Several mouse models have demonstrated that mutations, including K-ras, p27kip, and PTEN, play a key role in the recruitment and subsequent progression of BASCs to invasive disease.[23-25] At the cellular level, the proliferation gives rise to both Clara cells and type II pneumocytes that accumulate and transform into what is recognized histologically as AAH.[4]
The specific progression from AAH to BAC likely occurs through the accumulation of successive genetic hits, including the allelic loss of 9p, 8q, and 17p.[26-28] However, it is important to note that this transformation gives rise to a specific biologic subset of BAC tumors. Molecular analyses have revealed that K-ras mutations are commonly present in AAH, while EGFR mutations are infrequent, indicating that BACs and adenocarcinomas that are reliant on EGFR mutations probably do not arise from AAH.[29] The reliance of particular BAC subtypes on either K-ras or EGFR mutations is thought to be mutually exclusive[30,31] and serves to underscore biologic differences that support the notion that BAC actually comprises two separate diseases.[32]
Mucinous disease is more frequently associated with a variety of K-ras mutations, some specifically occurring on exon 1 (codon 12).[33,34]. In contrast, EGFR mutations and amplification or polysomy are associated almost exclusively with nonmucinous disease.[10,32] Furthermore, these EGFR mutations have been shown to co-exist with alterations in human epidermal growth factor receptor 2 (HER2).[35,36] Nonmucinous disease is also likely to be found with a higher frequency in smokers than is mucinous disease. Given these findings, further investigations will likely answer the question of whether AAH is a precursor of mucinous disease exclusively.
In the face of further molecular alterations, BAC is thought to transform eventually into frank adenocarcinoma. However, the exact sequence that drives this progression remains unknown. The expression of focal adhesion kinase (FAK) is significantly lower in BAC than in adenocarcinoma, indicating its potential role in the development of invasive disease.[37] Other genetic alterations have also been shown to occur more commonly in adenocarcinoma than in BAC. These include loss of heterozygosity at 1p, 3p, 7p, and 18q, and increased levels of vascular endothelial growth factor (VEGF) expression.[27,29]
As is the case for other tumors, the stepwise process of BAC tumorigenesis is complex, involving multiple pathways. Future investigations in this area hopefully will elucidate specific driver mutations that will serve to direct our approach to therapy at each step along the spectrum of disease.
Radiologic Features
BAC presents with a range of features that fall into three major radiographic patterns: solitary pulmonary nodules or masses (commonly termed ground glass opacities [GGO]), localized consolidation, and diffuse disease.[38-40] While each of these represents a distinct pattern that may be reflective of clinical course, a combination of features may be present in a single patient.[40]
Solitary nodules or masses are the most common BAC radiographic findings and are seen in approximately 40% of patients.[41] Lesions vary from having well-defined to irregular borders and are composed of solid soft-tissue attenuation, ground glass attenuation, or a mixture of the two.[40,42] The proportion of each is thought to reflect biological differences within the tumor.[41] Nodules with a predominant GGO component correspond to lower Noguchi subtypes, suggest nonmucinous BAC, and are likely attributable to the lepidic growth pattern of the malignancy.[43-48] Mixed lesions are more frequently a feature of Noguchi type C tumors and suggest mixed subtype adenocarcinoma.[42] An increasing solid component suggests higher biologic virulence and increased likelihood of the tumor having an invasive component.[41]
Localized consolidation accounts for 30% of cases and is believed to be typical of mucinous BAC[49]. While diffuse parenchymal infiltration is often difficult to differentiate from pneumonic or other inflammatory processes, certain radiologic features favor a diagnosis of BAC over pneumonia.[48] These include attenuation, stretching, and widening of branching air-filled bronchi within a consolidation; and bulging of the interlobar fissure, which occurs secondary to mucin production and tumor swelling.[50] Mucin production is also thought to be the source of what was described by Im and colleagues as the “CT angiogram sign,” or visibly enhancing pulmonary vessels within a consolidation.[51]
Diffuse disease, which accounts for another 30% of cases, presents in various forms, including multinodular disease in one or more lobes, or a “crazy paving” pattern of extensive GGO and septal thickening.[47,48] Akira and colleagues reported that the combination of consolidation, satellite nodules, and remote areas of GGO is highly characteristic of BAC.[52]
CT imaging represents the standard modality for assessment of the extent of disease. The utility of fluorodeoxyglucose positron emission tomography (FDG-PET) in BAC also has been explored. The standardized uptake values (SUVs) of BAC are significantly lower than those seen in other adenocarcinoma subtypes, probably due to BAC’s longer doubling times and slower rates of proliferation.[53,54] However, multiple reports have established a high false-negative rate for PET imaging in the diagnosis of BAC.[55,56] In fact, only half of all cases have a maximum SUV of greater than 2.5, the commonly accepted threshold that distinguishes benign from malignant lung neoplasms.[42,57] Beyond diagnosis, FDG-PET may have more of a role in elucidating the biological aggressiveness and prognosis of established lesions-and thus in directing care. Raz and colleagues demonstrated that in patients with node-negative BAC, preoperative PET-avidity significantly predicts lower long-term mortality compared with PET-negative disease.[4] Gandara and colleagues have suggested that close observation with serial imaging may represent a viable alternative to surgery in patients with PET-negative disease.[41]
In recent years, advances in MRI technology have prompted investigations into the potential of this modality as a diagnostic tool for assessing BAC. Tanaka and colleagues described techniques such as STIR (respiratory-triggered short inversion time [TI] inversion recovery) and high–b-value diffusion-weighted imaging (DWI) that significantly differentiated pure BAC from other adenocarcinoma subtypes.[58] Gadolinium-enhanced dynamic MRI also has been shown to differentiate BAC from non-BAC lesions.[58,59] To date, however, the clinical role of MRI in the evaluation of solitary nodules remains limited.[60]
In summary, BAC presents radiographically in several distinct patterns and morphologies that ultimately correlate with biologic differences related to histology and tumor aggressiveness. At present, CT remains the standard for initial diagnostic evaluation. However, the utility of FDG-PET in establishing the metabolic activity of disease, and its potential for determining the rate of growth of tumors, may result in its incorporation into future workup algorithms.
Clinical Course
The clinical presentation of BAC generally reflects the extent of disease. Most commonly, BAC presents as an asymptomatic process with 40% to 60% of cases incidentally diagnosed after patients had undergone chest imaging for other indications.[61,62] Unlike with other histological subsets of NSCLC, most patients with pure BAC present with surgically resectable disease-a reflection of the fact that pure BAC by definition is not associated with lymph node disease or distant metastasis.[9,15,20,63,64] However, up to 80% of BAC cases present with admixed adenocarcinoma; of these tumors, 10% to 25% have mediastinal nodal involvement, with 5% demonstrating distant metastatic disease, suggesting that an initial surgical approach may not be indicated.[61]
The clinical behavior of multifocal, unresectable BAC has been elucidated only from retrospective studies and is characterized by its tendency to present with intrathoracic metastasis, slow rate of growth and progression, longer median survival, and increased prevalence in women and nonsmokers.[65] When symptomatic, patients most commonly present with cough, sputum production, chest pain, or dyspnea-and less frequently with fever, hemoptysis, weight loss, or fatigue. Patients with advanced diffuse bilateral pulmonary disease can present with severe bronchorrhea and refractory hypoxemia from intrapulmonary shunting.[66] This clinical presentation is more commonly associated with the mucinous subset of BAC and can be mistaken for pneumonia or pneumonitis. Death is characteristically secondary to respiratory failure in the setting of diffuse pulmonary involvement infection, rather than resulting from the distant spread of cancer and involvement of other organ sites.[11] Metastases to sites outside the lungs are presumably due to an invasive component that precludes a diagnosis of pure BAC.
Management
TABLE 1
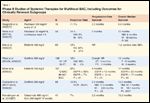
Phase II Studies of Systemic Therapies for Multifocal BAC, Including Outcomes for Clinically Relevant Subgroups
Despite the longstanding recognition of this entity, there is no established treatment paradigm for patients with multifocal BAC. This is largely due to the low incidence of pure BAC. However, other factors, including inconsistent pathological criteria and a scarcity of preclinical data (mouse lung carcinomas that mimic classic human BAC histologically are nonexistent[67]) have led to knowledge gaps regarding the optimal treatment of this disease. Current options for multifocal BAC include both surgery and systemic therapies. Unfortunately, prospective data on both modalities are limited by study design and small patient numbers. In addition, the small phase II studies and retrospective series that have been published on systemic approaches have yielded divergent results as a result of differing radiographic criteria (WHO versus RECIST [Response Evaluation Criteria in Solid Tumours]), pathological assessments, and primary endpoints (Table 1).
Surgery
Although a comprehensive assessment of the surgical literature for BAC is beyond the scope of this article, a brief discussion of this literature is warranted, given that surgical resection is the only potentially curative modality for this disease. Both prospective and retrospective surgical studies have demonstrated that patients with completely resected limited stage (stage I/II) BAC have a longer survival as well as lower rates of recurrence and lymph node micrometastasis than do patients with other subtypes of NSCLC.[68,69] In addition, further studies have suggested that completely resected multifocal (stage IIIB or IV) BAC is associated with survival equivalent to that of resected stage I NSCLC.[4] Specifically, Robert and colleagues and Furak and colleagues have reported 5-year survival rates of 64% and 82%, respectively, for completely resected multifocal BAC.[64,70] Based on the surgical series, it seems reasonable for fit patients with multifocal disease to be referred to an experienced surgeon for possible surgical resection. However, a definitive surgical approach must take into account the potential presence of invasive areas of adenocarcinoma admixed in the tumor, since it is impossible to differentiate pure BAC from admixed BAC by needle biopsy or frozen section.[71-73] In addition, mediastinal node involvement is found in up to 25% of admixed BAC, which suggests that these tumors may be more extensive than what is initially demonstrated radiographically or pathologically.[61]
Systemic Treatment
Although BAC has traditionally been perceived as a chemoresistant disease, there have been only two phase II studies evaluating the role of cytotoxic chemotherapy in BAC; each of these utilized paclitaxel. Experience with newer, third-generation agents such as pemetrexed (Alimta) or gemcitabine (Gemzar) has been described only in case reports or retrospective series; however, these agents have demonstrated competitive outcomes.[74,75] In the first prospective phase II study evaluating cytotoxic chemotherapy (S9714), 58 patients with confirmed stage IIIB/IV BAC received paclitaxel, 35 mg/m2/24 hours continuously infused for 96 hours every 3 weeks for a planned 6 cycles.[76] The objective response rate was 14%, with stable disease achieved in 40% of patients. Median progression-free survival (PFS) and overall survival (OS) were 5 and 12 months, respectively. Retrospective evaluation demonstrated a marked difference in outcome between the different histological subtypes; the nonmucinous subtype had an OS of 9 months, compared with OS for the mucinous subtype and for adenocarcinoma with BAC of 17 and 18 months, respectively. Notably, there were no responses (0%) in patients with nonmucinous BAC, compared with a 19% response rate in patients with mucinous BAC. Unfortunately, this regimen resulted in unacceptable grade 3-5 toxicity, including neutropenia (43%), febrile neutropenia (12%), infection (22%), pharyngitis (10%), and five treatment-related deaths; thus, the regimen was subsequently abandoned. In a second very small phase II study evaluating paclitaxel in multifocal BAC,[77] 19 patients with unresectable stage III/IV or recurrent BAC received intravenous (IV) paclitaxel, 200 mg/m2 over 3 hours, every 21 days until progression of disease or a maximum of 6 cycles. This study resulted in a disappointing response rate of only 11% and median PFS and OS of only 2.2 and 8.6 months, respectively. The incidence of hematological grade 3-5 toxicity was less than that reported in the earlier paclitaxel trial; the most common adverse effects were neutropenia (21%) and anemia and leucopenia (5.3% each).
Retrospective analysis of early studies evaluating the role of EGFR TKIs in NSCLC demonstrated disproportionate and often dramatic responses in those tumors classified as BAC.[78-80] This observation has led to five phase II studies exploiting the EGFR pathway with either the TKIs erlotinib (Tarceva) and gefitinib (Iressa) or the monoclonal antibody cetuximab (Erbitux).
In the first study, Kris and colleagues evaluated the role of erlotinib, 150 mg/d, in 69 patients with unresectable stage III/IV BAC (25% with “pure” BAC and 74% with adenocarcinoma with BAC features).[81] Results of this study demonstrated a partial response rate of 12% and a one-year survival rate of 58%. Response rates correlated with both clinical and histological features; more robust responses were seen in nonsmokers than in smokers (43% vs 37%) and in patients who had adenocarcinoma with BAC features than in patients who had “pure” BAC (30% vs 7%).
In a second trial evaluating the role of TKIs in BAC (S0126),[82] 136 patients (101 untreated, 35 previously treated) received gefitinib, 500 mg/d until disease progression or prohibitive toxicity, with one-year survival selected as the primary endpoint. The overall response rates in the untreated and previously treated groups were 17% and 9%, respectively. Median PFS was 4 months in the untreated group and 3 months in the previously treated group. Interestingly, a similar median OS was demonstrated in the two groups as well (13 months in the untreated group, 12 months in the previously treated group), and the one-year survival rate was 51% in both groups. An exploratory multivariate analysis demonstrated that the clinical variables associated with improved OS included female sex (hazard ratio [HR], 1.83; P=.063), the development of rash (HR, 2.41; P=.01), and a performance status of 1 or less (HR, 2.07; P=.006). Although the dose of gefitinib used was considered to be double the normal dose, the regimen was reasonably well tolerated; the grade 3-4 toxicities seen included rash (12%), diarrhea (21%), fatigue (5%), nausea (4%), and elevated transaminase levels (6%).
Two retrospective studies were subsequently published (in abstract form only) that importantly sought to identify histological and molecular predictors of outcome in the S0126 study. In a biomarker analysis of this study, Hirsch and colleagues showed that the presence of EGFR-activating mutations, increased EGFR protein expression as demonstrated by IHC, and increased gene copy as demonstrated by fluorescence in situ hybridization (FISH) were each predictive of response to gefitinib; however, only the latter two markers were associated with increased patient survival.[83] In a second analysis, Franklin and colleagues were able to demonstrate drastically different outcomes and responses to gefitinib for different sub-histologies.[84] The rate of response to gefitinib in nonmucinous BAC was 30%, with stable disease achieved in an additional 40%, compared with a 0% response rate and 0% achievement of stable disease in mucinous BAC. In addition, nonmucinous BAC was associated with significantly longer survival (HR, 2.85; P=.0030). It is likely that the differing molecular profiles of these two sub-histologies, as reflected in the fact that EGFR mutations are exclusively found in nonmucinous BAC, were responsible for the discrepant responses seen with gefinitib in this trial.
Following this study, Miller and colleagues sought to determine the activity of erlotinib, 150 mg, in 101 patients with either pure BAC (n=12) or adenocarcinoma, BAC subtype (n=89); the primary endpoint was response rate as determined by RECIST criteria.[85] Patients continued treatment until disease progression began or toxicity reached unacceptable levels. In this study, 25% of patients (n=26) had received prior chemotherapy one time. Erlotinib treatment resulted in an overall response rate of 22%, a median PFS of 4 months, and a median OS of 17 months. As in the S0126 trial, it was demonstrated that prior cytotoxic chemotherapy had no effect on clinical outcomes; similar response rates, PFS, and OS were seen in the untreated and previously treated groups (response rates, 27% and 21%, respectively; PFS, 4 months in both groups; OS, 16 months and 17 months, respectively). Clinical variables associated with improved survival included prior resection for BAC (P=.02), performance status of 90 or greater (P < .01), and no prior weight loss (P < .01). In addition, a correlative molecular analysis was performed on 82 of the 101 patients, including EGFR mutation testing by polymerase chain reaction (PCR), chromogenic in situ hybridization (CISH), IHC, and K-ras mutation testing by PCR. While the response rate and PFS were significantly more pronounced in patients who harbored the EGFR mutation than in those with EGFR wild type (response rate, 83% vs 7%, P < .01; PFS, 13 months vs 2 months, P < .01), there was no significant difference in OS between these two groups (23 months vs 17 months, P=.65). Not surprisingly, patients with K-ras mutations had a response rate of 0%. A multivariate analysis performed on these molecular predictors demonstrated the EGFR mutation to be the strongest predictor of both response rate and PFS (P < .001).
In the final study evaluating TKIs in BAC, 88 chemotherapy-nave patients with advanced or recurrent BAC were treated with gefinitib, 250 mg, until disease progression began or toxicity reached unacceptable levels (IFCT-0401).[86] The primary objective of this study was assessment of disease control rate (objective response + stable disease) at 3 months, using WHO criteria for response. Treatment with gefitinib resulted in a 3-month disease control rate of 29.4% and median PFS and OS of 2.9 months and 13.2 months, respectively. In a multivariate analysis, clinical characteristics consistently associated with improved clinical outcomes (3-month disease control rate, PFS, and OS) were a low respiratory symptom score (RSS) at inclusion (RSS less than 9), nonmucinous BAC, and development of rash during treatment. More specifically, median PFS and OS were significantly and dramatically prolonged in patients with nonmucinous BAC compared with patients with mucinous BAC (PFS, 11.3 months vs 2.6 months, P=.002; OS, 32.7 months vs 10.1 months, P=.0007). Treatment was generally well tolerated, with grade 3-4 toxicity limited to rash (4.6%), asthenia (1.1%), pulmonary symptoms (1.1%), and transaminitis (2.3%).
In an alternative approach to targeting of the EGFR pathway in advanced BAC, 41 highly pretreated patients with histologically confirmed BAC or adenocarcinoma with BAC features received a loading dose of cetuximab, 400 mg/m2, followed by weekly cetuximab, 250 mg/m2 until disease progression.[87] Most patients in this cohort had received some form of prior therapy (chemotherapy, 24%; radiotherapy, 5%; and surgery, 71%). The primary endpoint of response rate was achieved in 7% of patients, suggesting marginal clinical activity of cetuximab compared with gefitinib or erlotinib. Median PFS and OS were 3.2 months and 13 months, respectively. Molecular analysis was performed on 33 patient samples, and of the 9 patients with the EGFR mutation, only 1 had an objective response. Interestingly, 2 of 8 patients with the K-ras mutation had an objective response. Skin rash was the most common toxicity (any grade, 71%; grade of 3 or higher, 15%), and hypomagnesemia was noted in 26%.
In summary, while the incidence of BAC is increasing, there remains a lack of prospective data on agents that are potentially clinically active against this disease. Thus far, seven phase II studies, two utilizing paclitaxel and five exploiting the EGFR pathway (with erlotinib, gefitinib, or cetuximab), have generated varying response rates and survival times. Importantly, most of these trials have identified both molecular and clinical predictors that are associated with improved outcomes; these findings demonstrate the need to further define the complex pathophysiology of BAC in this era of targeted therapy. Many outstanding questions remain regarding the optimal treatment of this disease.
Discussion
With a firmer understanding of the molecular-genetic landscape of lung cancer, multiple advances have recently been made in the treatment of NSCLC, resulting in the development of effective novel targeted and chemotherapeutic agents. Whether these strategies can cross over into the treatment paradigm for BAC has yet to be validated prospectively, and a consideration of these strategies highlights several therapeutic challenges in this disease. Perhaps one of the most salient issues in the treatment of NSLCL is the importance of EGFR testing in those patients more likely to harbor the mutation based on clinical criteria (Asian, female, nonsmoker, adenocarcinoma). Recently, four large phase III trials comparing front-line gefitinib to platinum chemotherapy in advanced NSLCL demonstrated a dramatically higher response rate and greater PFS with gefitinib in those patients harboring the EGFR mutation.[6-8] Data from these trials and the high response rate demonstrated in the phase II trials reviewed here constitutes strong evidence supporting front-line treatment with a TKI in patients with BAC who harbor the EGFR mutation.
Reference Guide
Therapeutic Agents
Mentioned in This Article
Cetuximab (Erbitux)
Erlotinib (Tarceva)
Gefitinib (Iressa)
Gemcitabine (Gemzar)
Paclitaxel
Pemetrexed (Alimta)
Brand names are listed in parentheses only if a drug is not available generically and is marketed as no more than two trademarked or registered products. More familiar alternative generic designations may also be included parenthetically.
However, the approach to those patients whose BAC tumors are EGFR wild type-or in the common scenario in which mutational status is unknown or untested-remains a therapeutic dilemma. Perhaps the first question in these clinical scenarios is whether treatment with a TKI should be abandoned altogether. To evaluate this question, two points need to be considered. First, retrospective assessment from the study performed by Miller and colleagues demonstrated a response rate of 8% in those patients with wild-type EGFR who were treated with erlotinib,[85] which is not dramatically different from the rates demonstrated in the studies by West and Scagliotii that used IV paclitaxel (14% and 11%, respectively).[76,77] These results suggest that those patients with no detectable EGFR mutation may still benefit from treatment with a TKI; moreover, this notion is supported by several lines of research that demonstrate that EGFR wild type tumors may rely on alternate EGFR signaling pathways.[88] This concept has subsequently been reinforced in two large phase III studies demonstrating the clinical utility of erlotinib in the second-line and maintenance settings, independent of mutational status.[89,90]
The second point that needs to be addressed is the role of cytotoxic chemotherapy in BAC. While it is established that platinum chemotherapy remains a front-line standard treatment for fit patients with advanced NSCLC, there has not yet been a prospective study evaluating platinum chemotherapy in BAC or admixed BAC with adenocarcinoma. Interestingly, retrospective data from the sentinel ECOG 1594 study demonstrated a response rate of 6% to platinum chemotherapy in those patients with BAC.[74] Again, this is a rate not that different from the rates seen in the patients with EGFR wild type tumors who were treated with erlotinib in the trial by Miller (8%), or the rates in the two studies in which IV paclitaxel was used (14% and 11%). While the data are limited, it seems reasonable, based on the similar response rates, to consider erlotinib, platinum doublet chemotherapy, or single agent chemotherapy as first-line treatment options for those patients with unresectable BAC with a negative or unknown mutation status. Fortunately, further histological discrimination of these tumors may help guide treatment decisions and may introduce watchful waiting into the treatment paradigm.
Perhaps as important as the EGFR mutation assessment in the treatment of these patients is the pathological distinction of mucinous vs nonmucinous BAC. It has been consistently demonstrated in the trials reviewed here that these two histological subtypes have divergent clinical outcomes that may be reflective of their molecular signatures. The differing responses of these sub-histologies to paclitaxel are supported by the preclinical finding that human lung cancer cell lines that harbor EGFR mutations, which appear to be found exclusively in nonmucinous BAC, have pronounced resistance to both cisplatin and taxane chemotherapy.[91] Similarly, both the SWOG 0216 and IFTC-0401 trials demonstrated marked disparities in outcomes (response rate, PFS, and OS) between mucinous and nonmucinous BAC treated with gefitinib. This was most dramatically demonstrated in the more recent IFTC-0401 trial, in which the OS in patients with nonmucinous BAC was 32.7 months, compared with 10.1 months in patients with mucinous BAC. These results suggest that the presence of the EGFR mutation that is found exclusively in nonmucinous histologies may be the underlying predictor of the divergent clinical outcomes.
FIGURE 3

Unresectable/Multifocal BAC Treatment Algorithm
Given the selective responses to both TKIs and paclitaxel and the disparate clinical outcomes demonstrated with these agents, the assessment of both EGFR mutation status and sub-histology should be integrated into the treatment paradigm for patients with unresectable BAC. In making this recommendation, we recognize that prospective data remain limited and that these pathological assessments are not yet standardized. While treatment for patients with tumors that are EGFR mutation–positive seems straightforward, the authors believe that those patients with tumors that are EGFR wild type or of unknown mutation status should be further subdivided into those with mucinous and nonmucinous disease (Figure 3). For patients with unresectable mucinous BAC, we believe platinum doublet chemotherapy should be utilized in those patients who are candidates, despite the lack of prospective evidence. Although BAC is commonly perceived as an indolent tumor, the data suggest that this may be true only for nonmucinious histologies or admixed variants (see below); thus, mucinous BAC should be treated as aggressively as possible since the median survival for that entity is just over one year in most series. Treatment of nonmucinous histologies that are EGFR wild type or of unknown mutation remains a therapeutic challenge. The authors believe that erlotinib, single agent or platinum doublet chemotherapy, as well watchful waiting all are options for consideration, and that the selection should be contingent on such factors as clinical presentation and performance status.
Finally, considering that up to 80% of BAC presents admixed with adenocarcinoma, this pathologically defined subtype warrants discussion. While the surgical literature demonstrates that the presence of any BAC feature predicts improved survival, compared stage-for-stage with pure adenocarcinoma,[9,20,64,92-94] it is still unknown whether a higher proportion of BAC in an admixed tumor portends a better outcome than a lower proportion of BAC. As with the literature on pure BAC, there are very few prospective data addressing this subtype. Although treatment should be a factor in the potentially indolent nature of this histological subtype, it is our recommendation that treatment be consistent with that of advanced stage adenocarcinoma, per National Comprehensive Cancer Network guidelines.
As we usher in a new era of research into the specific signaling pathways and molecular determinants of cancer growth, we look forward to the identification of additional biomarkers that will result in more targeted approaches to the treatment of BAC. It is our hope that focused research into this subtype of adenocarcinoma will result in advances similar to those seen recently in NSCLC and will clarify the many outstanding questions related to the treatment of this disease.
Financial Disclosure: Dr. Levy receives speaker’s honoraria from Eli Lilly, Genentech, and Response Genetics. Drs. Drilon, Makarian, Patel, and Grossbard have no significant financial interests or other relationships to disclose.
References:
References
1. Barkley JE, Green MR. Bronchioloalveolar carcinoma. J Clin Oncol. 1996;14:2377-86.
2. Liebow A. Bronchiolo-alveolar carcinoma. Adv Intern Med. 1960;10:329-58.
3. Travis WD, Colby TV, Corrin B, et al., editors. Histological typing of lung and pleural tumors. 3rd ed. Berlin: Springer-Verlag; 1999.
4. Raz DJ, He B, Rosell R, Jablons DM. Bronchioloalveolar carcinoma: a review. Clin Lung Cancer. 2006;7:313-22.
5. Travis WD, editor. World Health Organization, International Agency for Research on Cancer, international Association for the Study of Lung Cancer, International Academy of Pathology. Pathology and Genetics of Tumours of the Lung, Pleura, Thymus and Heart. Lyon Oxford: IARC Press, Oxford University Press; 2004.
6. Mok TS, Wu YL, Thongprasert S, et al. Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N Engl J Med. 2009;361:947-57.
7. Inoue A, Kobayashi K, Usui K, et al. First-line gefitinib for patients with advanced non-small-cell lung cancer harboring epidermal growth factor receptor mutations without indication for chemotherapy. J Clin Oncol. 2009;27:1394-400.
8. Mitsudomi T, Morita S, Yatabe Y, et al. Gefitinib versus cisplatin plus docetaxel in patients with non-small-cell lung cancer harbouring mutations of the epidermal growth factor receptor (WJTOG3405): an open label, randomised phase 3 trial. Lancet Oncol. 2010;11:121-8.
9. Noguchi M, Morikawa A, Kawasaki M, et al. Small adenocarcinoma of the lung. Histologic characteristics and prognosis. Cancer. 1995;75:2844-52.
10. Garfield DH, Cadranel J. The importance of distinguishing mucinous and nonmucinous bronchioloalveolar carcinomas. Lung. 2009;187:207-8.
11.West H. Emerging approaches to advanced bronchioloalveolar carcinoma. Curr Treat Options Oncol. 2006;7:69-76.
12. Moran CA. Pulmonary adenocarcinoma: the expanding spectrum of histologic variants. Arch Pathol Lab Med. 2006;130:958-62.
13. Yousem SA, Beasley MB. Bronchioloalveolar carcinoma: a review of current concepts and evolving issues. Arch Pathol Lab Med. 2007;131:1027-32.
14. Finberg KE, Sequist LV, Joshi VA, et al. Mucinous differentiation correlates with absence of EGFR mutation and presence of KRAS mutation in lung adenocarcinomas with bronchioloalveolar features. J Mol Diagn. 2007;9:320-6.
15. Ebright MI, Zakowski MF, Martin J, et al. Clinical pattern and pathologic stage but not histologic features predict outcome for bronchioloalveolar carcinoma. Ann Thorac Surg. 2002;74:1640-6; discussion 6-7.
16. Yokose T, Suzuki K, Nagai K, et al. Favorable and unfavorable morphological prognostic factors in peripheral adenocarcinoma of the lung 3 cm or less in diameter. Lung Cancer. 2000;29:179-88.
17. Suzuki K, Yokose T, Yoshida J, et al. Prognostic significance of the size of central fibrosis in peripheral adenocarcinoma of the lung. Ann Thorac Surg. 2000;69:893-7.
18. Sakurai H, Maeshima A, Watanabe S, et al. Grade of stromal invasion in small adenocarcinoma of the lung: histopathological minimal invasion and prognosis. Am J Surg Pathol. 2004;28:198-206.
19. Yim J, Zhu LC, Chiriboga L, et al. Histologic features are important prognostic indicators in early stages lung adenocarcinomas. Mod Pathol. 2007;20:233-41.
20. Terasaki H, Niki T, Matsuno Y, et al. Lung adenocarcinoma with mixed bronchioloalveolar and invasive components: clinicopathological features, subclassification by extent of invasive foci, and immunohistochemical characterization. Am J Surg Pathol. 2003;27:937-51.
21. Dacic S. Minimally invasive adenocarcinomas of the lung. Adv Anat Pathol. 2009;16:166-71.
22. Travis WD GK, Franklin W. Bronchioloalveolar carcinoma and lung adenocarcinoma: the clinical importance and research relevance of the 2004 World Health Organization pathologic criteria. Journ Thorac Oncol. 2006;1:S13-S9.
23. Kim CF, Jackson EL, Woolfenden AE, et al. Identification of bronchioalveolar stem cells in normal lung and lung cancer. Cell. 2005;121:823-35.
24. Besson A, Hwang HC, Cicero S, et al. Discovery of an oncogenic activity in p27Kip1 that causes stem cell expansion and a multiple tumor phenotype. Genes Dev. 2007;21:1731-46.
25. Yanagi S, Kishimoto H, Kawahara K, et al. PTEN controls lung morphogenesis, bronchioalveolar stem cells, and onset of lung adenocarcinomas in mice. J Clin Invest. 2007; 117:2929-40.
26. Dacic S, Finkelstein SD, Yousem SA. Clonal selection of adenocarcinoma of the lung as determined by loss of heterozygosity. Exp Mol Pathol. 2005;78:135-9.
27. Sasatomi E, Johnson LR, Aldeeb DN, et al. Genetic profile of cumulative mutational damage associated with early pulmonary adenocarcinoma: bronchioloalveolar carcinoma vs stage I invasive adenocarcinoma. Am J Surg Pathol. 2004;28:1280-8.
28. Yamasaki M, Takeshima Y, Fujii S, et al. Correlation between morphological heterogeneity and genetic alteration within one tumor in adenocarcinomas of the lung. Pathol Int. 2000;50:891-6.
29. Wislez M, Beer DG, Wistuba I, et al. Molecular biology, genomics, and proteomics in bronchioloalveolar carcinoma. J Thorac Oncol. 2006;1(9 Suppl):S8-12.
30. Riely GJ, Marks J, Pao W. KRAS mutations in non-small cell lung cancer. Proc Am Thorac Soc. 2009;6:201-5.
31. Bianchi F, Nicassio F, Di Fiore PP. Unbiased vs biased approaches to the identification of cancer signatures: the case of lung cancer. Cell Cycle. 2008;7:729-34.
32. Garfield DH, Cadranel J, West HL. Bronchioloalveolar carcinoma: the case for two diseases. Clin Lung Cancer. 2008;9:24-9.
33. Marchetti A, Martella C, Felicioni L, et al. EGFR mutations in non-small-cell lung cancer: analysis of a large series of cases and development of a rapid and sensitive method for diagnostic screening with potential implications on pharmacologic treatment. J Clin Oncol. 2005;23:857-65.
34. Sakuma Y, Matsukuma S, Yoshihara M, et al. Distinctive evaluation of nonmucinous and mucinous subtypes of bronchioloalveolar carcinomas in EGFR and K-ras gene-mutation analyses for Japanese lung adenocarcinomas: confirmation of the correlations with histologic subtypes and gene mutations. Am J Clin Pathol. 2007;128:100-8.
35. Hirsch FR, Herbst RS, Olsen C, et al. Increased EGFR gene copy number detected by fluorescent in situ hybridization predicts outcome in non-small-cell lung cancer patients treated with cetuximab and chemotherapy. J Clin Oncol. 2008;26:3351-7.
36. Erman M, Grunenwald D, Penault-Llorca F, et al. Epidermal growth factor receptor, HER-2/neu and related pathways in lung adenocarcinomas with bronchioloalveolar features. Lung Cancer. 2005;47:315-23.
37. Wang C, Yang R, Yue D, Zhang Z. Expression of FAK and PTEN in bronchioloalveolar carcinoma and lung adenocarcinoma. Lung. 2009;187:104-9.
38. Trigaux JP, Gevenois PA, Goncette L, et al. Bronchioloalveolar carcinoma: computed tomography findings. Eur Respir J. 1996;9:11-6.
39. Bonomo L, Storto ML, Ciccotosto C, et al. Bronchioloalveolar carcinoma of the lung. Eur Radiol. 1998;8:996-1001.
40. Sabloff BS, Truong MT, Wistuba II, Erasmus JJ. Bronchioalveolar cell carcinoma: radiologic appearance and dilemmas in the assessment of response. Clin Lung Cancer. 2004;6:108-12.
41. Gandara DR, Aberle D, Lau D, et al. Radiographic imaging of bronchioloalveolar carcinoma: screening, patterns of presentation and response assessment. J Thorac Oncol. 2006;1(9 Suppl):S20-6.
42. Raz DJ, Kim JY, Jablons DM. Diagnosis and treatment of bronchioloalveolar carcinoma. Curr Opin Pulm Med. 2007;13:290-6.
43. Kuriyama K, Seto M, Kasugai T, et al. Ground-glass opacity on thin-section CT: value in differentiating subtypes of adenocarcinoma of the lung. AJR Am J Roentgenol. 1999;173:465-9.
44. Matsugama H. Proportion of ground-glass opacity on high-resolution compted tomography in clinical T1 N0 M0 adenocarcinoma of the lung a predictor of lymph node metastasis. J Thoracic Cardiovasc Surg. 2002;124:221-2.
45. Nakata M, Sawada S, Saeki H, et al. Prospective study of thoracoscopic limited resection for ground-glass opacity selected by computed tomography. Ann Thorac Surg. 2003;75:1601-5; discussion 5-6.
46. Nakamura H, Saji H, Ogata A, et al. Lung cancer patients showing pure ground-glass opacity on computed tomography are good candidates for wedge resection. Lung Cancer. 2004;44:61-8.
47. Travis WD, Garg K, Franklin WA, et al. Evolving concepts in the pathology and computed tomography imaging of lung adenocarcinoma and bronchioloalveolar carcinoma. J Clin Oncol. 2005;23:3279-87.
48. Patsios D, Roberts HC, Paul NS, et al. Pictorial review of the many faces of bronchioloalveolar cell carcinoma. Br J Radiol. 2007;80:1015-23.
49. Shah RM, Balsara G, Webster M, Friedman AC. Bronchioloalveolar cell carcinoma: impact of histology on dominant CT pattern. J Thorac Imaging. 2000;15:180-6.
50. Jung JI, Kim H, Park SH, et al. CT differentiation of pneumonic-type bronchioloalveolar cell carcinoma and infectious pneumonia. Br J Radiol. 2001;74:490-4.
51. Im JG, Han MC, Yu EJ, et al. Lobar bronchioloalveolar carcinoma: “angiogram sign” on CT scans. Radiology. 1990;176:749-53.
52. Akira M, Atagi S, Kawahara M, et al. High-resolution CT findings of diffuse bronchioloalveolar carcinoma in 38 patients. AJR Am J Roentgenol. 1999;173:1623-9.
53. Aquino SL, Halpern EF, Kuester LB, Fischman AJ. FDG-PET and CT features of non-small cell lung cancer based on tumor type. Int J Mol Med. 2007;19:495-9.
54. Sun JS, Park KJ, Sheen SS, et al. Clinical usefulness of the fluorodeoxyglucose (FDG)-PET maximal standardized uptake value (SUV) in combination with CT features for the differentiation of adenocarcinoma with a bronchioloalveolar carcinoma from other subtypes of non-small cell lung cancers. Lung Cancer. 2009;66:205-10.
55. Heyneman LE, Patz EF. PET imaging in patients with bronchioloalveolar cell carcinoma. Lung Cancer. 2002;38:261-6.
56. Yap CS, Schiepers C, Fishbein MC, et al. FDG-PET imaging in lung cancer: how sensitive is it for bronchioloalveolar carcinoma? Eur J Nucl Med Mol Imaging. 2002;29:1166-73.
57. Wang Y. FDG-PET in bronchial alveolar carcinoma. Chinese-German J Clin Oncol. 2006;5:P54-P7.
58. Tanaka R, Horikoshi H, Nakazato Y, et al. Magnetic resonance imaging in peripheral lung adenocarcinoma: correlation with histopathologic features. J Thorac Imaging. 2009;24:4-9.
59. Ohno Y, Hatabu H, Takenaka D, et al. Dynamic MR imaging: value of differentiating subtypes of peripheral small adenocarcinoma of the lung. Eur J Radiol. 2004;52:144-50.
60. Fujimoto K. Usefulness of contrast-enhanced magnetic resonance imaging for evaluating solitary pulmonary nodules. Cancer Imaging. 2008;8:36-44.
61. Dumont P, Gasser B, Rouge C, et al. Bronchoalveolar carcinoma: histopathologic study of evolution in a series of 105 surgically treated patients. Chest. 1998;113:391-5.
62. Carretta A, Canneto B, Calori G, et al. Evaluation of radiological and pathological prognostic factors in surgically-treated patients with bronchoalveolar carcinoma. Eur J Cardiothorac Surg. 2001;20:367-71.
63. Liu YY, Chen YM, Huang MH, Perng RP. Prognosis and recurrent patterns in bronchioloalveolar carcinoma. Chest. 2000;118:940-7.
64. Furak J, Trojan I, Szoke T, et al. Bronchioloalveolar lung cancer: occurrence, surgical treatment and survival. Eur J Cardiothorac Surg. 2003;23:818-23.
65. Laskin J SA, Johnson D. Redefining Bronchioloalveolar Carcinoma. Seminars in Oncology. 2005;32:329-35.
66. Barlesi F, Doddoli C, Thomas P, et al. Bilateral bronchioloalveolar lung carcinoma: is there a place for palliative pneumonectomy? Eur J Cardiothorac Surg. 2001;20:1113-6.
67. Christiani DC, Pao W, DeMartini JC, et al. BAC consensus conference, November 4-6, 2004: epidemiology, pathogenesis, and preclinical models. J Thorac Oncol. 2006;1(9 Suppl):S2-7.
68. Regnard JF, Santelmo N, Romdhani N, et al. Bronchioloalveolar lung carcinoma: results of surgical treatment and prognostic factors. Chest. 1998;114:45-50.
69. Rena O, Papalia E, Ruffini E, et al. Stage I pure bronchioloalveolar carcinoma: recurrences, survival and comparison with adenocarcinoma of the lung. Eur J Cardiothorac Surg. 2003;23:409-14.
70. Roberts PF, Straznicka M, Lara PN, et al. Resection of multifocal non-small cell lung cancer when the bronchioloalveolar subtype is involved. J Thorac Cardiovasc Surg. 2003;126:1597-602.
71. Atkins KA. The diagnosis of bronchioloalveolar carcinoma by cytologic means. Am J Clin Pathol. 2004;122:14-6.
72. Marchevsky AM, Changsri C, Gupta I, et al. Frozen section diagnoses of small pulmonary nodules: accuracy and clinical implications. Ann Thorac Surg. 2004;78:1755-9.
73. Miller DL, Rowland CM, Deschamps C, et al. Surgical treatment of non-small cell lung cancer 1 cm or less in diameter. Ann Thorac Surg. 2002;73:1545-50; discussion 50-1.
74. Schiller JH, Harrington D, Belani CP, Langer C, Sandler A, Krook J, et al. Comparison of four chemotherapy regimens for advanced non-small-cell lung cancer. N Engl J Med. 2002;346:92-8.
75. Duruisseaux M, Cadranel J, Biron E, et al. Major and prolonged response to pemetrexed in two cases of lung adenocarcinoma with bronchioloalveolar carcinoma features. Lung Cancer. 2009;65:385-7.
76. West HL, Crowley JJ, Vance RB, et al. Advanced bronchioloalveolar carcinoma: a phase II trial of paclitaxel by 96-hour infusion (SWOG 9714): a Southwest Oncology Group study. Ann Oncol. 2005;16:1076-80.
77. Scagliotti GV, Smit E, Bosquee L, et al. A phase II study of paclitaxel in advanced bronchioloalveolar carcinoma (EORTC trial 08956). Lung Cancer. 2005;50:91-6.
78. Fukuoka M, Yano S, Giaccone G, et al. Multi-institutional randomized phase II trial of gefitinib for previously treated patients with advanced non-small-cell lung cancer (The IDEAL 1 Trial) [corrected]. J Clin Oncol. 2003;21:2237-46.
79. Lynch TJ, Bell DW, Sordella R, et al. Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. N Engl J Med. 2004;350:2129-39.
80. Miller VA, Kris MG, Shah N, et al. Bronchioloalveolar pathologic subtype and smoking history predict sensitivity to gefitinib in advanced non-small-cell lung cancer. J Clin Oncol. 2004;22:1103-9.
81. Kris MG, Sandler A, Miller M, et al. Cigarette smoking history predicts sensitivity to erlotinib: results of a phase II trial in patients with bronchioloalveolar carcinoma (BAC) [abstract]. J Clin Oncol. 2004;145(July 15 Suppl):7062.
82. West HL, Franklin WA, McCoy J, et al. Gefitinib therapy in advanced bronchioloalveolar carcinoma: Southwest Oncology Group Study S0126. J Clin Oncol. 2006;24:1807-13.
83. Hirsch FR GD, McCoy J. Increased EGFR gene copy number detected by FISH is associated with increased sensitivity to gefitinib in patients in patients with bronchioloaveolar carcinoma (BAC)(S0126). J Clin Oncol. 2005;24(628s).
84. Franklin WA CK, Gumerlock PH. Association between activation of ErbB pathway genes and survival following gefitinib treatment in advanced BAC (SWOG 0126). Proc Amer Soc Cli Oncol. 2004;23(620s).
85. Miller VA, Riely GJ, Zakowski MF, et al. Molecular characteristics of bronchioloalveolar carcinoma and adenocarcinoma, bronchioloalveolar carcinoma subtype, predict response to erlotinib. J Clin Oncol. 2008;26:1472-8.
86. Cadranel J, Quoix E, Baudrin L, et al. IFCT-0401 Trial: a phase II study of gefitinib administered as first-line treatment in advanced adenocarcinoma with bronchioloalveolar carcinoma subtype. J Thorac Oncol. 2009;4:1126-35.
87. Ramalingam S, Lee J, Belani CP, et al. Cetuximab for the treatment of advanced bronchioloalveolar carcinoma (BAC): an Eastern Cooperative Oncology Group phase II study (ECOG 1504). J Clin Oncol. 2010;28(15s).
88. Bunn PA, Jr., Dziadziuszko R, Varella-Garcia M, et al. Biological markers for non-small cell lung cancer patient selection for epidermal growth factor receptor tyrosine kinase inhibitor therapy. Clin Cancer Res. 2006;12:3652-6.
89. Shepherd FA, Rodrigues Pereira J, Ciuleanu T, et al. Erlotinib in previously treated non-small-cell lung cancer. N Engl J Med. 2005;353:123-32.
90. Cappuzzo F, Ciuleanu T, Stelmakh L, et al. Erlotinib as maintenance treatment in advanced non-small-cell lung cancer: a multicentre, randomised, placebo-controlled phase 3 study. Lancet Oncol. 2010;11:521-9.
91. Sordella R, Bell DW, Haber DA, Settleman J. Gefitinib-sensitizing EGFR mutations in lung cancer activate anti-apoptotic pathways. Science. 2004;305:1163-7.
92. Higashiyama M, Kodama K, Yokouchi H, et al. Prognostic value of bronchiolo-alveolar carcinoma component of small lung adenocarcinoma. Ann Thorac Surg. 1999;68:2069-73.
93. Koga T, Hashimoto S, Sugio K, et al. Lung adenocarcinoma with bronchioloalveolar carcinoma component is frequently associated with foci of high-grade atypical adenomatous hyperplasia. Am J Clin Pathol. 2002;117:464-70.
94. Okubo K, Mark EJ, Flieder D, et al. Bronchoalveolar carcinoma: clinical, radiologic, and pathologic factors and survival. J Thorac Cardiovasc Surg. 1999;118:702-9.