Toripalimab Consolidation Improves Survival in Limited-Stage SCLC
In patients with LS-SCLC who were ineligible for a prophylactic cranial irradiation, toripalimab appeared to decrease the progression of brain metastases.
Topline efficacy data revealed that among patients who underwent treatment with toripalimab vs those who underwent observation following chemoradiation, the median OS was not reached vs 30.3 months, respectively.
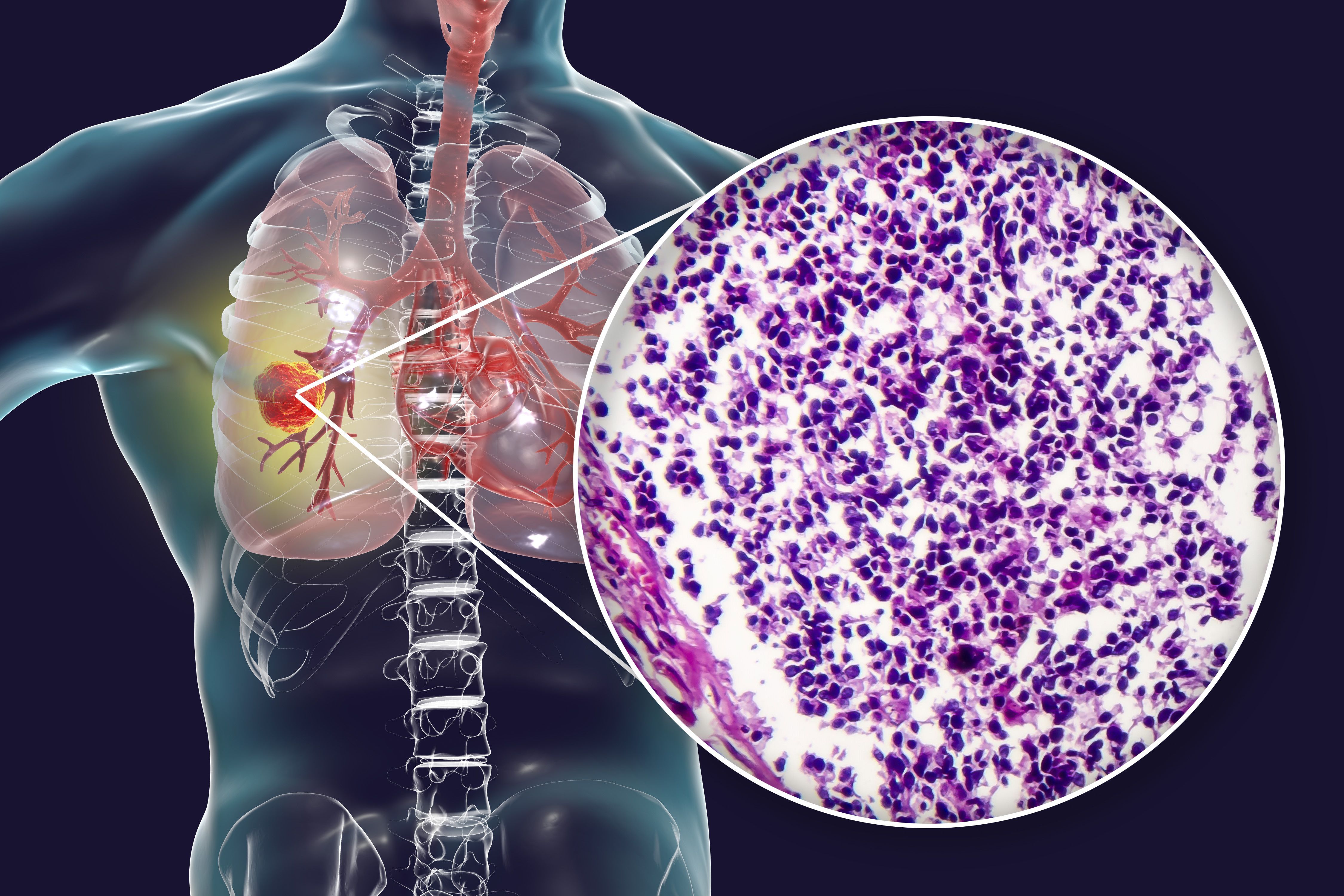
Toripalimab-tpzi (Loqtorzi) consolidation following chemoradiotherapy improved overall survival (OS) and progression-free survival (PFS) outcomes among patients with limited-stage small cell lung cancer (LS-SCLC), according to findings from the phase 2 GASTO-1052A trial (NCT04212052) presented at the IASLC 2025 World Conference on Lung Cancer.1
Topline efficacy data revealed that among patients who underwent treatment with toripalimab (n = 49) vs those who underwent observation following chemoradiation (n = 49), the median OS was not reached (NR) vs 30.3 months, respectively (HR, 0.41; 95% CI, 0.20-0.82; P = .012). Additionally, the 12- and 24-month rates were 93.7% vs 77.2% and 79.2% vs 59.1%. A subgroup analysis of OS revealed that patients who did not receive prior prophylactic cranial irradiation (PCI; HR, 0.17), those younger than 60 (HR, 0.18), those with an ECOG performance status of 1 (HR, 0.39), and those with stage III disease (HR, 0.40) experienced particular benefit with toripalimab consolidation.
Regarding median PFS, it was NR in the consolidation group vs 14.1 months (95% CI, 2.8-25.4) with observation (HR, 0.54; 95% CI, 0.31-0.94; P = .03). The respective 12- and 24-month values were 67.3% vs 50.7% and 57.0% vs 36.2%. A subgroup analysis for PFS revealed that patients who did not receive prior PCI (HR, 0.30), those younger than 60 (HR, 0.27), those with an ECOG performance status of 1 (HR, 0.47), and those with stage III disease (HR, 0.50) experienced particular benefit with toripalimab consolidation.
“Toripalimab consolidation post-[chemoradiotherapy] in patients with LS-SCLC significantly improved PFS and OS. The conditional power is 94.95% and the predictive power is 86.30% to detect a true HR of 0.548 at the final analysis,” study author PengXin Zhang, MD, of the Department of Radiation Oncology of Sun Yat-sen University Cancer Center in Guangzhou, China, wrote in the presentation with coinvestigators.1 “Toripalimab appears to potentially decrease brain metastasis progression among patients ineligible for PCI.”
Investigators in the phase 2 trial enrolled patients with unresectable LS-SCLC without disease progression following chemoradiotherapy and randomly assigned them 1:1 to undergo treatment with toripalimab consolidative therapy or observation. Patients were stratified by disease stage I/II or III and receipt of PCI. Toripalimab consisted of 240 mg every 3 weeks for a maximum of 6 months.
Additionally, chemotherapy with etoposide and cisplatin was dosed for 4 cycles, and radiation therapy consisted of 60 to 65 Gy over 24 to 26 fractions daily for 5 to 6 weeks. If eligible, patients received PCI within 6 weeks of the last chemoradiation dose and within 42 days of the first dose of toripalimab.
The median age in the consolidative and observation groups was 60 years (range, 29-79) and 60 years (range, 39-71), respectively. Patients were mostly male (both 85.7%), had an ECOG performance status of 1 (77.6% vs 79.6%), and had a history of smoking (89.8% vs 93.9%). A similar number of patients had stage III disease (both 91.8%) and received prior PCI (both 65.3%).
The primary end point of the study was PFS. Secondary end points included OS, objective response rate, and safety.
Of note, the randomized, controlled phase 2 GASTO-1052A trial was suspended following the publication of the phase 3 ADRIATIC trial (NCT03703297) results. Results from ADRIATIC were presented at the 2024 European Society for Medical Oncology Congress.2 The results supported the FDA approval of durvalumab in patients with LS-SCLC who have not progressed following concurrent platinum-based chemoradiation in December 2024.3
References
- Zhang P, Wang D, He W, et al. Toripalimab consolidation after chemoradiotherapy in limited-stage small cell lung cancer: a phase II, randomized controlled study (GASTO-1052A). Presented at the International Association for the Study of Lung Cancer World Conference on Lung Cancer 2025; September 6-9, 2025; Barcelona, Spain. Abstract 3956.
- Senan S, Spigel D, Cho BC, et al. Durvalumab as consolidation therapy in limited-stage SCLC (LS-SCLC): outcomes by prior concurrent chemoradiotherapy (cCRT) regimen and prophylactic cranial irradiation (PCI) use in the ADRIATIC trial. Presented at the 2024 European Society for Medical Oncology Congress (ESMO); September 13-17, 2024; Barcelona, Spain. Abstract LBA81.
- FDA approves durvalumab for limited-stage small cell lung cancer. News release. FDA. December 4, 2024. Accessed September 15, 2025. https://shorturl.at/0eID1