Trial Heralding a ‘New Day’ for Melanoma Meets with Guarded Enthusiasm
Ipilimumab has being lauded as a monumental advance in the field of immuno-oncology. While the news is certainly promising, unanswered questions remain and the melanoma community must proceed with caution.
ABSTRACT: Ipilimumab has being lauded as a monumental advance in the field of immuno-oncology. While the news is certainly promising, unanswered questions remain and the melanoma community must proceed with caution.
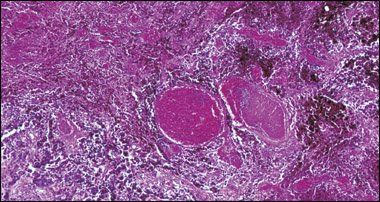
Photomicrograph of metastatic malignant melanoma in the human lymph node, section, H&E stain, magnified 10× at 24 × 36 mm.
©Carolina Biological Supply Company/PhototakeUSA.com
For a disease that is most closely linked to the sun, melanoma has seen some very dark days-the last approval for a treatment regimen, interleukin-2, took place nearly 12 years ago. Since then, multiple trials have been conducted with new agents or combination therapies and the results have been mostly dismal (J Clin Oncol 26:527-534, 2008).
When a new trial offered more than a ray of hope in melanoma therapy, it was no surprise that the spotlight shone with full force: The phase III MDX010-20 trial, which tested ipilimumab (see Fact box on page 20) and a gp100 peptide vaccine in metastatic melanoma, landed a coveted spot in an ASCO 2010 plenary session, with the results published simultaneously in the New England Journal of Medicine online (June 5, 2010; updated on June 14, 2010).

STEVEN O'DAY, MD
"I feel that I'm presenting [these data] not only for my co-investigators but also for the clinicians who have worked in this disease over the many decades as we've faced great disappointment. But finally we are getting good news," said lead investigator Steven O'Day, MD, during his plenary session address (abstract 4).
The excitement generated by the results extended beyond the ASCO meeting, with mass media spreading the word like sunshine: A "cure" for melanoma had been discovered.
"I've already gotten dozens of requests for this drug," said Sanjiv Agarwala, MD, chief of hematology and oncology at St. Luke's Hospital and Health Network in Bethlehem, Penn. "We are going to have a compassionate use program here soon [for this drug] and there's already a waiting list. But what's interesting is that when people talk to me about this, they say 'There's been a new drug approved for melanoma' or 'There's a cure for melanoma,' and I have to point out that nothing has been approved yet and that it's not a cure" (see Vantage Point).
While there's no doubt that the MDX010-20 trial is a major breakthrough, is it a breakthrough of epic proportions? Oncology News International spoke with experts who concurred that the results are quite meaningful-but only to a point.
"Before we say 'Aha, we've got it,' we have to look at the limitations of this study. . .while an important advance, it opens up more questions than it resolves," said Lee Cranmer, MD, PhD, an assistant professor of clinical medicine at the University of Arizona in Tucson.
VANTAGE POINT

SANJIV AGARWALA, MD 'A base hit but not a home run'
Results from the MDX010-20 trial are certainly a step in the right direction, Dr. Agarwala said. "It's a base hit but not a home run. This drug benefits a subset of patients, about 10% of melanoma patients overall I would say, and, again, it's a good step."
The results will change the landscape for future melanoma trials as other drugs will have to be compared to ipilimumab, added Dr. Agarwala, principal investigator for a phase II trial of PV-10 in metastatic melanoma (see Related Reading, at left).
Dr. Agarwala also participated in and was principal investigator for the phase III PRISM trial, which evaluated sorafenib (Nexavar) with carboplatin and paclitaxel as second-line treatment in advanced melanoma patients (J Clin Oncol 27:2823-2830, 2009).
There's still plenty of work that needs to be done in terms of combining ipilimumab with other agents, sequencing, and dosing, he said. "With these ipilimumab results, we now have another treatment option for our patients, but that that doesn't mean that every person with melanoma who walks through the door is going to get this drug and will be cured."
Trial results
TABLE 1 MDX010-20 trial Rx arms Arm 1: ipilimumab (3 mg/kg q3w × 4 doses) plus gp100 vaccine peptides 209-217 [210M] and 280-288 [288V] (1 mg q3w × 4 doses)
Arm 2: ipilimumab plus placebo
Arm 3: gp100 vaccine plus placebo
Dr. O'Day and colleagues found that in pretreated patients with metastatic melanoma, ipilimumab improved overall survival (OS), although combining ipilimumab with the gp100 vaccine did not provide an additional survival benefit. Dr. O'Day is the chief of research and director of the melanoma program at The Angeles Clinic and Research Institute in Santa Monica, Calif.
Dr. O'Day noted that the global incidence of metastatic melanoma is rising rapidly and that there are no approved therapies for pretreated patients. Prognosis is poor in metastatic melanoma patients, with a one-year survival of about 25% and a two-year survival of about 10%.
Phase II trials of ipilimumab monotherapy have shown 20% to 30% durable disease control and two-year survival. Dr. O'Day underscored also that ipilimumab's immune system activation does produce side effects. They occur usually in the first 12 weeks of treatment, most commonly affecting the skin and colon, and less frequently the liver and pituitary gland. Such side effects may require vigilant follow up and early steroid use, Dr. O'Day said.
TABLE 2 One-year and two-year survival rates
In the phase III, double-blind, multicenter trial (125 centers in 13 countries), 676 patients (mean age, 66) with unresectable stage III/IV melanoma were randomized 3:1:1 to three treatment arms (see Table 1). The gp100 vaccine, an experimental melanoma peptide vaccine designed to stimulate T-cell attacks on melanoma cells, has been shown previously to have modest but promising anticancer activity. OS was the trial's primary endpoint.
According to the results, the hazard ratio (HR) for survival as compared with gp100 alone was reduced by 32% for arm 1 (HR 0.68; P = .0004) and by 34% for arm 2 (HR 0.66; P = .0026). Median overall survival was 10 months for arm 1, 10.1 months for arm 2, and 6.4 months for arm 3. One- and two-year survival rates also favored the protocol used in arm 2 (see Table 2).
Rose bengal stain shows promise in melanoma
In the form of PV-10, rose bengal, a sodium salt stain that has been used for wool dying, liver imaging, and in eye drops, has demonstrated an ability to elicit selective chemoablation. Dr. Sanjiv Agarwala led a phase II trial of 80 subjects with stage III-IV melanoma (cutaneous, subcutaneous, or nodal lesions) treated with a single injection of PV-10 initially with re-treatment when appropriate.
According to the results in the first 40 subjects, PV-10 was delivered to 486 lesions. The adverse events were mild to moderate, with the most common being pain at the treatment site (82% of the patients). There were no grade 4-5 adverse events attributed to PV-10. Among the 40 subjects, 33% achieved complete response. In all subjects, the mean progression-free survival was 8.5 months (ASCO 2010 abstract 8534).
"It's an intratumoral injection and that needs to be done in patients with accessible tumors," Dr. Agarwala explained. "This is early work and we're looked at the response in injected lesions and bystander lesions. We don't know the response of the entire body and how the drug affects visceral disease. We think it has a systemic immune effect. It's an agent that is possibly waking up the immune system some way."
Dr. Agarwala said that PV-10 would be a good adjunct to other immunotherapies. "I would love to see a trial combining PV-10 with ipilimumab. There may be some synergy," he said. "The main advantage of PV-10 is that it's very easy. The median age of the patients in our trial was 70 and that's not the kind of group that can receive aggressive therapy."
Provectus Pharmaceuticals is currently in talks with the FDA to design a phase III trial for PV-10, he added.
The trouble with toxicity
In the trial, treatment-related adverse events were more common in patients receiving ipilimumab. Treatment-related deaths were reported at rates of 2.1% for arm 1; 3.1% for arm 2; and 1.5% for arm 3. Grade 3-4 related adverse events were reported at rates of 17.4% for arm 1, 22.9% for arm 2, and 11.4% for arm 3.
Immune-related adverse events were reported in about 60% of patients receiving ipilimumab and in about 30% of those receiving only gp100.
"Overall, ipilimumab was very well tolerated," Dr. O'Day told Oncology News International. "The vast majority of side effects were grade 1-2, and [these] were managed quite rapidly. Ten percent to 14% were more severe and required that the drug be stopped and high-dose steroids initiated-almost always successfully." He added that while there was some correlation between patients experiencing side effects and response to ipilimumab, the correlation was not absolute; some patients without side effects still responded to treatment.
"It is a drug that needs to be monitored closely, but the risk trade-off is strongly in favor of the drug's benefit," he said. Our experts agreed, but with some caveats.
Treatment with ipilimumab requires a committed, multidisciplinary team to track adverse events, said Vernon Sondak, MD, chair of the cutaneous oncology department at H. Lee Moffitt Cancer Center & Research Institute in Tampa, Fla. However, "a trained oncologist with an experienced team can manage this toxicity if they are careful, thorough, and aggressive" (see Vantage Point).
Educating advanced melanoma patients and physicians-particularly those who see these patients in an emergency setting-about the toxicity associated with ipilimumab is vital, Dr. Cranmer said.
"Just because it is immunotherapy, doesn't mean it is nontoxic. Actually, there are some very unusual and occasionally life-threatening toxicities with ipilimumab therapy. . .the most critical one is the development of a syndrome that looks like ulcerative colitis. And this can be associated with perforation of the bowel. . .indeed there were several bowel perforations reported in this particular study," he said. Dr. Cranmer acknowledged that treatment with corticosteroid therapy as an immunosuppressive antidote does generally work.
VANTAGE POINT

VERNON K. SONDAK, MD Clinical trials remain best treatment option for melanoma patients
For the last few years, those of us in the melanoma business have felt like we were in a long, dark tunnel, Dr. Sondak said, "a tunnel with no documented improvement in survival for metastatic melanoma patients over the past three decades and no new FDA-approved drugs. That has left us in a situation where first-line therapy has been of questionable value over supportive care and there is no established second-line therapy whatsoever-and no proof in the value of combining any of the marginal or ineffective agents that we have."
As a result, virtually all national and international guidelines for metastatic melanoma have come to the same conclusion: The treatment of choice is participation in a clinical trial, added Dr. Sondak, who is a professor in the departments of oncologic sciences and surgery at Tampa's University of South Florida College of Medicine.
Do the results of MDX010-20 mean those guidelines will have to be revised? Yes and no.
"For the first time, we can say there was a documented improvement in survival in a phase III trial," Dr. Sondak pointed out.
For overall survival, the results clearly favored both ipilimumab-containing arms, he said, while the overall progression-free survival also supported the two ipilimumab arms over the gp100 control.
"Perhaps we'll soon hear that this drug was approved by the FDA," he said.
"But we'll still be left with uncertainties about whether this is a first-line or second-line drug; we still won't know how to combine these drugs, and we will still have to conclude that the best treatment for our patients is a clinical trial."
Vaccine: More harm than good?
Immunotherapy has been tested in melanoma more than any other tumor type. But did the addition of the vaccine in this study really offer any benefit? Our experts were divided.

A Second Opinion
"We have not had any therapy that has prolonged survival for patients with stage IV melanoma, period," said Lynn Schuchter, MD, leader of the melanoma program at the Abramson Cancer Center, University of Pennsylvania, in Philadelphia. "So to show this kind of benefit in this randomized, large clinical trial is really a step forward. We will be able to build on these results with other combinations of immunotherapy."
"It is interesting that there was no clear difference between ipilimumab and ipilimumab plus vaccine," said Jennifer A. Wargo, MD, from the surgical oncology division at Boston's Massachusetts General Hospital.
Was gp100 the right control for this study, Dr. Sondak asked. "It was reasonable because there is no standard therapy for stage IV melanoma patients who have failed additional treatment, mostly single-agent chemotherapy," he explained. "On the other hand, gp100 could have been harmful. At the very least, it's disappointing and unexplained why the ipilimumab plus gp100 arm was no better than the ipilimumab-alone arm."
FACT Ipilimumab basics Ipilimumab is a human monoclonal antibody directed against CTLA-4 (cytotoxic T lymphocyte-associated antigen 4) on the T-cell surface. CTLA-4 acts as a "brake" on T-cell activity, blocking the CTLA-4 receptor and potentiating T-cell activation.
Previous data on gp100, mostly out of NIH research, have been limited but strongly suggested that the vaccine is most likely inactive, Dr. Cranmer pointed out. The vaccine "can induce immune responses [but] that doesn't mean that the immune response is clinically relevant. It can cure mice but it may not help people. So if it does have activity, it's not likely to have that much activity," he said.
Dr. Agarwala suggested that the vaccine in this case may have been acting like a placebo, but what if it was worse than placebo, he asked. "What if [the vaccine] was driving higher death rate? It wouldn't surprise me that the vaccine was ineffective but I don't think it was detrimental based upon the data presented. The fact that [the vaccine] arms were no better than ipilimumab alone tells me that the vaccine was likely worthless. . .that's something that needs to be teased out."
Ipilimumab's future prospects
"Ipilimumab represents the new class of T-cell potentiators and an important advance in the field of immuno-oncology," Dr. O'Day said. The drug is currently being looked at in other disease states such as lung and prostate cancer, with an eye toward finding alternative combinations and refining dosing. The matter of dosing still needs to be addressed. Dr. Agarwala pointed out that other trials have used a 10 mg/kg dose, including a trial that compared 10 mg/kg to 3 mg/kg. "Even though it wasn't powered to offer definitive answers about dosing, it did suggest that 10 mg/kg was better than 3 mg/kg" (Clin Cancer Res 16:2861-2871, 2010), he said. For Dr. Wargo, the study results "spark the question of combining nonspecific forms of immunotherapy or other forms of therapy (ie, targeted therapy) to enhance response rates" (see "BRAF inhibition may enhance immunotherapy in melanoma" on Dr. Wargo's research).

"Immunotherapy may be part of the solution...but it may not be the 'be all and end all' for melanoma therapy" - LEE CRANMER, MD, PHD
The rather homogenous study results are not the "Holy Grail" that melanoma experts are perpetually searching for, Dr. Cranmer said. "Progression-free survival (PFS) in all three arms was basically the same: about three months. The median survival in the ipilimumab-containing arms was 10 months vs six months for the gp100-alone arm. So the gp100 survival data were basically what I would expect for an inactive agent and that's no better than what we've [currently] got," Dr. Cranmer said. No doubt the latest results are a boon to developers Bristol-Myers Squibb and Medarex, which put the brakes on a Biologics License Application (BLA) submission for ipilimumab in 2008 after the FDA requested additional OS data. As of June 2010, Bristol-Myers Squibb was in the process of finalizing an updated application to the FDA.
"I'm sure this drug will get approved," Dr. Agarwala said. "There's no arguing with the fact that there was a survival improvement. The issues that have been raised with these results are not enough to negate the data." He added that results from this single trial will change the treatment paradigm, given how long melanoma specialists have waited for positive news.
Visit the
Oncology News International
online archives for more on melanoma:
Radiation Rx prevents melanoma's invasion of lymph nodes
Apoptosis inducer hits melanoma with double whammy
"There is hope in the melanoma treatment community that some form of immunotherapy can have an effect on this disease, and this [study] demonstrates that in fact there is something to that argument," Dr. Cranmer said. "Immunotherapy may be part of the solution to the melanoma problem, but it may not be the 'be all and end all' for melanoma therapy."
Additional reporting by Fran Lowry and Kathlyn Stone.